Tuesday Poster Session
Category: Biliary/Pancreas
P4361 - Decreased Risk of a Subsequent Diagnosis of Chronic Pancreatitis Following a First Acute Pancreatitis Event in Patients With DM Type 2 Taking Metformin
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Luis Lara, MD (he/him/his)
Professor and Division Director
University of Cincinnati
Cincinnati, OH
Presenting Author(s)
Luis Lara, MD1, Moamen Gabr, MD, MSc1, Rosanne Danielson, MD1, Wei-Wen Hsu, PhD1, Milton Smith, MD1, Inuk Zandvakili, MD, PhD1, Andrew Ofosu, MD, MPH2, Mitchell L. Ramsey, MD3, Maisam Abu-El-Haija, MD4, Georgios I. Papachristou, MD, PhD3
1University of Cincinnati, Cincinnati, OH; 2University of Cincinnati College of Medicine, Cincinnati, OH; 3The Ohio State University Wexner Medical Center, Columbus, OH; 4Cincinnati Children's Hospital Medical Center, Cincinnati, OH
Introduction: Subjects with diabetes mellitus (DM) have a higher risk of developing acute pancreatitis (AP) and chronic pancreatitis (CP). AP is a risk for CP, but there is currently no medication to prevent the progression to CP after an initial AP event. Metformin is regularly used to treat DM type 2. Its pleiotropic properties include anti-inflammation by NFkB inhibition directly by AMPK or indirectly by PTEN, which may modify the inflammatory cascade. We studied the effect of metformin on AP progression to CP.
Methods: The TriNetX database (Cambridge, MA) was queried from 2014-2025. Only data from the Unites States was used. Patients had to be on metformin for at least 1 year and after a first AP event they were followed over time to determine the incidence of CP in this cohort. To decrease lead-time bias the diagnosis of CP had to occur at least 3 years after the index AP event. 37 exclusion criteria including a previous history of AP, CP, pancreas surgery, smoking, alcohol use, and DM type 1 were used. AP and CP were diagnosed according to ICD-10 codes. Propensity score matching (PSM) was performed after comparing variables using Wilcoxon rank sums and Kruskal-Wallis tests. Percentages and odds ratio were reported. P< 0.001 was significant.
Results: Before matching there were 76,096 subjects with DM 2 on metformin and 1,943,565 with DM 2 not on metformin. After PSM there were 74,930 subjects in each group. 53% were females, 58% White, 17% Black, mean age 60, mean weight was 200 lbs. The incidence of a diagnosis of CP after an index AP event was significantly lower (98 patients,1.3%) for patients with DM type 2 on metformin compared to patients with DM type 2 not taking metformin (172 patients, 2.3%), OR 1.75, P< 0.0001. See table.
Discussion: We found a decreased risk of progression to CP after a first AP event in patients with DM 2 on metformin. This may be explained by inhibition of the inflammatory cascade. Our findings suggest that metformin may act as a disease modifier for the development of, or progression to, chronic pancreatitis, which needs to be further studied.
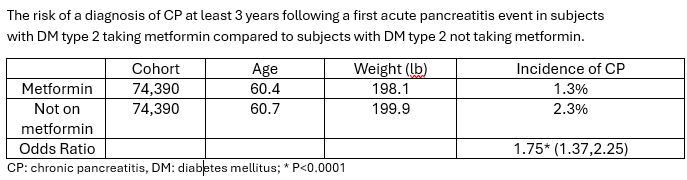
Figure: Table: The risk of a diagnosis of CP at least 3 years following a first acute pancreatitis event in subjects with DM type 2 taking metformin compared to subjects with DM type 2 not taking metformin.
Disclosures:
Luis Lara: AbbVie – Consultant, Grant/Research Support, Speakers Bureau.
Moamen Gabr indicated no relevant financial relationships.
Rosanne Danielson indicated no relevant financial relationships.
Wei-Wen Hsu indicated no relevant financial relationships.
Milton Smith indicated no relevant financial relationships.
Inuk Zandvakili: Eli Lilly – Consultant.
Andrew Ofosu indicated no relevant financial relationships.
Mitchell Ramsey indicated no relevant financial relationships.
Maisam Abu-El-Haija indicated no relevant financial relationships.
Georgios Papachristou: AbbVie – Grant/Research Support.
