Tuesday Poster Session
Category: Biliary/Pancreas
P4337 - Cannabis Use Is Associated With Better Outcomes in Patients With Acute Pancreatitis: A Propensity-Matched Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mahmoud Y. Madi, MD (he/him/his)
University of Texas at Austin Dell Medical School
Austin, TX
Presenting Author(s)
Mahmoud Y. Madi, MD1, Noemy Coreas, MD2, Ayah Obeid, MD3, Christopher Nguyen, MD4, Wissam Kiwan, MD5
1University of Texas at Austin Dell Medical School, Austin, TX; 2National University of El Salvador, El Salvador, San Salvador, El Salvador; 3St. Luke's University Health Network, Bethlehem, PA; 4Saint Louis University, St. Louis, MO; 5SSM Health Saint Louis University Hospital, Saint Louis, MO
Introduction: The rate of cannabis use has been increasing especially since the legalization of marijuana in the United States and is estimated to be used by over 200 million people worldwide. There has been conflicting evidence regarding the effect of cannabis in acute pancreatitis (AP), with studies suggesting a potential protective effect of cannabis while others suggesting an increase in incidence of AP in cannabis users. This study aims to compare and highlight the demographics and outcomes in patient with AP who used cannabis compared to those who did not use cannabis.
Methods: This retrospective cohort study used the TriNetX research network to identify adults (≥ 18 years) diagnosed with AP irrespective of the etiology. Patients were matched using propensity score matching and stratified to two groups: Patients who used cannabis and patients who did not. The primary outcome was the 30-day all-cause mortality. Secondary outcomes included 30-day incidence of intensive care unit (ICU) admission, acute respiratory distress syndrome (ARDS), acute kidney injury (AKI), sepsis. Patients’ median follow-up was 1 year for both cohorts.
