Tuesday Poster Session
Category: Biliary/Pancreas
P4373 - Unmasking the Impact of Alcohol Withdrawal in Acute Pancreatitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Manasa Ginjupalli, MD
Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
Manasa Ginjupalli, MD1, Camelia Ciobanu, MD1, Chaula Desai, MD1, Arnold Forlemu, MD1, Hima Varsha Voruganti, MD2, Vikash Kumar, MD3, Madhavi Reddy, MD4
1Brooklyn Hospital Center, Brooklyn, NY; 2North Alabama Medical Center, Florence, AL; 3Creighton University School of Medicine, Phoenix, AZ; 4The Brooklyn Hospital Center, Brooklyn, NY
Introduction: Alcohol use is an established and major cause of acute pancreatitis. However, there was a hypothesis that acute pancreatitis might be a manifestation of alcohol withdrawal, in long term alcohol users with sudden cessation. Withdrawal may exacerbate inflammation via disrupted calcium signaling, oxidative stress, and impaired autophagy triggering episodes of acute pancreatitis and ongoing inflammation could lead to worse. In this study, we tried to explore the effects of alcohol withdrawal on outcomes of acute pancreatitis.
Methods: We conducted a retrospective cohort study using the National Inpatient Sample database (2018–2022). Patients ≥18 years with a principal AAP diagnosis were identified by ICD-10 codes and stratified by presence of alcohol withdrawal during the admission. The primary outcome was in-hospital mortality; secondary outcomes included resource use and AAP complications. Categorical variables were compared with chi-square tests, continuous variables with t-tests. Multivariable logistic and linear regressions adjusted for demographics, hospital characteristics, and comorbidities.
Results: Among 498,680 AAP hospitalizations, 27.9% involved alcohol withdrawal. The majority of patients were male in both groups (72% with withdrawal vs. 67% without). Demographic characteristics were comparable between the two cohorts. The in-hospital mortality rate was slightly higher with withdrawal (1.5%) compared to without (1.1%); however, this difference was not statistically significant after multivariable adjustment (OR 1.13; p > 0.05).
Alcohol withdrawal was significantly associated with increased odds of sepsis, septic shock, acute renal failure, acute respiratory distress syndrome and the need for mechanical ventilation (Table). Additionally, alcohol withdrawal correlated with increased resource utilization, evidenced by a prolonged hospital stay of 2.17 days and an average increase in hospital charges of $24,362.
Discussion: Our study shows that alcohol withdrawal during AAP hospitalizations is associated with heightened mortality and morbidity burden. While chronic alcohol intake is generally considered a proinflammatory state, sudden cessation could exacerbate the inflammation, lead to autophagy and release of pancreatic enzymes leading to AAP. These findings underscore the importance of early identification and management of alcohol withdrawal. Implementing standardized screening protocols and withdrawal management regimens may help mitigate adverse outcomes.
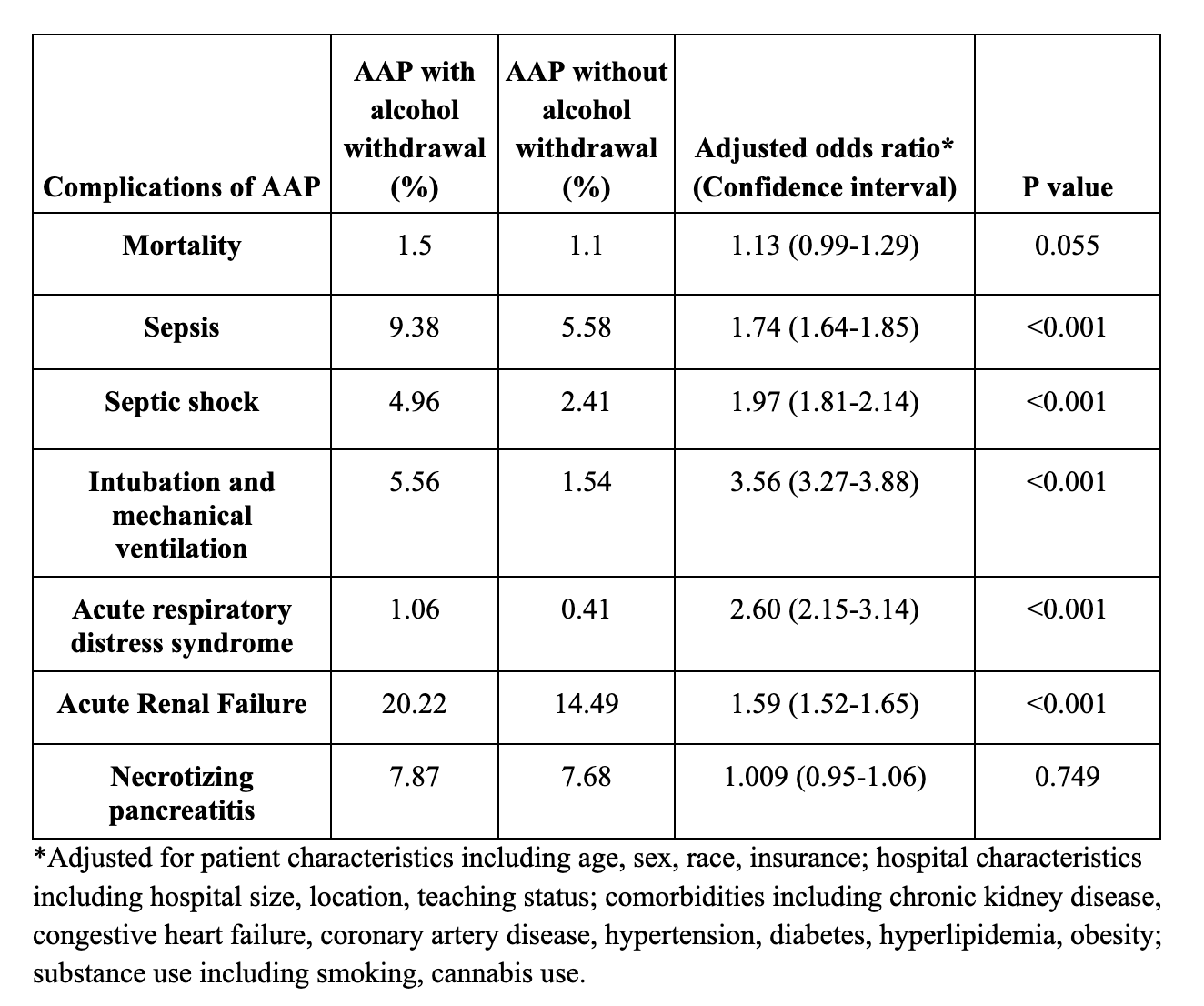
Figure: Table: Comparison of Acute alcoholic pancreatitis hospitalization outcomes with and without alcohol withdrawal
Disclosures:
Manasa Ginjupalli indicated no relevant financial relationships.
