Tuesday Poster Session
Category: Biliary/Pancreas
P4385 - Type 1 Autoimmune Pancreatitis in a Teenager With Ulcerative Colitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Jerry H. Rose, MD (he/him/his)
University of Maryland Medical System
Baltimore, CA
Presenting Author(s)
Jerry H. Rose, MD1, Michael J. Sikorski, MD, PhD2, Patrick W. Ruane, DO2, Dania Hudhud, MD2, Abdulhameed M. Al-Sabban, MBBS3
1University of Maryland Medical System, Baltimore, MD; 2University of Maryland School of Medicine, Baltimore, MD; 3UNIVERSITY OF MARYLAND School of Medicine, Baltimore, MD
Introduction: Type 2 autoimmune pancreatitis (AIP) is a recognized complication of ulcerative colitis (UC), whereas Type 1 AIP—an IgG4-related sclerosing pancreatitis—is uncommon in this patient population and typically presents in older males. We present a case of recurrent pancreatitis in an 18-year-old male with UC. Investigations revealed elevated IgG4 levels and images demonstrating diffuse pancreatic strictures and parenchymal enlargement, consistent with Type 1 AIP. The patient showed a favorable response to glucocorticoid therapy. This case highlights a potential new association between AIP and UC and emphasizes early recognition and treatment.
Case Description/
Methods: An 18-year-old male with a history of biopsy-confirmed UC proctitis diagnosed six months prior, treated with oral and rectal mesalamine, and in endoscopic remission, presented with severe epigastric pain for three days. His symptoms began one month prior and were described as intermittent, “stabbing or throbbing”, non-radiating, and worse with eating, leading to fatigue and a 10-pound weight loss.
On our examination, he appeared underweight with a body mass index of 17.7 kg/m2 (2nd percentile). Abdominal palpation elicited epigastric and generalized abdominal tenderness. Laboratory evaluation showed elevated serum lipase (5573 U/L, reference range 23-300 U/L) and serum IgG4 (2430 mg/dL, reference range of 4.0-86.0 mg/dL). MRCP revealed features suggestive of acute pancreatitis involving the distal body and tail. There was an irregular pancreatic duct narrowing at the tail, and a dilated main pancreatic duct with abrupt cutoff at the head (Figure 1A). Global parenchymal enlargement resulted in a “sausage-shaped” pancreas (Figure 2A). No gallstones were identified on cross-sectional imaging. Prior MRCP studies were unavailable for comparison.
