Tuesday Poster Session
Category: Biliary/Pancreas
P4369 - Early Prognostic Scoring and Outcomes in Acute Pancreatitis: Ambispective Analysis of a Large Indian Cohort
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Mipasha Patel, MD
Abington Jefferson Hospital
Willow Grove, PA
Presenting Author(s)
Mipasha Patel, MD1, Samir Vanani, MBBS2, Dhvani Adhvaryu, PharmD2, Nishtha Nandwani, MBBS2, Aarya Desai, BSc2, Dhiraaj Desai, BE2, Rajiv Mehta, MD, DNB2
1Abington Jefferson Hospital, Willow Grove, PA; 2Surat Institute of Digestive Sciences Hospital, Surat, Gujarat, India
Introduction: Acute pancreatitis (AP) is a common and potentially severe inflammatory condition with rising global incidence. In India, data on predictors of severity and mortality remain limited. This study aimed to assess early predictors of adverse outcomes, including BISAP score and C-reactive protein (CRP), and explore the impact of etiology and demographics on clinical course and complications.
Methods: We ambispectively analyzed 1,250 patients with AP admitted to a tertiary care center in India from 2018 to 2025. Diagnosis was based on Revised Atlanta Criteria. Data were extracted from electronic medical records. BISAP score at admission and CRP at 48 hours were evaluated as predictors of in-hospital mortality, pancreatic necrosis, and persistent organ failure. Logistic regression and ROC curve analyses were used to assess associations and predictive accuracy.
Results: The median age was 41 years with 74% males. Etiologies included idiopathic (36%), biliary (35.4%), alcoholic (19.9%), and hypertriglyceridemia (5.3%) and other (3.4%). Overall, 61% were mild, while 14% were severe cases. Overall mortality was 5.7%, pancreatic necrosis occurred in 28.6% and organ failure in 18.4%. BISAP score and CRP were strong predictors of adverse outcomes. On multivariate analysis, each BISAP point increase was associated with higher odds of mortality (aOR 6.52), and each 10 mg/L rise in CRP increased mortality risk (aOR 1.24). BISAP and CRP also predicted necrosis and organ failure independently. Additionally, age and alcoholic etiology were independently associated with necrosis, even after adjustment. ROC curves showed BISAP had excellent discrimination for mortality (AUC 0.95), superior to CRP (AUC 0.73). Combining both marginally improved prediction (AUC 0.96). While alcoholic AP was linked to worse outcomes, etiology, age, and sex were not independent predictors of mortality after adjustment.
Discussion: This large Indian cohort confirms BISAP as a robust early risk stratification tool in AP, outperforming CRP for mortality prediction. CRP remains a useful adjunct for anticipating complications. Notably, age and etiology were independently associated with necrosis, suggesting that host factors and disease mechanism contribute to local complications. Alcoholic AP was more frequently associated with necrosis and organ failure, emphasizing the need for preventive strategies. These findings support the routine use of BISAP and CRP for timely risk stratification, especially in resource-limited settings.