Camelia Ciobanu indicated no relevant financial relationships.
Chaula Desai indicated no relevant financial relationships.
Arnold Forlemu indicated no relevant financial relationships.
Hima Varsha Voruganti indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Madhavi Reddy indicated no relevant financial relationships.
Manasa Ginjupalli, MD1, Camelia Ciobanu, MD1, Chaula Desai, MD1, Arnold Forlemu, MD1, Hima Varsha Voruganti, MD2, Vikash Kumar, MD3, Madhavi Reddy, MD4. P4373 - Unmasking the Impact of Alcohol Withdrawal in Acute Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Brooklyn Hospital Center, Brooklyn, NY; 2North Alabama Medical Center, Florence, AL; 3Creighton University School of Medicine, Phoenix, AZ; 4The Brooklyn Hospital Center, Brooklyn, NY
Introduction: Alcohol use is an established and major cause of acute pancreatitis. However, there was a hypothesis that acute pancreatitis might be a manifestation of alcohol withdrawal, in long term alcohol users with sudden cessation. Withdrawal may exacerbate inflammation via disrupted calcium signaling, oxidative stress, and impaired autophagy triggering episodes of acute pancreatitis and ongoing inflammation could lead to worse. In this study, we tried to explore the effects of alcohol withdrawal on outcomes of acute pancreatitis.
Methods: We conducted a retrospective cohort study using the National Inpatient Sample database (2018–2022). Patients ≥18 years with a principal AAP diagnosis were identified by ICD-10 codes and stratified by presence of alcohol withdrawal during the admission. The primary outcome was in-hospital mortality; secondary outcomes included resource use and AAP complications. Categorical variables were compared with chi-square tests, continuous variables with t-tests. Multivariable logistic and linear regressions adjusted for demographics, hospital characteristics, and comorbidities.
Results: Among 498,680 AAP hospitalizations, 27.9% involved alcohol withdrawal. The majority of patients were male in both groups (72% with withdrawal vs. 67% without). Demographic characteristics were comparable between the two cohorts. The in-hospital mortality rate was slightly higher with withdrawal (1.5%) compared to without (1.1%); however, this difference was not statistically significant after multivariable adjustment (OR 1.13; p > 0.05).
Alcohol withdrawal was significantly associated with increased odds of sepsis, septic shock, acute renal failure, acute respiratory distress syndrome and the need for mechanical ventilation (Table). Additionally, alcohol withdrawal correlated with increased resource utilization, evidenced by a prolonged hospital stay of 2.17 days and an average increase in hospital charges of $24,362.
Discussion: Our study shows that alcohol withdrawal during AAP hospitalizations is associated with heightened mortality and morbidity burden. While chronic alcohol intake is generally considered a proinflammatory state, sudden cessation could exacerbate the inflammation, lead to autophagy and release of pancreatic enzymes leading to AAP. These findings underscore the importance of early identification and management of alcohol withdrawal. Implementing standardized screening protocols and withdrawal management regimens may help mitigate adverse outcomes.