The patient tolerated a diet and was discharged the following day on prednisone 40 mg daily x2 weeks, followed by a slow taper over 7 additional weeks. 3 weeks after discharge, repeat MRCP showed no evidence of acute pancreatitis (Figure 1B and 2B). He continues maintenance on low-dose prednisone 2.5 mg daily. Pancreatitis has not recurred in 8 months, post-hospitalization.
Discussion: The case presented highlights a unique association of Type 1 AIP that developed in the setting of ulcerative colitis. Narrow definitions of autoimmune conditions may not be appropriate. Given the overlap of AIP subtypes, a broad differential for new pancreatitis in UC patients should include IgG4 levels.
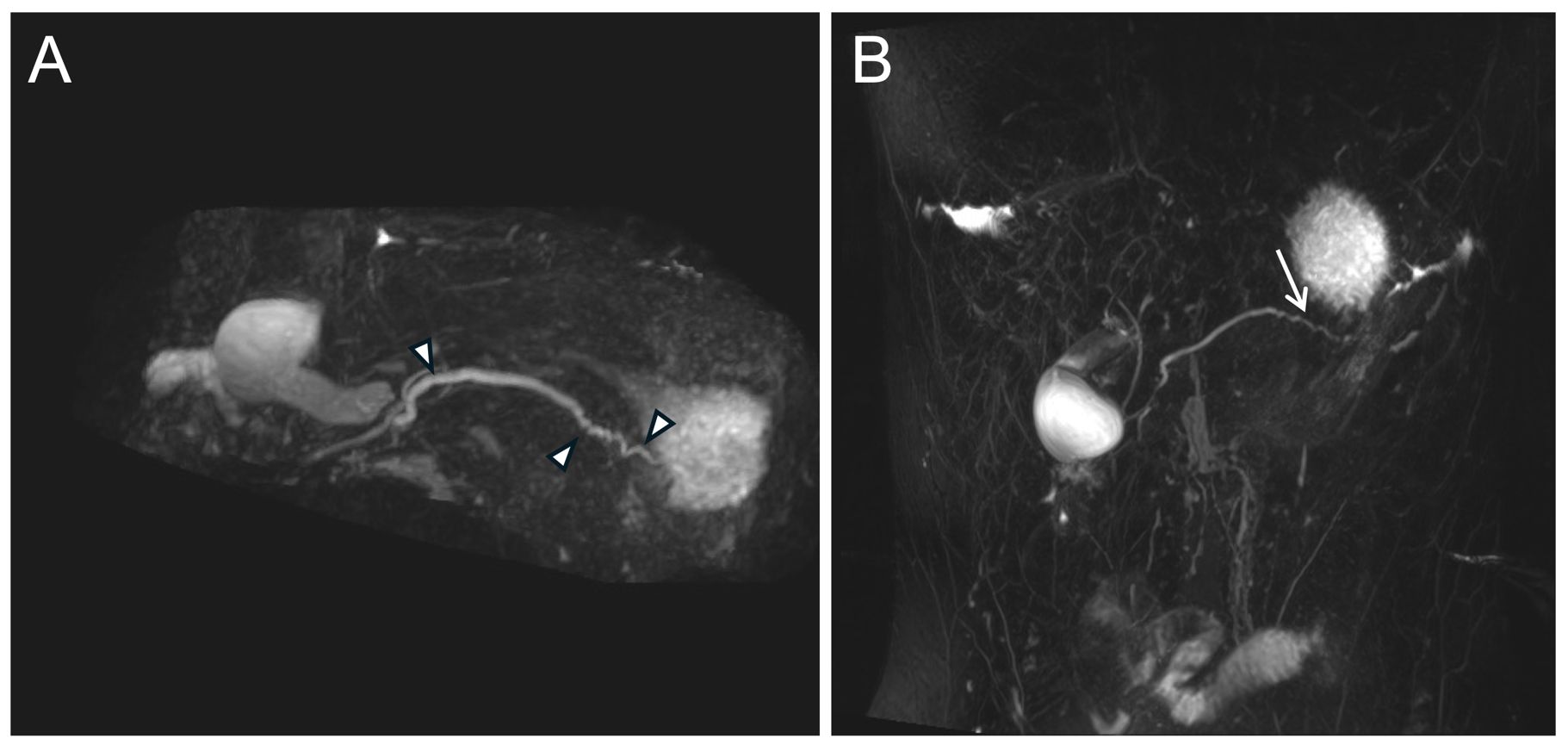
Figure: Magnetic Resonance Cholangiopancreatography obtained (A) before and (B) after steroid therapy reveals a reversal of pancreatic duct narrowing. Figure 1A: Arrowheads point to strictures throughout the pancreatic duct. Figure 1B: The arrow points to the normal pancreatic duct appearance at the tail.
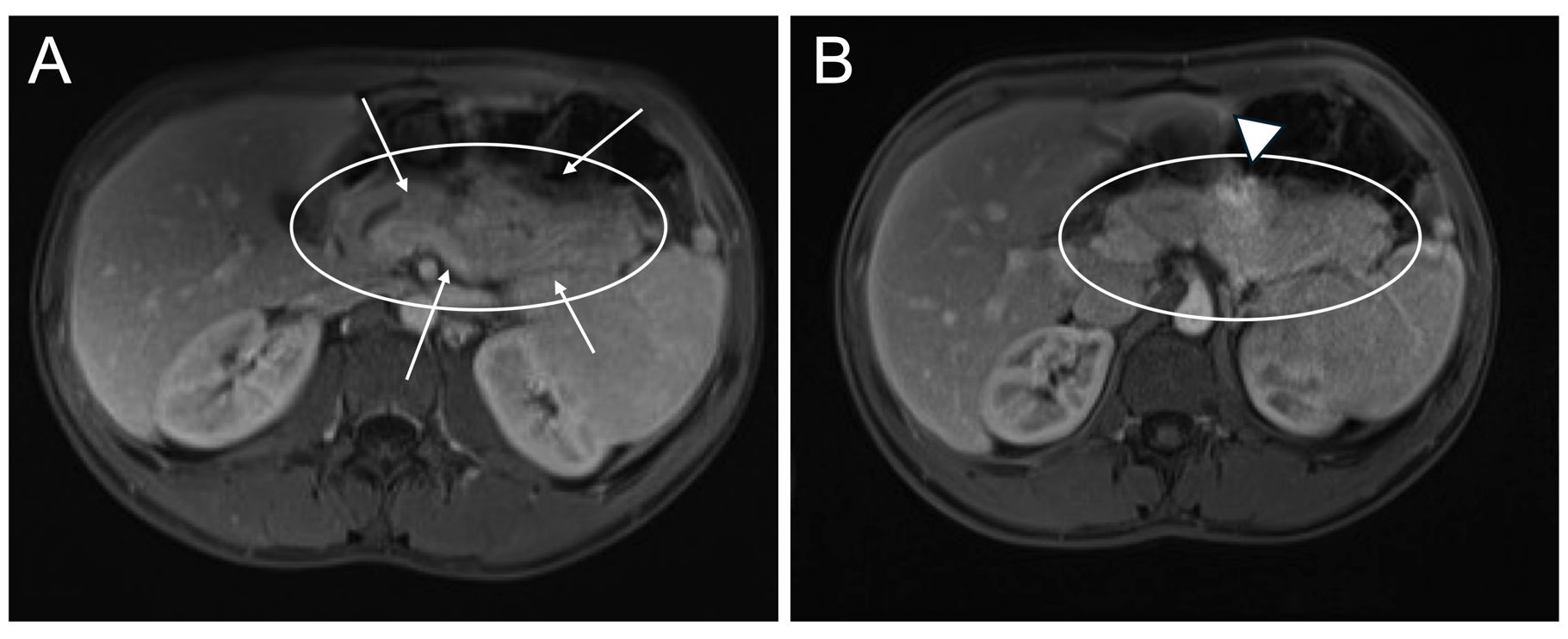
Figure: Figure 2. Magnetic resonance imaging of the abdomen obtained (A) before and (B) after steroid therapy reveals interval atrophy of the gland with resolution of the peripancreatic hypodense rim. Circles outline the pancreas. Arrows point to diffuse parenchymal swelling (sausage-shaped pancreas), which persists. Arrowhead points to focal inflammatory mass.
Disclosures:
Jerry Rose indicated no relevant financial relationships.
Michael Sikorski indicated no relevant financial relationships.
Patrick Ruane indicated no relevant financial relationships.
Dania Hudhud indicated no relevant financial relationships.
Abdulhameed Al-Sabban indicated no relevant financial relationships.