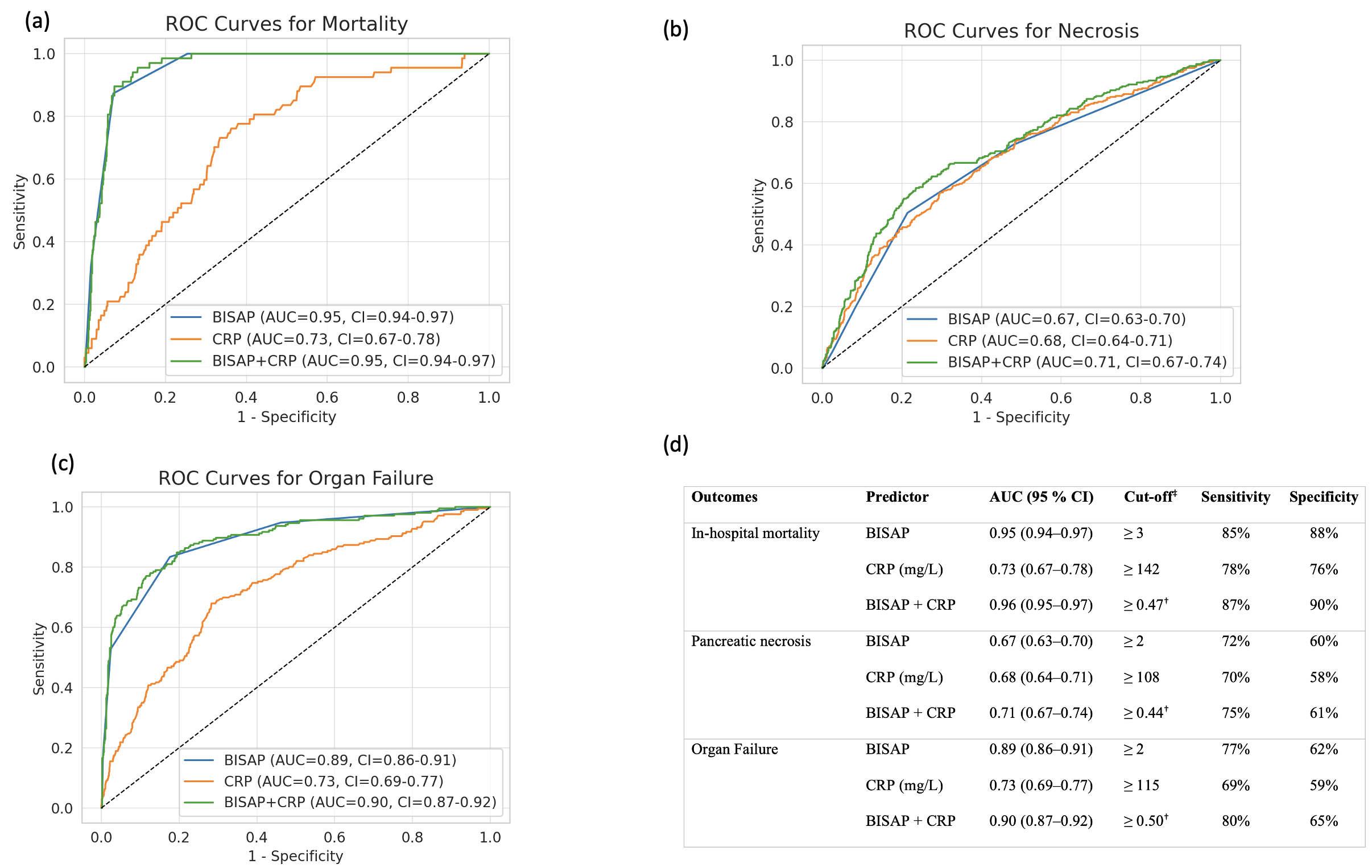
Figure: Multivariable logistic regression showing independent predictors of mortality, pancreatic necrosis, and organ failure.
aOR: adjusted odds ratio; CI: confidence interval; BISAP: bedside index of severity in acute pancreatitis; CRP: C-reactive protein.
