Tuesday Poster Session
Category: Biliary/Pancreas
P4335 - Comparative Outcomes of High-Intensity Hydrophilic vs Lipophilic Statins in Patients With Primary Biliary Cholangitis: A Real-World Global Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hussam Kawas, MD
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Hussam Kawas, MD1, Mohammad Alabbas, MD2, Mohamad-Noor Abu-Hammour, MD3, Walid Hazem, DO4, Barish Eren, MD1, Omar Sims, PhD5, Dian Jung Chiang, MD3
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic Foundation, South Euclid, OH; 3Cleveland Clinic, Cleveland, OH; 4University Hospitals Cleveland Medical Center, Cleveland, OH; 5Cleveland Clinic Foundation, Hoover, AL
Introduction: Primary biliary cholangitis (PBC) is a chronic autoimmune cholestatic liver disease characterized by progressive bile duct destruction and impaired lipid absorption. The pathophysiology may influence the bioavailability and efficacy of hydrophilic vs lipophilic statins, particularly given their varying solubility and pharmacokinetic profiles. It remains unclear whether these differences translate to different clinical outcomes in patients with PBC. Despite the known cardiovascular risks of dyslipidemia, statin use in PBC remains underutilized due to longstanding concerns over hepatotoxicity. Evaluating the comparative safety and effectiveness of statin classes in this unique population is crucial.
Methods: We conducted a retrospective analysis using the TriNetX global research network. Adult patients with a diagnosis of PBC were included if they were prescribed a high-intensity hydrophilic statin (e.g., rosuvastatin) or a high-intensity lipophilic statin (e.g., atorvastatin). Patients were propensity-score matched (1:1) on demographics and comorbidities. Primary outcomes included major adverse cardiovascular events (MACE), all-cause mortality, and liver-related outcomes (cirrhosis, ascites, hepatic encephalopathy [HE], varices, hepatocellular carcinoma [HCC], paracentesis). Secondary outcomes included hospitalizations and quality-of-life markers (i.e., fatigue, pruritus, depression).
Results: After matching, 719 patients per patient group were included in the analysis. There were no significant differences in the incidence of MACE (39.2% high-intensity hydrophilic vs. 42.7% high-intensity lipophilic; HR=0.87 [95% CI: 0.74–1.02], p=0.18) or all-cause mortality (11.7% high-intensity hydrophilic vs. 12.0% high-intensity lipophilic; HR=0.96 [95% CI: 0.71–1.30], p=0.87]). Liver outcomes (i.e., cirrhosis, ascites, SBP, HE, varices, HCC) and symptom burden (i.e., fatigue, pruritus, depression) were similar between both groups (all p-values >0.05). However, the incidence of all-cause hospitalizations was significantly lower in the hydrophilic statin group (27.4% vs. 38.1%; HR=0.66 [95% CI: 0.55–0.79], p< 0.001]).
Discussion: In this large real-world study of patients with PBC, high-intensity hydrophilic statins were associated with a significantly lower rate of all-cause hospitalizations, with no increase in liver-related and cardiac complications or mortality compared to lipophilic statins. These findings suggest that hydrophilic statins may offer a more favorable safety profile in PBC patients.