Jerry H. Rose, MD1, Michael J. Sikorski, MD, PhD2, Patrick W. Ruane, DO2, Dania Hudhud, MD2, Abdulhameed M. Al-Sabban, MBBS3. P4385 - Type 1 Autoimmune Pancreatitis in a Teenager With Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Maryland Medical System, Baltimore, MD; 2University of Maryland School of Medicine, Baltimore, MD; 3UNIVERSITY OF MARYLAND School of Medicine, Baltimore, MD
Introduction: Type 2 autoimmune pancreatitis (AIP) is a recognized complication of ulcerative colitis (UC), whereas Type 1 AIP—an IgG4-related sclerosing pancreatitis—is uncommon in this patient population and typically presents in older males. We present a case of recurrent pancreatitis in an 18-year-old male with UC. Investigations revealed elevated IgG4 levels and images demonstrating diffuse pancreatic strictures and parenchymal enlargement, consistent with Type 1 AIP. The patient showed a favorable response to glucocorticoid therapy. This case highlights a potential new association between AIP and UC and emphasizes early recognition and treatment.
Case Description/
Methods: An 18-year-old male with a history of biopsy-confirmed UC proctitis diagnosed six months prior, treated with oral and rectal mesalamine, and in endoscopic remission, presented with severe epigastric pain for three days. His symptoms began one month prior and were described as intermittent, “stabbing or throbbing”, non-radiating, and worse with eating, leading to fatigue and a 10-pound weight loss.
On our examination, he appeared underweight with a body mass index of 17.7 kg/m2 (2nd percentile). Abdominal palpation elicited epigastric and generalized abdominal tenderness. Laboratory evaluation showed elevated serum lipase (5573 U/L, reference range 23-300 U/L) and serum IgG4 (2430 mg/dL, reference range of 4.0-86.0 mg/dL). MRCP revealed features suggestive of acute pancreatitis involving the distal body and tail. There was an irregular pancreatic duct narrowing at the tail, and a dilated main pancreatic duct with abrupt cutoff at the head (Figure 1A). Global parenchymal enlargement resulted in a “sausage-shaped” pancreas (Figure 2A). No gallstones were identified on cross-sectional imaging. Prior MRCP studies were unavailable for comparison.
