Tuesday Poster Session
Category: Biliary/Pancreas
P4332 - Post-Endoscopic Retrograde Cholangiopancreatography (ERCP) Cholangitis: A Comprehensive Systematic Review and Meta-Analysis of Incidence and Predictive Risk Factors
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- HP
Harsh Patel, MD
NewYork-Presbyterian / Brooklyn Methodist Hospital
Brooklyn, NY
Presenting Author(s)
Harsh Patel, MD1, Kin Li, MD2, Anas Zaher, MD2, Karthik Chandrasekaran, MD2, Drew Wright, 3, Nicholas Brown, MD2
1NewYork-Presbyterian / Brooklyn Methodist Hospital, Brooklyn, NY; 2New York Brooklyn Methodist Hospital, Brooklyn, NY; 3Weill Cornell Medicine, New York, NY
Introduction: Endoscopic Retrograde Cholangiopancreatography (ERCP) has been used for both diagnostic and therapeutic purposes since its introduction in 1968. However, as endoscopic ultrasound (EUS) applications expand and MRI imaging technology improves, the indications for using ERCP have shifted towards therapeutic purposes. Coinciding with this change, there has been anincrease in ERCP-related adverse events, most notably post-ERCP cholangitis (PEC). Updated data on PEC following a shift in ERCP use patterns is currently lacking. We aim to comprehensively examine the incidence and risk factors associated with post-ERCP cholangitis in the modern era
Methods: Relevant publications from 2000-2024 were obtained from Embase, MEDLINE, and PubMed. Inclusion criteria were adult patients undergoing ERCP with documentation of post-ERCP cholangitis as well as any risk factors for post ERCP cholangitis. Post ERCP cholangitis definitions were exclusively defined by each study. Exclusion criteria included studies with patient population who had risk factors for incomplete biliary drainage (malignant hilar obstructions), primary sclerosing cholangitis, and post-liver transplant on immunosuppression. Data analysis was performed using R Software.
Results: Our search identified 6701 unique citations. 38 studies were included in the final review (Figure 1). The average incidence of post-ERCP cholangitis was 8.08%, ranging from 0.60% to 71.90%. The median age of all patients in the studies was 61.46. Those with age >60 were more likely to develop post-ERCP cholangitis (2.02 [1.36 - 3.06]), while males were found to have a lower risk (0.68 [0.50 - 0.92]) compared to females. Though based on limited studies, balloon dilation and difficult cannulation were additionally associated with increased risk of cholangitis (7.13 [4.66 - 10.92]), and (5.30 [1.17 - 24.07]), respectively. Biliary sphincterotomy and periampullary diverticulum were not found to have an increased risk, although there was significant heterogeneity between studies.
Discussion: Our comprehensive review of studies over 24 years found an average incidence of PEC to be 8.08% with advancing age being a significant risk factor for PEC in 3.4% of patients over 60 years old. These findings highlight the importance of patient-specific risk stratification and reinforces the need for prophylactic strategies in high-risk populations to reduce the burden of PEC in the modern landscape of ERCP.