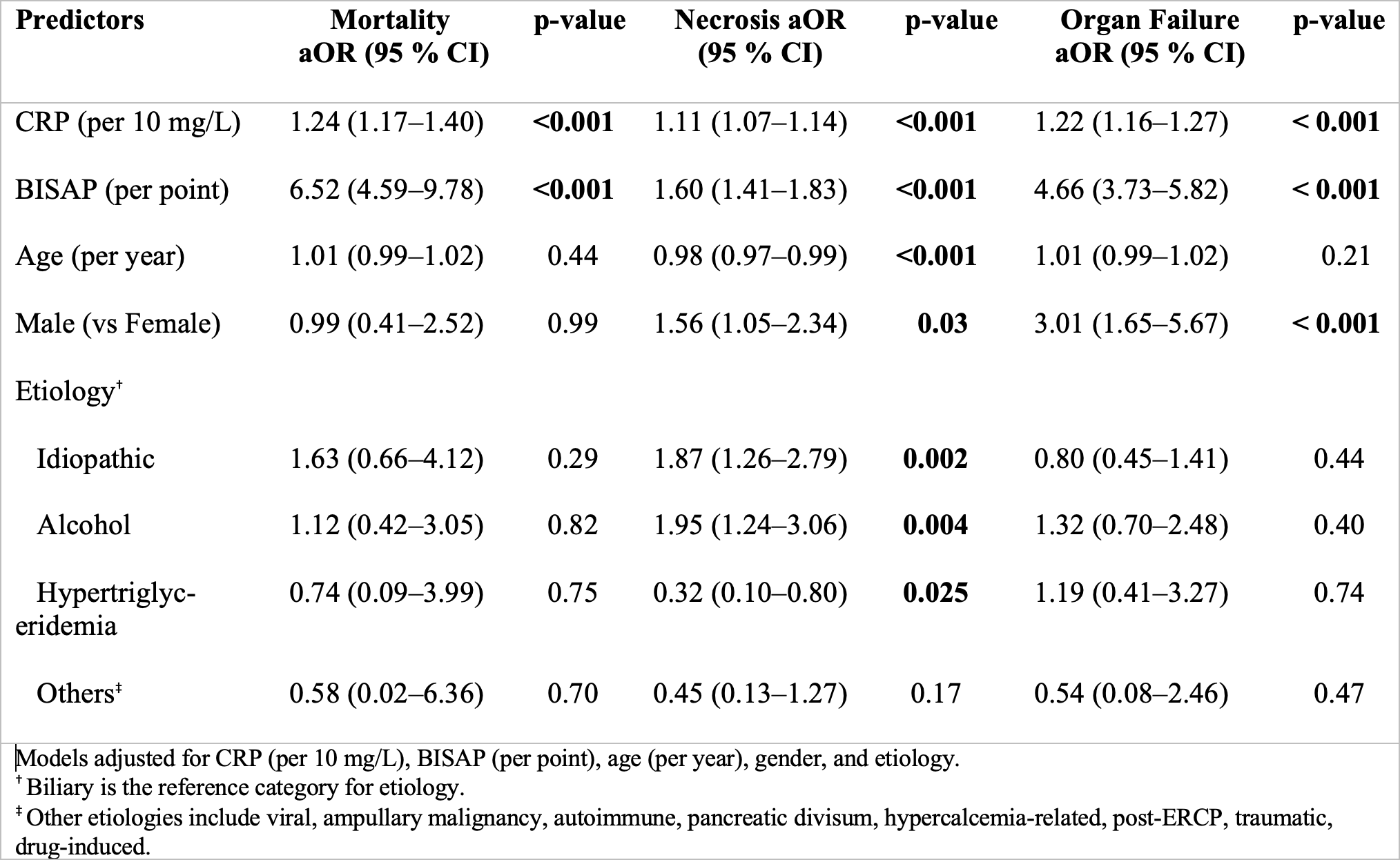
Figure: Combined ROC curves and diagnostic performance of BISAP, CRP, and BISAP+CRP models for predicting mortality (a), pancreatic necrosis (b), and organ failure (c) in acute pancreatitis. Table (d) summarizes AUC, optimal cut-offs, sensitivity, and specificity.
AUC: Area under the curve; CRP: C-reactive protein; BISAP: Bedside Index of Severity in Acute Pancreatitis.
Disclosures:
Mipasha Patel indicated no relevant financial relationships.
Samir Vanani indicated no relevant financial relationships.
Dhvani Adhvaryu indicated no relevant financial relationships.
Nishtha Nandwani indicated no relevant financial relationships.
Aarya Desai indicated no relevant financial relationships.
Dhiraaj Desai indicated no relevant financial relationships.
Rajiv Mehta indicated no relevant financial relationships.