Luis Lara, MD1, Moamen Gabr, MD, MSc1, Rosanne Danielson, MD1, Wei-Wen Hsu, PhD1, Milton Smith, MD1, Inuk Zandvakili, MD, PhD1, Andrew Ofosu, MD, MPH2, Mitchell L. Ramsey, MD3, Maisam Abu-El-Haija, MD4, Georgios I. Papachristou, MD, PhD3. P4361 - Decreased Risk of a Subsequent Diagnosis of Chronic Pancreatitis Following a First Acute Pancreatitis Event in Patients With DM Type 2 Taking Metformin, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Cincinnati, Cincinnati, OH; 2University of Cincinnati College of Medicine, Cincinnati, OH; 3The Ohio State University Wexner Medical Center, Columbus, OH; 4Cincinnati Children's Hospital Medical Center, Cincinnati, OH
Introduction: Subjects with diabetes mellitus (DM) have a higher risk of developing acute pancreatitis (AP) and chronic pancreatitis (CP). AP is a risk for CP, but there is currently no medication to prevent the progression to CP after an initial AP event. Metformin is regularly used to treat DM type 2. Its pleiotropic properties include anti-inflammation by NFkB inhibition directly by AMPK or indirectly by PTEN, which may modify the inflammatory cascade. We studied the effect of metformin on AP progression to CP.
Methods: The TriNetX database (Cambridge, MA) was queried from 2014-2025. Only data from the Unites States was used. Patients had to be on metformin for at least 1 year and after a first AP event they were followed over time to determine the incidence of CP in this cohort. To decrease lead-time bias the diagnosis of CP had to occur at least 3 years after the index AP event. 37 exclusion criteria including a previous history of AP, CP, pancreas surgery, smoking, alcohol use, and DM type 1 were used. AP and CP were diagnosed according to ICD-10 codes. Propensity score matching (PSM) was performed after comparing variables using Wilcoxon rank sums and Kruskal-Wallis tests. Percentages and odds ratio were reported. P< 0.001 was significant.
Results: Before matching there were 76,096 subjects with DM 2 on metformin and 1,943,565 with DM 2 not on metformin. After PSM there were 74,930 subjects in each group. 53% were females, 58% White, 17% Black, mean age 60, mean weight was 200 lbs. The incidence of a diagnosis of CP after an index AP event was significantly lower (98 patients,1.3%) for patients with DM type 2 on metformin compared to patients with DM type 2 not taking metformin (172 patients, 2.3%), OR 1.75, P< 0.0001. See table.
Discussion: We found a decreased risk of progression to CP after a first AP event in patients with DM 2 on metformin. This may be explained by inhibition of the inflammatory cascade. Our findings suggest that metformin may act as a disease modifier for the development of, or progression to, chronic pancreatitis, which needs to be further studied.
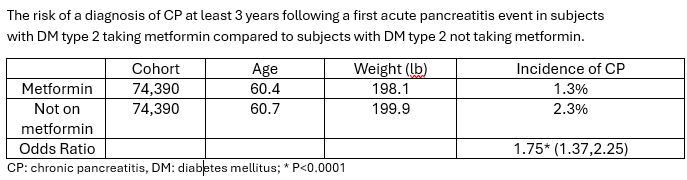
Figure: Table: The risk of a diagnosis of CP at least 3 years following a first acute pancreatitis event in subjects with DM type 2 taking metformin compared to subjects with DM type 2 not taking metformin.
Disclosures:
Luis Lara: AbbVie – Consultant, Grant/Research Support, Speakers Bureau.
Moamen Gabr indicated no relevant financial relationships.
Rosanne Danielson indicated no relevant financial relationships.
Wei-Wen Hsu indicated no relevant financial relationships.
Milton Smith indicated no relevant financial relationships.
Inuk Zandvakili: Eli Lilly – Consultant.
Andrew Ofosu indicated no relevant financial relationships.
Mitchell Ramsey indicated no relevant financial relationships.
Maisam Abu-El-Haija indicated no relevant financial relationships.
Georgios Papachristou: AbbVie – Grant/Research Support.
Luis Lara, MD1, Moamen Gabr, MD, MSc1, Rosanne Danielson, MD1, Wei-Wen Hsu, PhD1, Milton Smith, MD1, Inuk Zandvakili, MD, PhD1, Andrew Ofosu, MD, MPH2, Mitchell L. Ramsey, MD3, Maisam Abu-El-Haija, MD4, Georgios I. Papachristou, MD, PhD3. P4361 - Decreased Risk of a Subsequent Diagnosis of Chronic Pancreatitis Following a First Acute Pancreatitis Event in Patients With DM Type 2 Taking Metformin, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