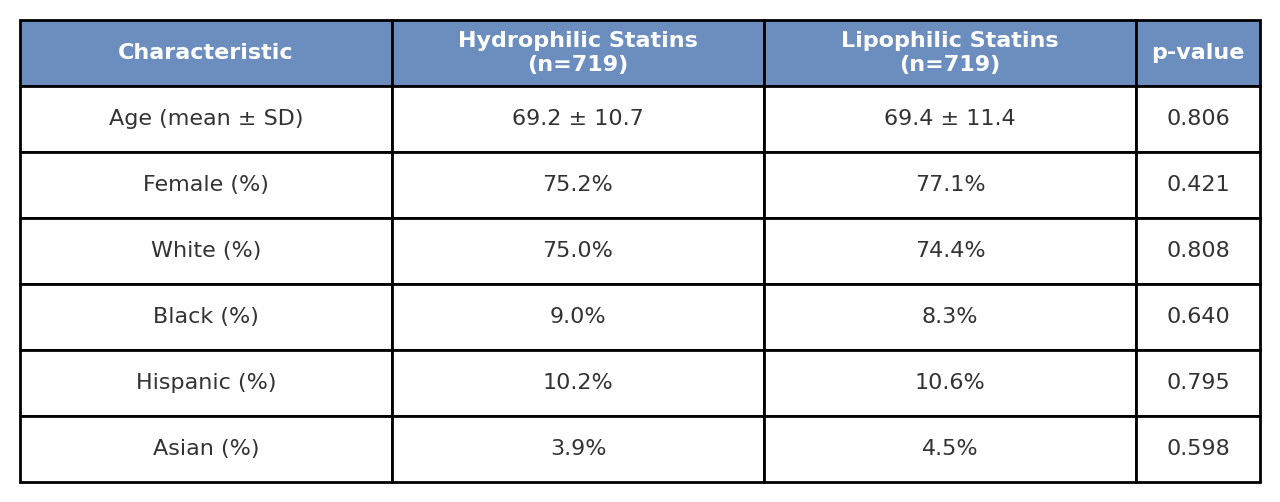
Figure: Table 1. Demographics
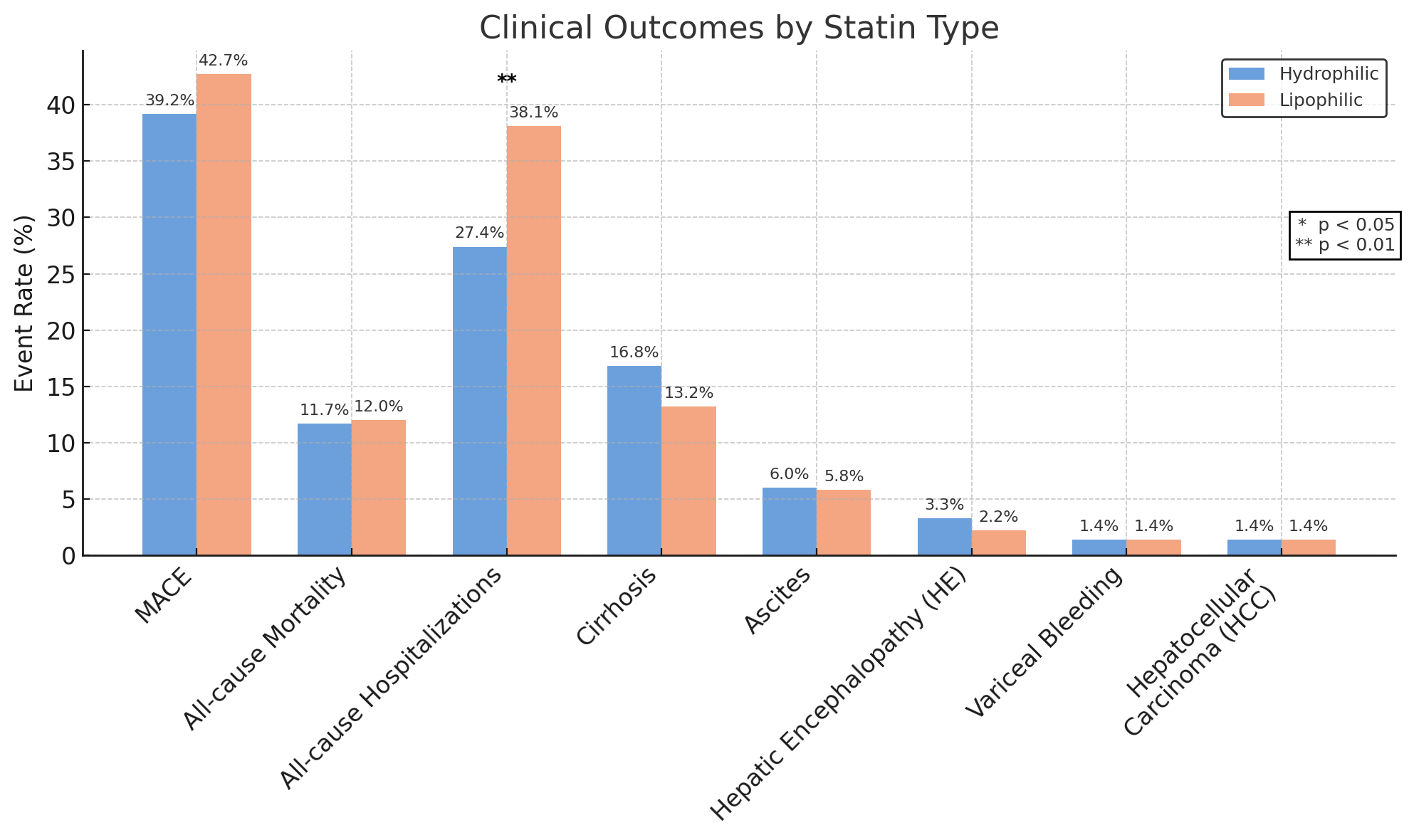
Figure: Table 2. Clinical Outcomes by Statin Type in PBC
Disclosures:
Hussam Kawas indicated no relevant financial relationships.
Mohammad Alabbas indicated no relevant financial relationships.
Mohamad-Noor Abu-Hammour indicated no relevant financial relationships.
Walid Hazem indicated no relevant financial relationships.
Barish Eren indicated no relevant financial relationships.
Omar Sims indicated no relevant financial relationships.
Dian Jung Chiang: Ipsen – Advisory Committee/Board Member.
Hussam Kawas, MD1, Mohammad Alabbas, MD2, Mohamad-Noor Abu-Hammour, MD3, Walid Hazem, DO4, Barish Eren, MD1, Omar Sims, PhD5, Dian Jung Chiang, MD3. P4335 - Comparative Outcomes of High-Intensity Hydrophilic vs Lipophilic Statins in Patients With Primary Biliary Cholangitis: A Real-World Global Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic Foundation, South Euclid, OH; 3Cleveland Clinic, Cleveland, OH; 4University Hospitals Cleveland Medical Center, Cleveland, OH; 5Cleveland Clinic Foundation, Hoover, AL
Introduction: Primary biliary cholangitis (PBC) is a chronic autoimmune cholestatic liver disease characterized by progressive bile duct destruction and impaired lipid absorption. The pathophysiology may influence the bioavailability and efficacy of hydrophilic vs lipophilic statins, particularly given their varying solubility and pharmacokinetic profiles. It remains unclear whether these differences translate to different clinical outcomes in patients with PBC. Despite the known cardiovascular risks of dyslipidemia, statin use in PBC remains underutilized due to longstanding concerns over hepatotoxicity. Evaluating the comparative safety and effectiveness of statin classes in this unique population is crucial.
Methods: We conducted a retrospective analysis using the TriNetX global research network. Adult patients with a diagnosis of PBC were included if they were prescribed a high-intensity hydrophilic statin (e.g., rosuvastatin) or a high-intensity lipophilic statin (e.g., atorvastatin). Patients were propensity-score matched (1:1) on demographics and comorbidities. Primary outcomes included major adverse cardiovascular events (MACE), all-cause mortality, and liver-related outcomes (cirrhosis, ascites, hepatic encephalopathy [HE], varices, hepatocellular carcinoma [HCC], paracentesis). Secondary outcomes included hospitalizations and quality-of-life markers (i.e., fatigue, pruritus, depression).