The patient tolerated a diet and was discharged the following day on prednisone 40 mg daily x2 weeks, followed by a slow taper over 7 additional weeks. 3 weeks after discharge, repeat MRCP showed no evidence of acute pancreatitis (Figure 1B and 2B). He continues maintenance on low-dose prednisone 2.5 mg daily. Pancreatitis has not recurred in 8 months, post-hospitalization.
Discussion: The case presented highlights a unique association of Type 1 AIP that developed in the setting of ulcerative colitis. Narrow definitions of autoimmune conditions may not be appropriate. Given the overlap of AIP subtypes, a broad differential for new pancreatitis in UC patients should include IgG4 levels.
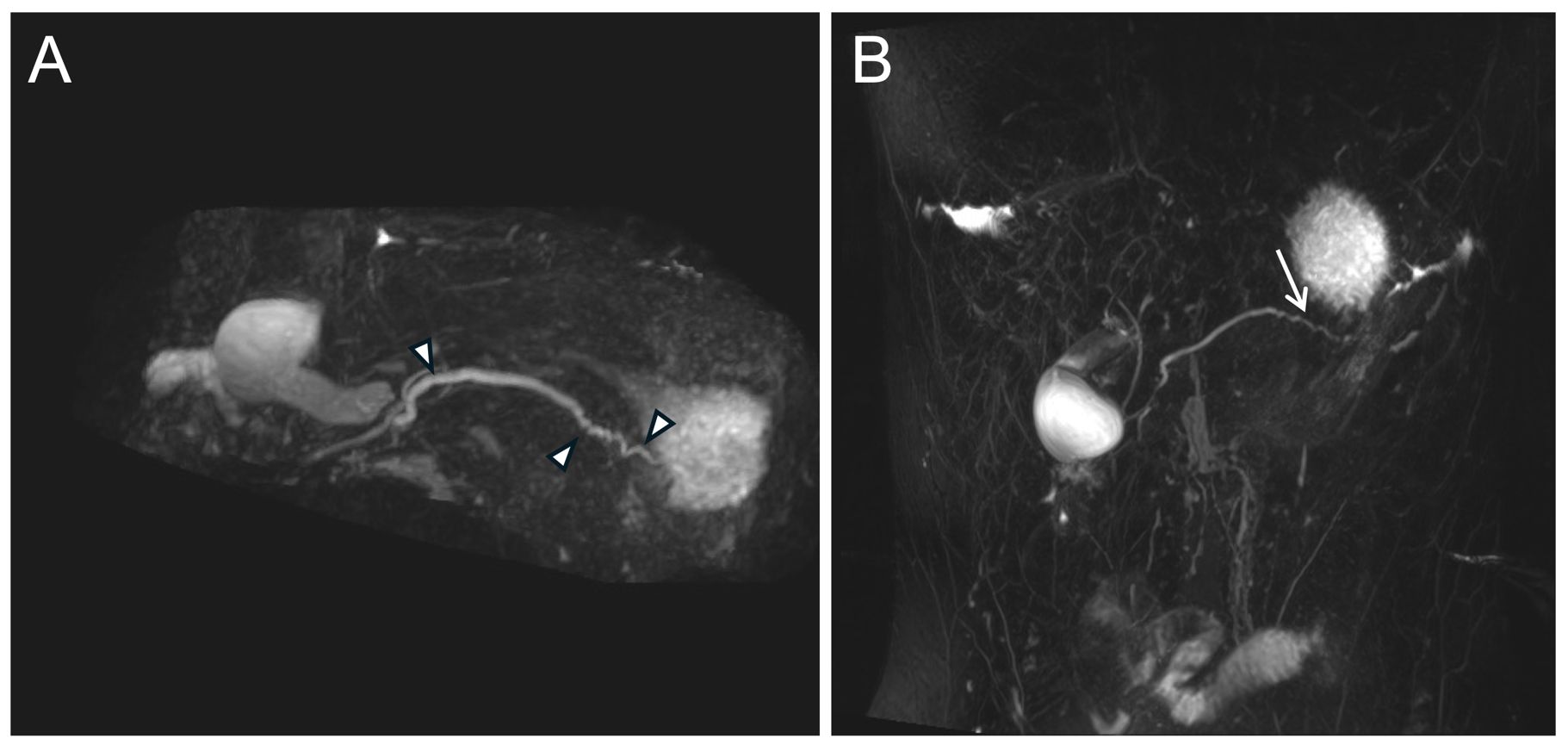
Figure: Magnetic Resonance Cholangiopancreatography obtained (A) before and (B) after steroid therapy reveals a reversal of pancreatic duct narrowing. Figure 1A: Arrowheads point to strictures throughout the pancreatic duct. Figure 1B: The arrow points to the normal pancreatic duct appearance at the tail.