Mipasha Patel, MD1, Samir Vanani, MBBS2, Dhvani Adhvaryu, PharmD2, Nishtha Nandwani, MBBS2, Aarya Desai, BSc2, Dhiraaj Desai, BE2, Rajiv Mehta, MD, DNB2. P4369 - Early Prognostic Scoring and Outcomes in Acute Pancreatitis: Ambispective Analysis of a Large Indian Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Abington Jefferson Hospital, Willow Grove, PA; 2Surat Institute of Digestive Sciences Hospital, Surat, Gujarat, India
Introduction: Acute pancreatitis (AP) is a common and potentially severe inflammatory condition with rising global incidence. In India, data on predictors of severity and mortality remain limited. This study aimed to assess early predictors of adverse outcomes, including BISAP score and C-reactive protein (CRP), and explore the impact of etiology and demographics on clinical course and complications.
Methods: We ambispectively analyzed 1,250 patients with AP admitted to a tertiary care center in India from 2018 to 2025. Diagnosis was based on Revised Atlanta Criteria. Data were extracted from electronic medical records. BISAP score at admission and CRP at 48 hours were evaluated as predictors of in-hospital mortality, pancreatic necrosis, and persistent organ failure. Logistic regression and ROC curve analyses were used to assess associations and predictive accuracy.
Results: The median age was 41 years with 74% males. Etiologies included idiopathic (36%), biliary (35.4%), alcoholic (19.9%), and hypertriglyceridemia (5.3%) and other (3.4%). Overall, 61% were mild, while 14% were severe cases. Overall mortality was 5.7%, pancreatic necrosis occurred in 28.6% and organ failure in 18.4%. BISAP