Results: A total of 33,455 patients with AP who used cannabis were identified and propensity matched with 33,455 patients with AP who did not use cannabis. Among unmatched samples, cannabis users had increased rates of alcohol use, cholelithiasis, cigarette smoking, and cancers (all p< 0.001) (Table 1). Cannabis use in patients with AP was associated with decreased all-cause mortality (adjusted Odds Ratio (aOR) = 0.73, 95% CI: 0.65-0.82), ICU admissions (adjusted Odds Ratio (aOR) = 0.73, 95% CI: 0.65-0.82), ARDS (aOR = 0.63, 95% CI: 0.81-0.93), AKI (aOR = 0.94, 95% CI: 0.88-0.99), and sepsis (aOR 0.87, 95% CI: 0.80-0.95).
Discussion: This retrospective cohort study found that cannabis use could be protective in patients with acute pancreatitis, with decreased rates of all-cause mortality, ICU admission, ARDS, AKI, and sepsis. Additional prospective studies should be performed to assess the possible pathophysiological mechanisms explaining these differences.
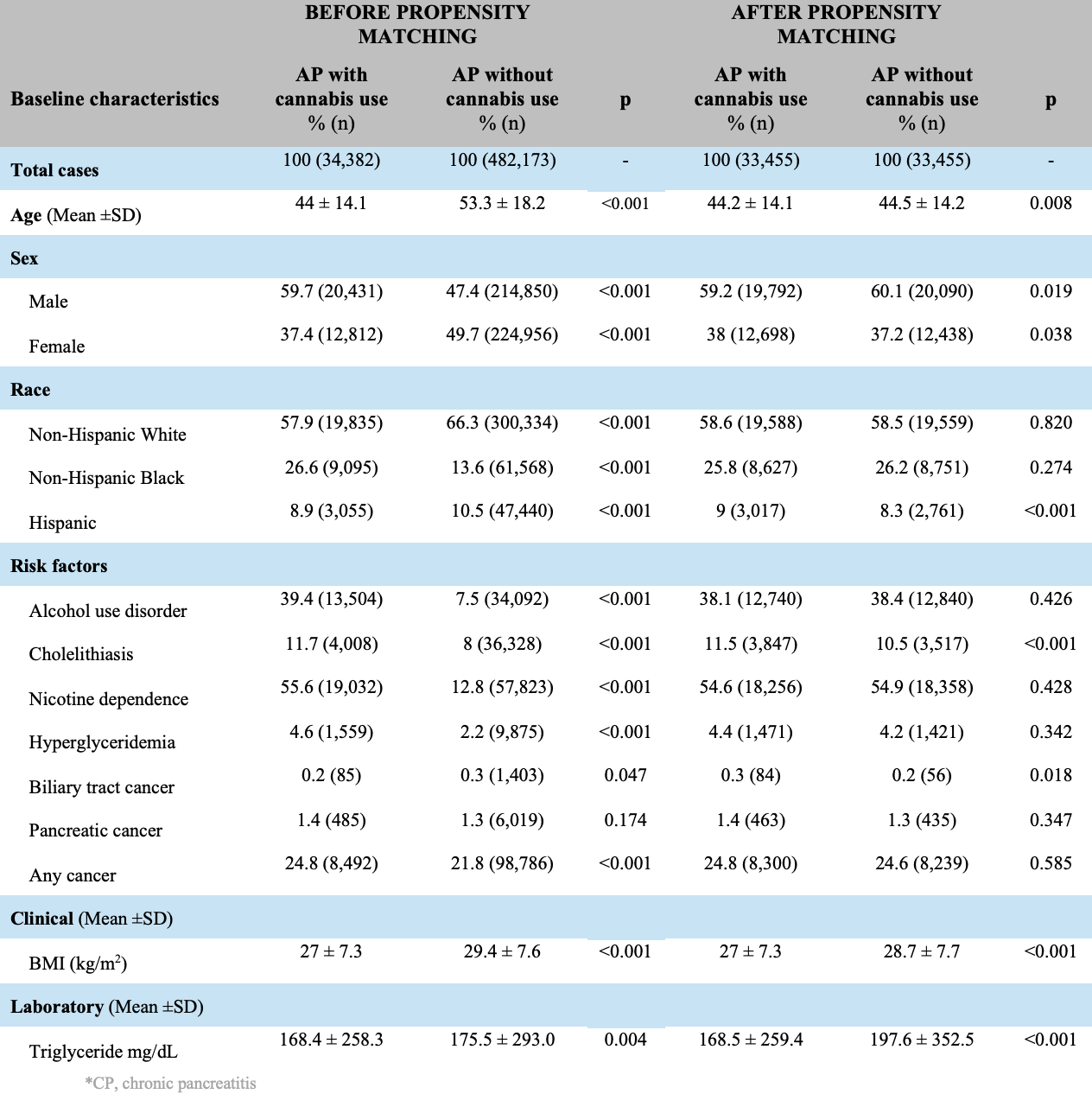
Figure: Table 1. Baseline characteristics when comparing patients with acute pancreatitis using cannabis compared to non-users
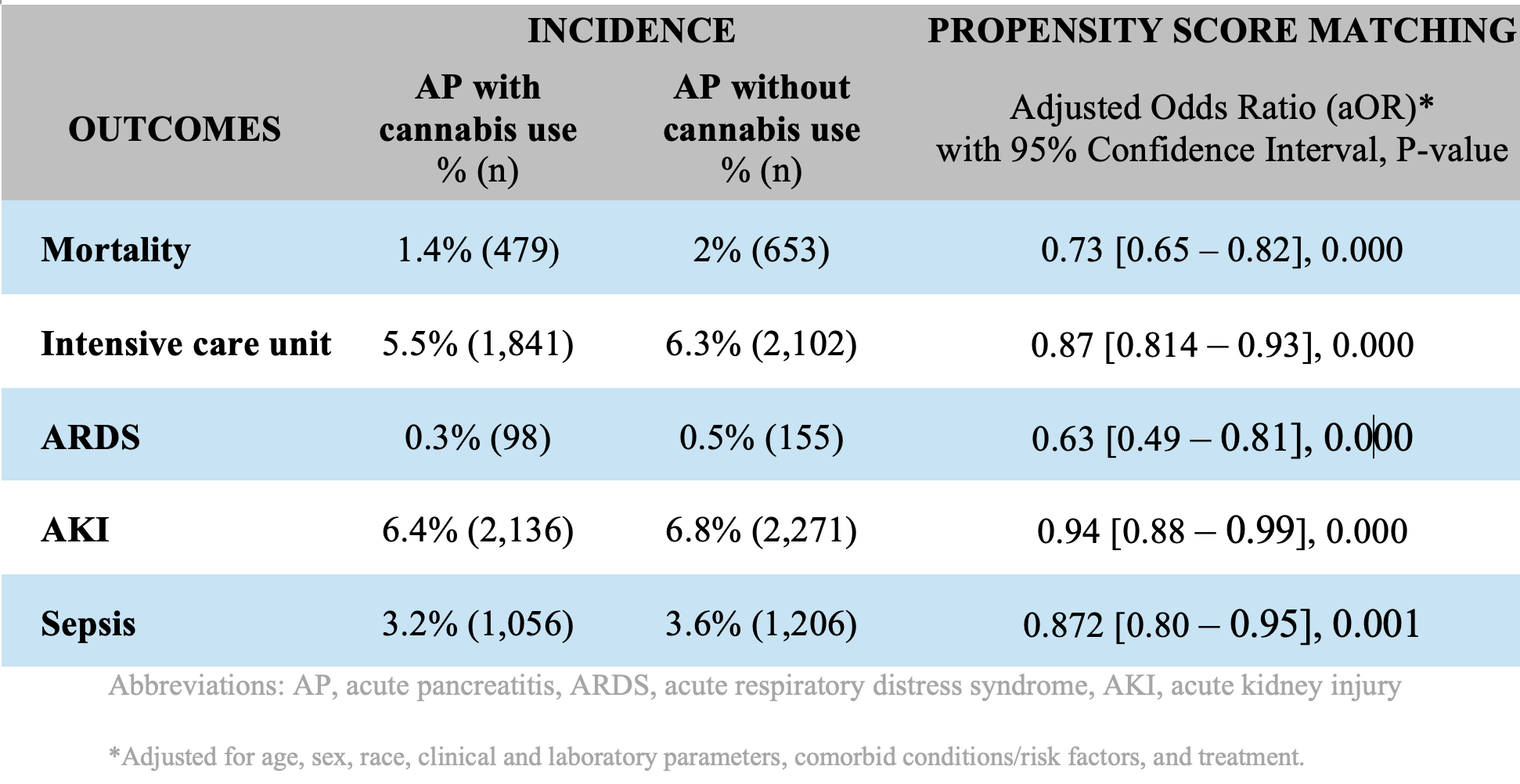
Figure: Table 2. 30-day outcomes when comparing patients with acute pancreatitis using cannabis compared to non-users
Disclosures:
Mahmoud Madi indicated no relevant financial relationships.
Noemy Coreas indicated no relevant financial relationships.
Ayah Obeid indicated no relevant financial relationships.
Christopher Nguyen indicated no relevant financial relationships.
Wissam Kiwan indicated no relevant financial relationships.
Mahmoud Y. Madi, MD1, Noemy Coreas, MD2, Ayah Obeid, MD3, Christopher Nguyen, MD4, Wissam Kiwan, MD5. P4337 - Cannabis Use Is Associated With Better Outcomes in Patients With Acute Pancreatitis: A Propensity-Matched Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas at Austin Dell Medical School, Austin, TX; 2National University of El Salvador, El Salvador, San Salvador, El Salvador; 3St. Luke's University Health Network, Bethlehem, PA; 4Saint Louis University, St. Louis, MO; 5SSM Health Saint Louis University Hospital, Saint Louis, MO