Results: After matching, 719 patients per patient group were included in the analysis. There were no significant differences in the incidence of MACE (39.2% high-intensity hydrophilic vs. 42.7% high-intensity lipophilic; HR=0.87 [95% CI: 0.74–1.02], p=0.18) or all-cause mortality (11.7% high-intensity hydrophilic vs. 12.0% high-intensity lipophilic; HR=0.96 [95% CI: 0.71–1.30], p=0.87]). Liver outcomes (i.e., cirrhosis, ascites, SBP, HE, varices, HCC) and symptom burden (i.e., fatigue, pruritus, depression) were similar between both groups (all p-values >0.05). However, the incidence of all-cause hospitalizations was significantly lower in the hydrophilic statin group (27.4% vs. 38.1%; HR=0.66 [95% CI: 0.55–0.79], p< 0.001]).
Discussion: In this large real-world study of patients with PBC, high-intensity hydrophilic statins were associated with a significantly lower rate of all-cause hospitalizations, with no increase in liver-related and cardiac complications or mortality compared to lipophilic statins. These findings suggest that hydrophilic statins may offer a more favorable safety profile in PBC patients.
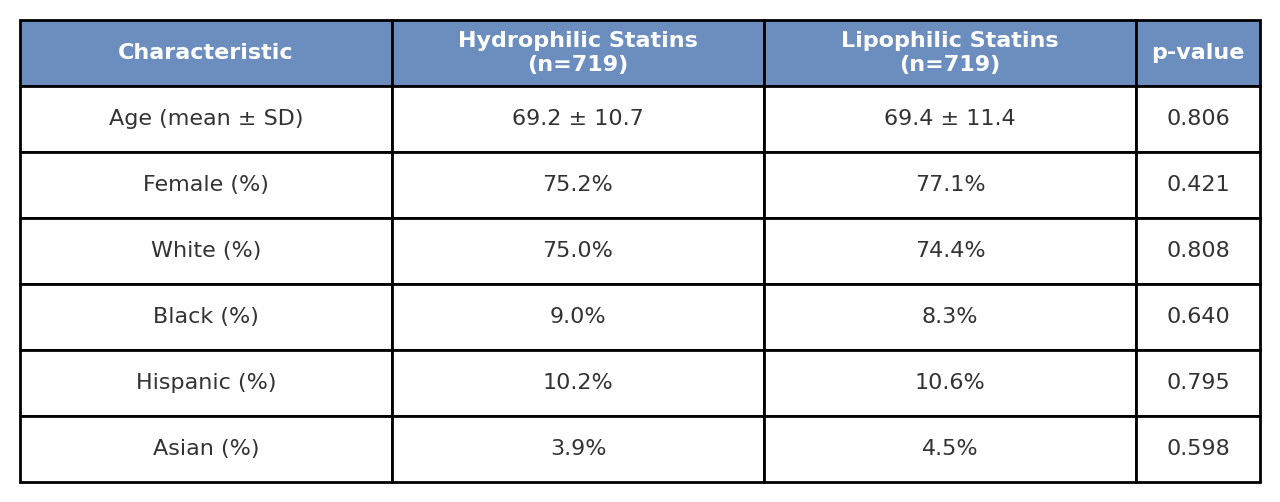
Figure: Table 1. Demographics
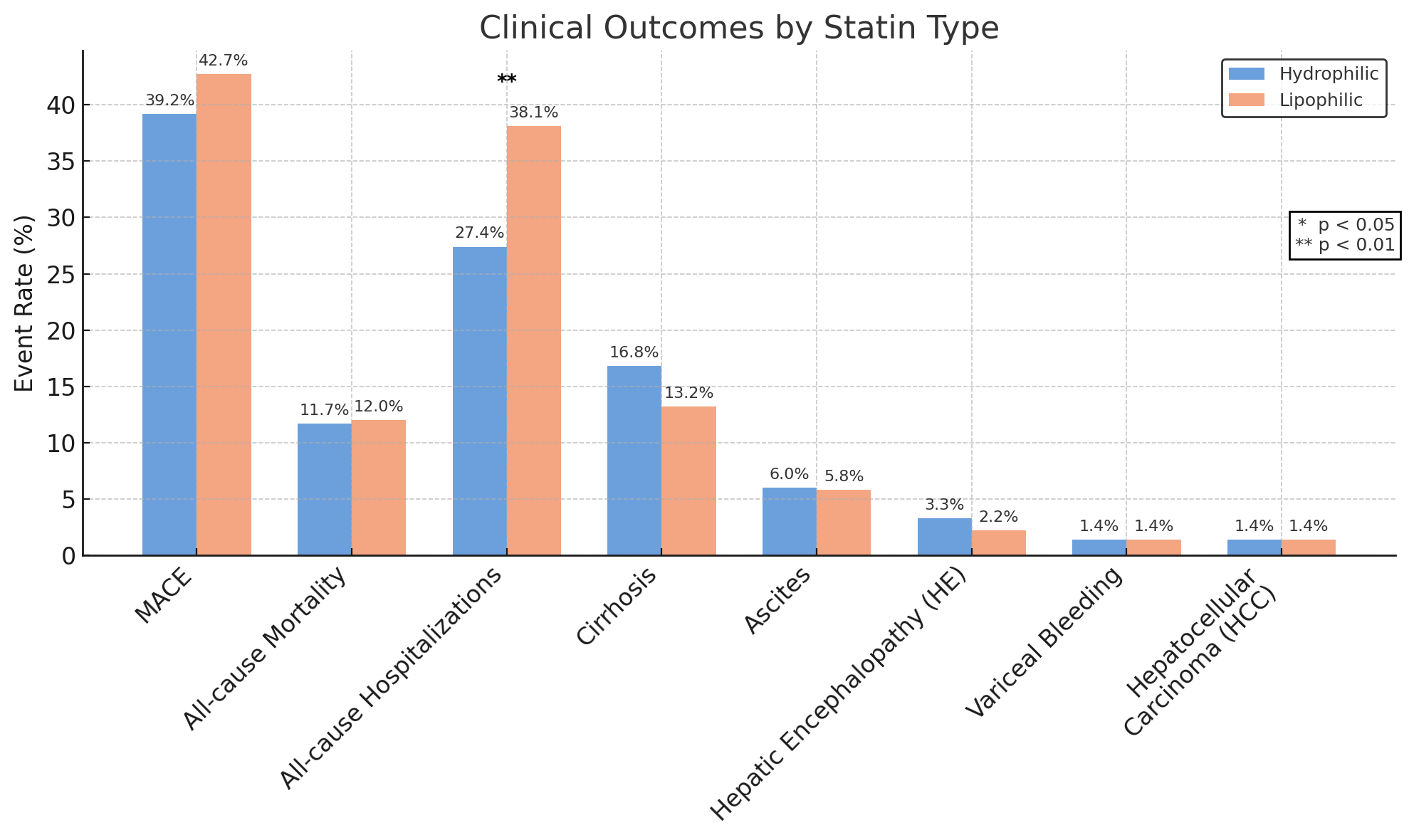
Figure: Table 2. Clinical Outcomes by Statin Type in PBC
Disclosures:
Hussam Kawas indicated no relevant financial relationships.
Mohammad Alabbas indicated no relevant financial relationships.
Mohamad-Noor Abu-Hammour indicated no relevant financial relationships.
Walid Hazem indicated no relevant financial relationships.
Barish Eren indicated no relevant financial relationships.
Omar Sims indicated no relevant financial relationships.
Dian Jung Chiang: Ipsen – Advisory Committee/Board Member.
Hussam Kawas, MD1, Mohammad Alabbas, MD2, Mohamad-Noor Abu-Hammour, MD3, Walid Hazem, DO4, Barish Eren, MD1, Omar Sims, PhD5, Dian Jung Chiang, MD3. P4335 - Comparative Outcomes of High-Intensity Hydrophilic vs Lipophilic Statins in Patients With Primary Biliary Cholangitis: A Real-World Global Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