score and CRP were strong predictors of adverse outcomes. On multivariate analysis, each BISAP point increase was associated with higher odds of mortality (aOR 6.52), and each 10 mg/L rise in CRP increased mortality risk (aOR 1.24). BISAP and CRP also predicted necrosis and organ failure independently. Additionally, age and alcoholic etiology were independently associated with necrosis, even after adjustment. ROC curves showed BISAP had excellent discrimination for mortality (AUC 0.95), superior to CRP (AUC 0.73). Combining both marginally improved prediction (AUC 0.96). While alcoholic AP was linked to worse outcomes, etiology, age, and sex were not independent predictors of mortality after adjustment.
Discussion: This large Indian cohort confirms BISAP as a robust early risk stratification tool in AP, outperforming CRP for mortality prediction. CRP remains a useful adjunct for anticipating complications. Notably, age and etiology were independently associated with necrosis, suggesting that host factors and disease mechanism contribute to local complications. Alcoholic AP was more frequently associated with necrosis and organ failure, emphasizing the need for preventive strategies. These findings support the routine use of BISAP and CRP for timely risk stratification, especially in resource-limited settings.
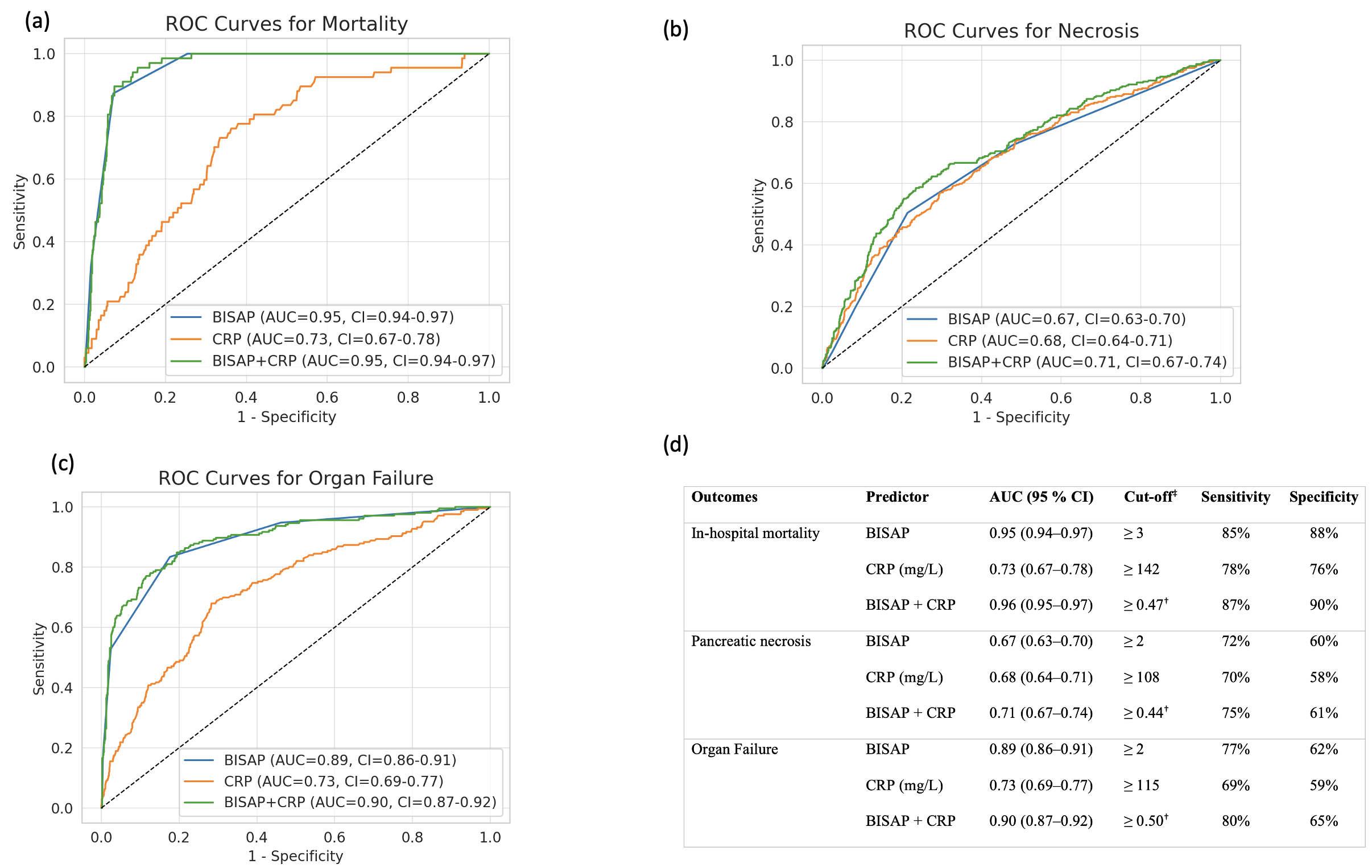
Figure: Multivariable logistic regression showing independent predictors of mortality, pancreatic necrosis, and organ failure.
aOR: adjusted odds ratio; CI: confidence interval; BISAP: bedside index of severity in acute pancreatitis; CRP: C-reactive protein.