Introduction: The rate of cannabis use has been increasing especially since the legalization of marijuana in the United States and is estimated to be used by over 200 million people worldwide. There has been conflicting evidence regarding the effect of cannabis in acute pancreatitis (AP), with studies suggesting a potential protective effect of cannabis while others suggesting an increase in incidence of AP in cannabis users. This study aims to compare and highlight the demographics and outcomes in patient with AP who used cannabis compared to those who did not use cannabis.
Methods: This retrospective cohort study used the TriNetX research network to identify adults (≥ 18 years) diagnosed with AP irrespective of the etiology. Patients were matched using propensity score matching and stratified to two groups: Patients who used cannabis and patients who did not. The primary outcome was the 30-day all-cause mortality. Secondary outcomes included 30-day incidence of intensive care unit (ICU) admission, acute respiratory distress syndrome (ARDS), acute kidney injury (AKI), sepsis. Patients’ median follow-up was 1 year for both cohorts.
Results: A total of 33,455 patients with AP who used cannabis were identified and propensity matched with 33,455 patients with AP who did not use cannabis. Among unmatched samples, cannabis users had increased rates of alcohol use, cholelithiasis, cigarette smoking, and cancers (all p< 0.001) (Table 1). Cannabis use in patients with AP was associated with decreased all-cause mortality (adjusted Odds Ratio (aOR) = 0.73, 95% CI: 0.65-0.82), ICU admissions (adjusted Odds Ratio (aOR) = 0.73, 95% CI: 0.65-0.82), ARDS (aOR = 0.63, 95% CI: 0.81-0.93), AKI (aOR = 0.94, 95% CI: 0.88-0.99), and sepsis (aOR 0.87, 95% CI: 0.80-0.95).