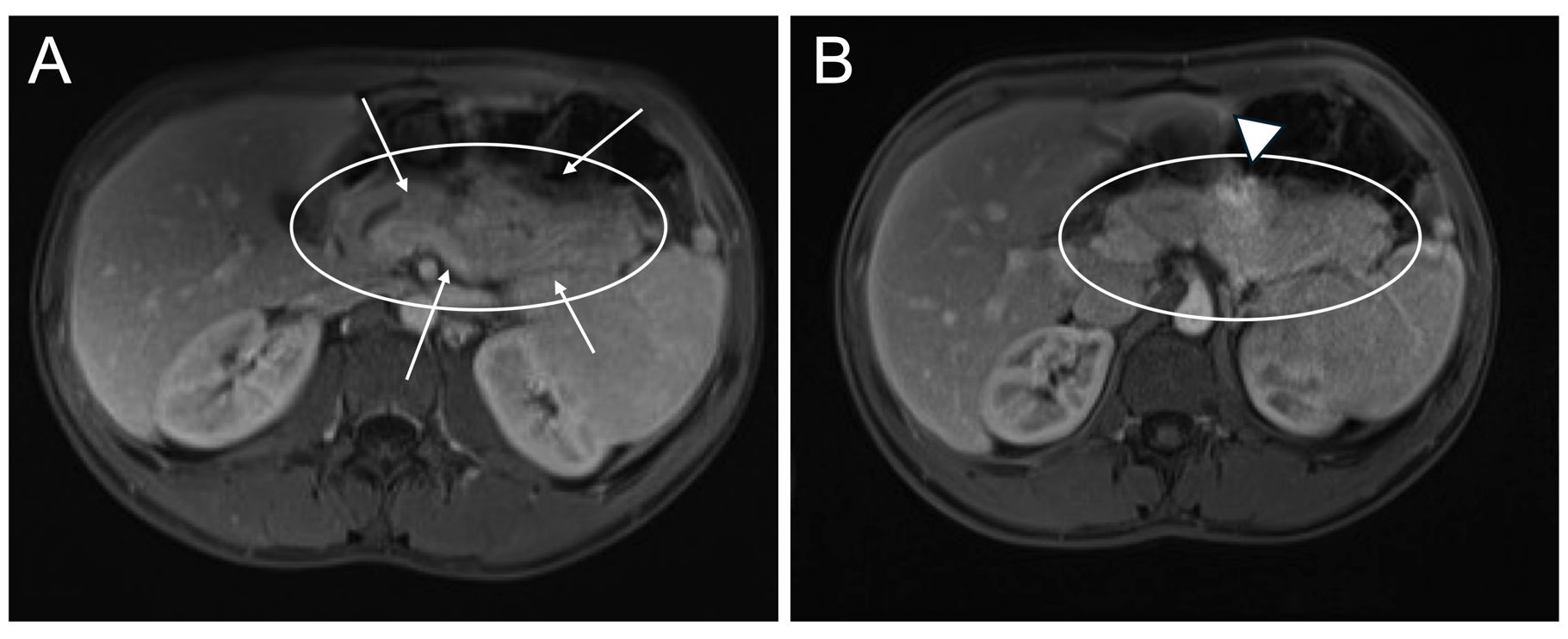
Figure: Figure 2. Magnetic resonance imaging of the abdomen obtained (A) before and (B) after steroid therapy reveals interval atrophy of the gland with resolution of the peripancreatic hypodense rim. Circles outline the pancreas. Arrows point to diffuse parenchymal swelling (sausage-shaped pancreas), which persists. Arrowhead points to focal inflammatory mass.
Disclosures:
Jerry Rose indicated no relevant financial relationships.
Michael Sikorski indicated no relevant financial relationships.
Patrick Ruane indicated no relevant financial relationships.
Dania Hudhud indicated no relevant financial relationships.
Abdulhameed Al-Sabban indicated no relevant financial relationships.
Jerry H. Rose, MD1, Michael J. Sikorski, MD, PhD2, Patrick W. Ruane, DO2, Dania Hudhud, MD2, Abdulhameed M. Al-Sabban, MBBS3. P4385 - Type 1 Autoimmune Pancreatitis in a Teenager With Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