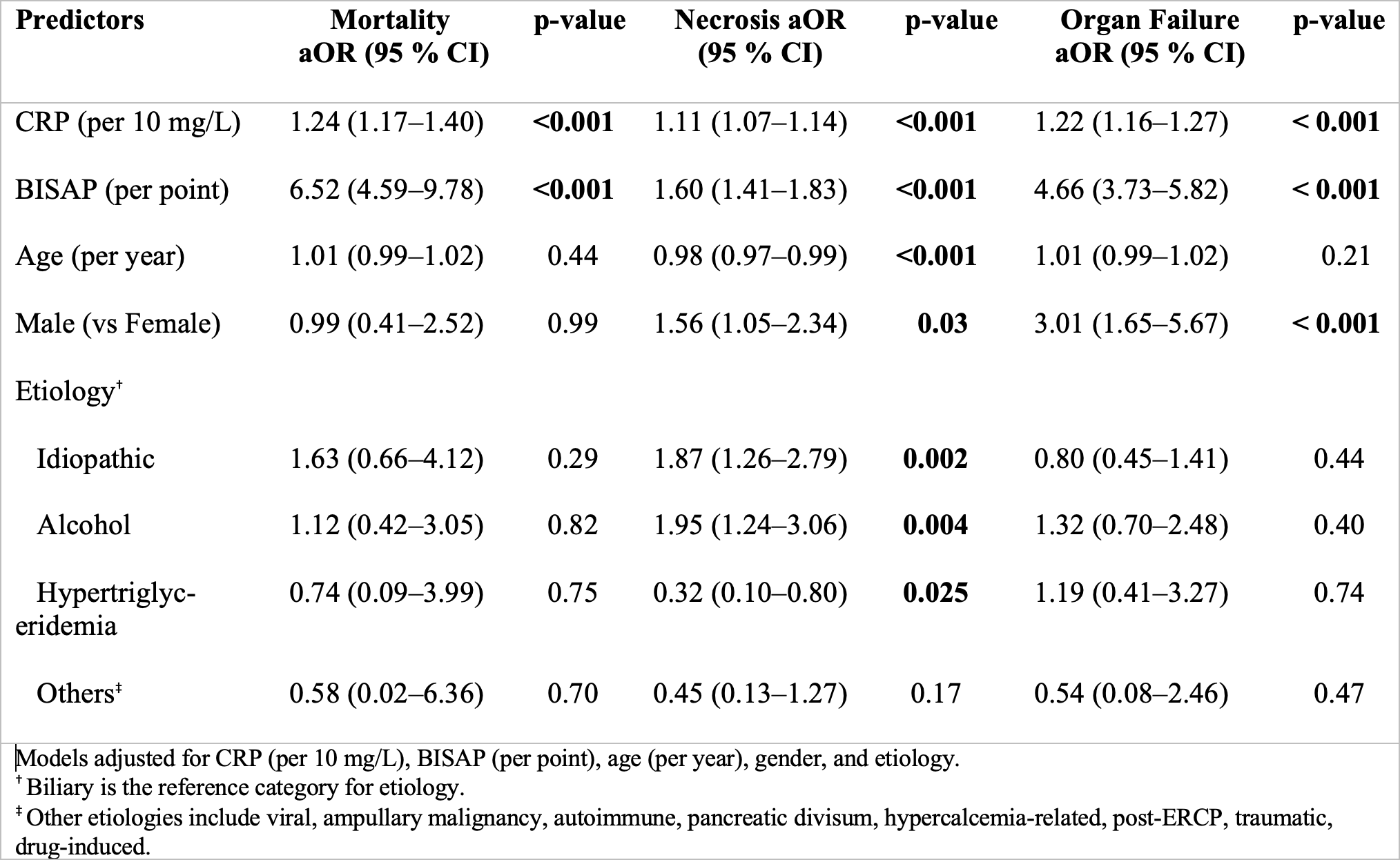
Figure: Combined ROC curves and diagnostic performance of BISAP, CRP, and BISAP+CRP models for predicting mortality (a), pancreatic necrosis (b), and organ failure (c) in acute pancreatitis. Table (d) summarizes AUC, optimal cut-offs, sensitivity, and specificity.
AUC: Area under the curve; CRP: C-reactive protein; BISAP: Bedside Index of Severity in Acute Pancreatitis.
Disclosures:
Mipasha Patel indicated no relevant financial relationships.
Samir Vanani indicated no relevant financial relationships.
Dhvani Adhvaryu indicated no relevant financial relationships.
Nishtha Nandwani indicated no relevant financial relationships.
Aarya Desai indicated no relevant financial relationships.
Dhiraaj Desai indicated no relevant financial relationships.
Rajiv Mehta indicated no relevant financial relationships.
Mipasha Patel, MD1, Samir Vanani, MBBS2, Dhvani Adhvaryu, PharmD2, Nishtha Nandwani, MBBS2, Aarya Desai, BSc2, Dhiraaj Desai, BE2, Rajiv Mehta, MD, DNB2. P4369 - Early Prognostic Scoring and Outcomes in Acute Pancreatitis: Ambispective Analysis of a Large Indian Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