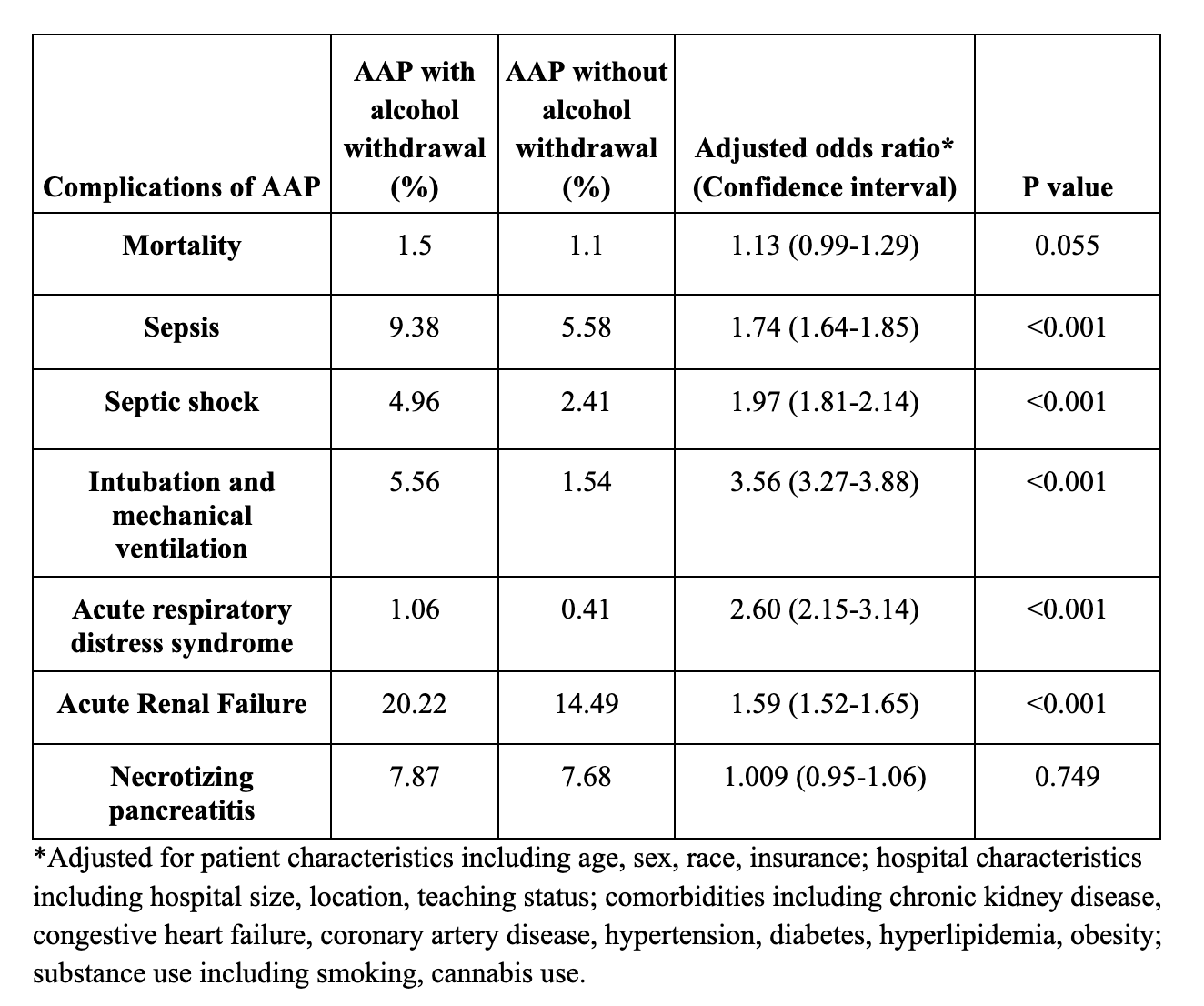
Figure: Table: Comparison of Acute alcoholic pancreatitis hospitalization outcomes with and without alcohol withdrawal
Disclosures:
Manasa Ginjupalli indicated no relevant financial relationships.
Camelia Ciobanu indicated no relevant financial relationships.
Chaula Desai indicated no relevant financial relationships.
Arnold Forlemu indicated no relevant financial relationships.
Hima Varsha Voruganti indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Madhavi Reddy indicated no relevant financial relationships.
Manasa Ginjupalli, MD1, Camelia Ciobanu, MD1, Chaula Desai, MD1, Arnold Forlemu, MD1, Hima Varsha Voruganti, MD2, Vikash Kumar, MD3, Madhavi Reddy, MD4. P4373 - Unmasking the Impact of Alcohol Withdrawal in Acute Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