Discussion: This retrospective cohort study found that cannabis use could be protective in patients with acute pancreatitis, with decreased rates of all-cause mortality, ICU admission, ARDS, AKI, and sepsis. Additional prospective studies should be performed to assess the possible pathophysiological mechanisms explaining these differences.
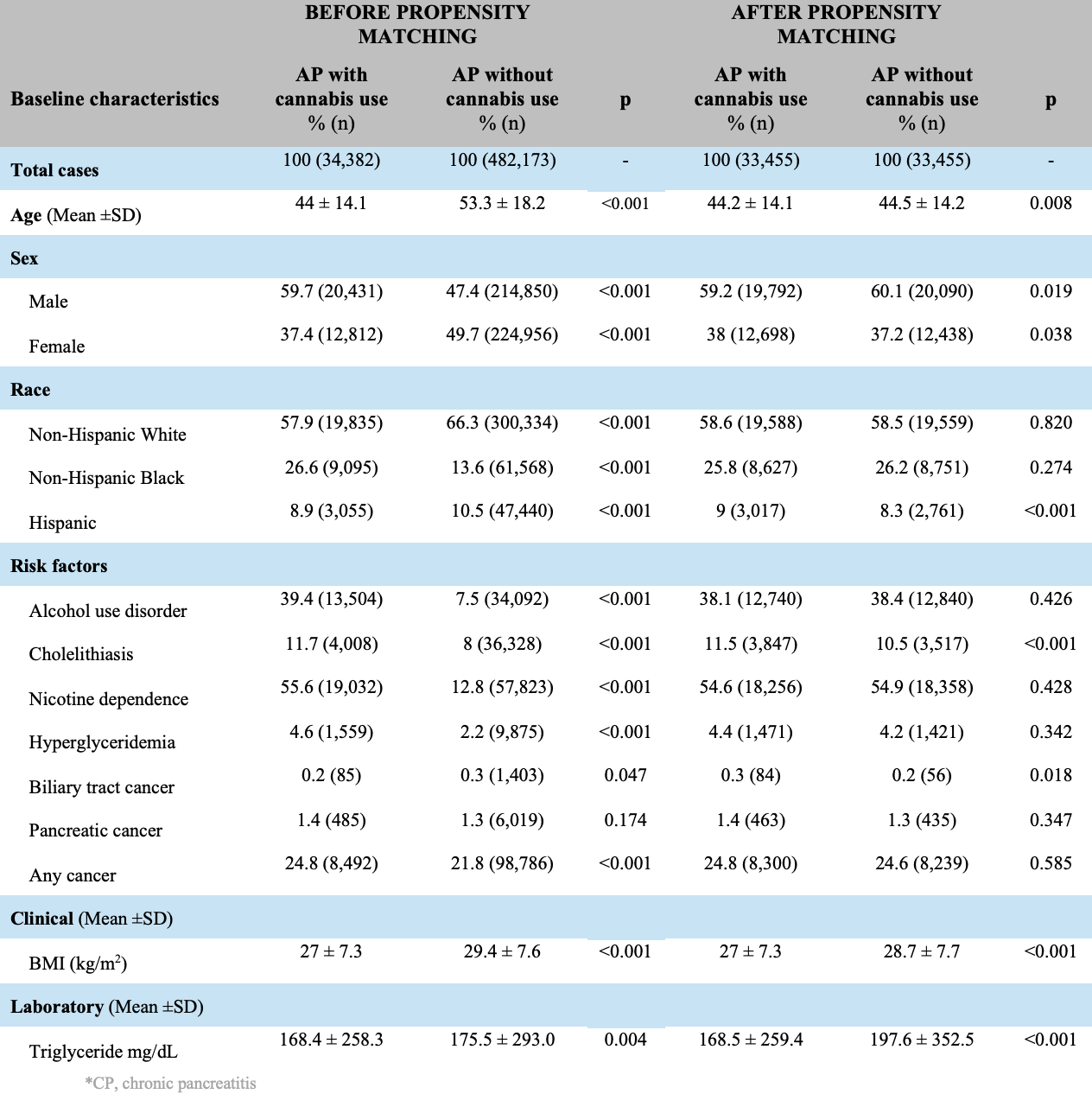
Figure: Table 1. Baseline characteristics when comparing patients with acute pancreatitis using cannabis compared to non-users
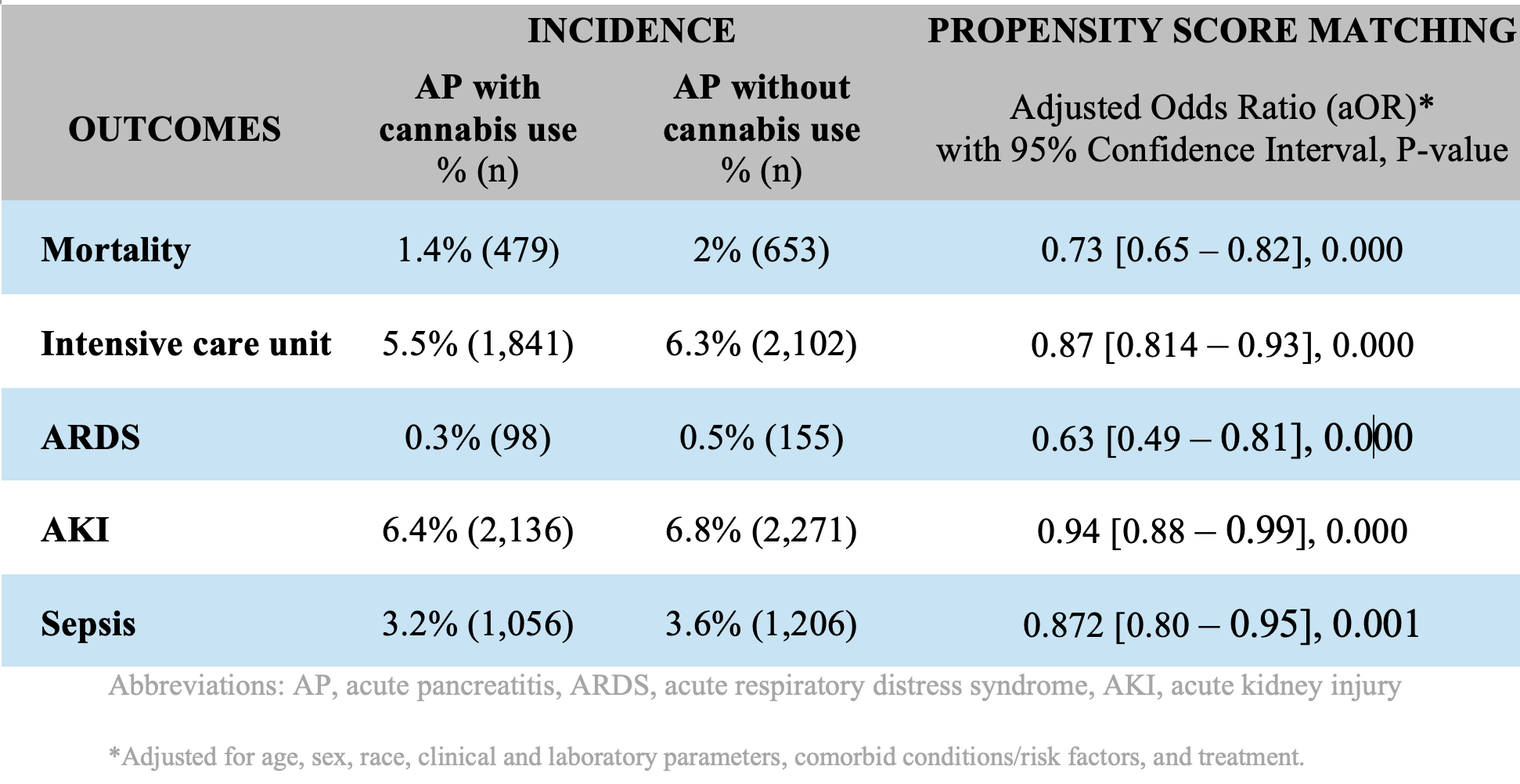
Figure: Table 2. 30-day outcomes when comparing patients with acute pancreatitis using cannabis compared to non-users
Disclosures:
Mahmoud Madi indicated no relevant financial relationships.
Noemy Coreas indicated no relevant financial relationships.
Ayah Obeid indicated no relevant financial relationships.
Christopher Nguyen indicated no relevant financial relationships.
Wissam Kiwan indicated no relevant financial relationships.
Mahmoud Y. Madi, MD1, Noemy Coreas, MD2, Ayah Obeid, MD3, Christopher Nguyen, MD4, Wissam Kiwan, MD5. P4337 - Cannabis Use Is Associated With Better Outcomes in Patients With Acute Pancreatitis: A Propensity-Matched Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