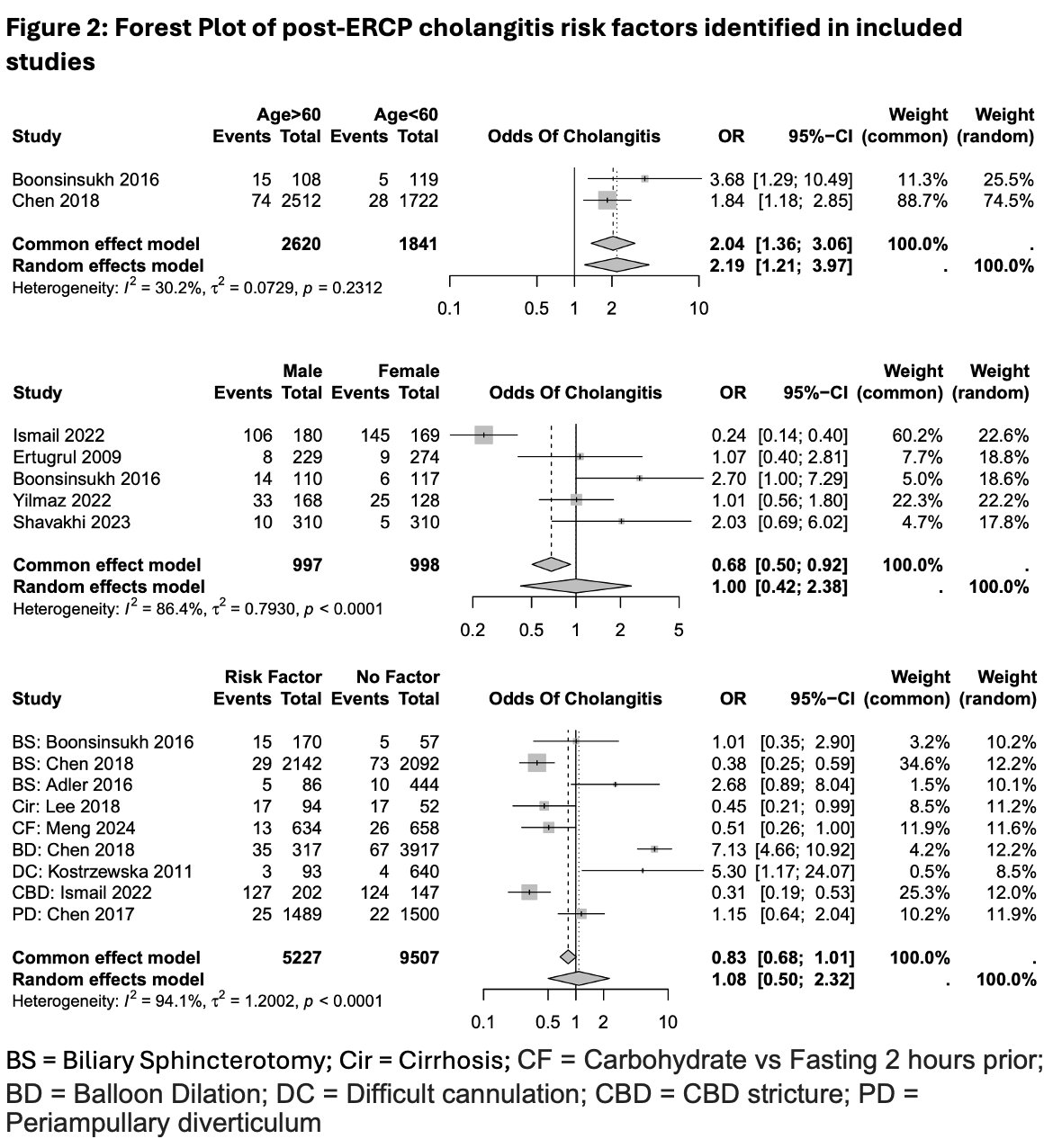
Figure: Figure 1: Study extraction data
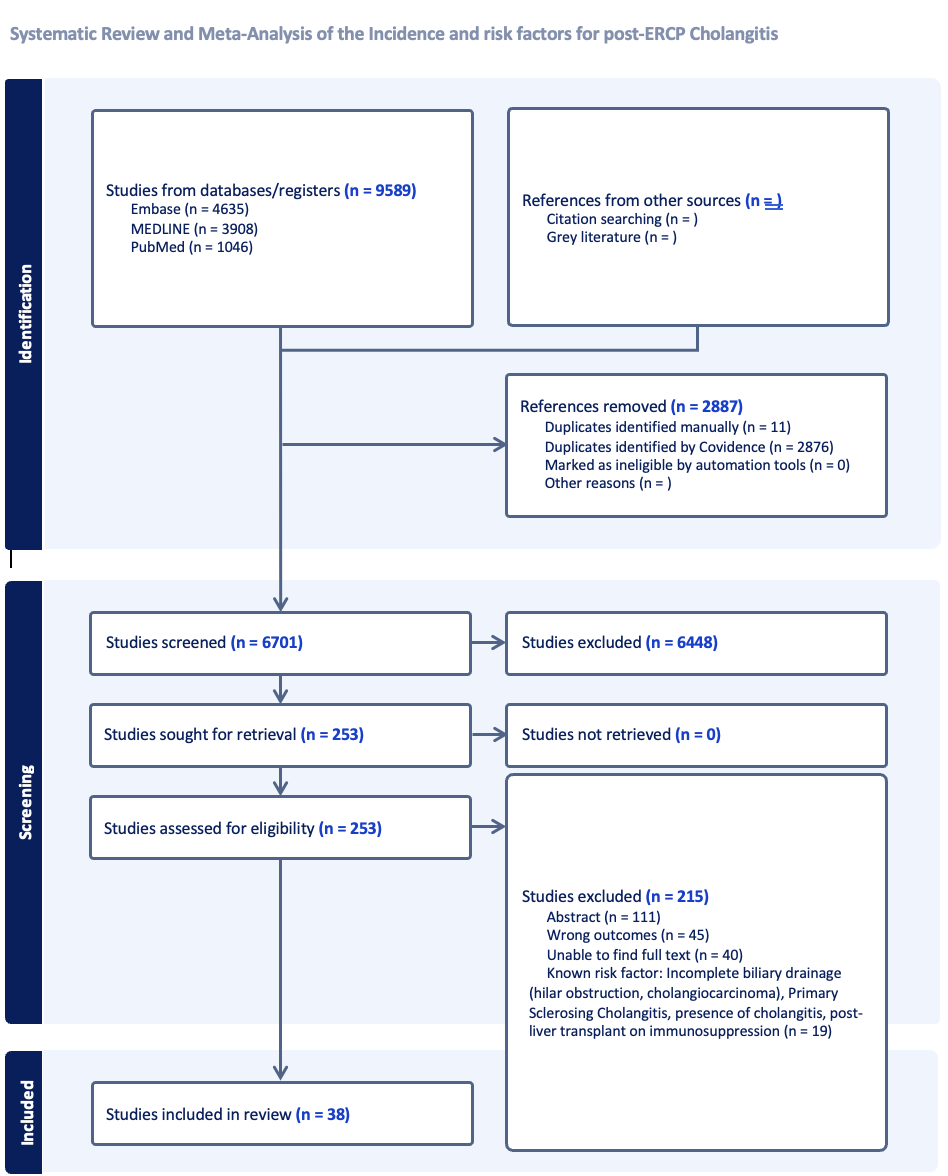
Figure: Figure 2: Forest Plot of post-ERCP cholangitis risk factors identified in included studies
Disclosures:
Harsh Patel indicated no relevant financial relationships.
Kin Li indicated no relevant financial relationships.
Anas Zaher indicated no relevant financial relationships.
Karthik Chandrasekaran indicated no relevant financial relationships.
Drew Wright indicated no relevant financial relationships.
Nicholas Brown indicated no relevant financial relationships.
Harsh Patel, MD1, Kin Li, MD2, Anas Zaher, MD2, Karthik Chandrasekaran, MD2, Drew Wright, 3, Nicholas Brown, MD2. P4332 - Post-Endoscopic Retrograde Cholangiopancreatography (ERCP) Cholangitis: A Comprehensive Systematic Review and Meta-Analysis of Incidence and Predictive Risk Factors, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NewYork-Presbyterian / Brooklyn Methodist Hospital, Brooklyn, NY; 2New York Brooklyn Methodist Hospital, Brooklyn, NY; 3Weill Cornell Medicine, New York, NY
Introduction: Endoscopic Retrograde Cholangiopancreatography (ERCP) has been used for both diagnostic and therapeutic purposes since its introduction in 1968. However, as endoscopic ultrasound (EUS) applications expand and MRI imaging technology improves, the indications for using ERCP have shifted towards therapeutic purposes. Coinciding with this change, there has been anincrease in ERCP-related adverse events, most notably post-ERCP cholangitis (PEC). Updated data on PEC following a shift in ERCP use patterns is currently lacking. We aim to comprehensively examine the incidence and risk factors associated with post-ERCP cholangitis in the modern era
Methods: Relevant publications from 2000-2024 were obtained from Embase, MEDLINE, and PubMed. Inclusion criteria were adult patients undergoing ERCP with documentation of post-ERCP cholangitis as well as any risk factors for post ERCP cholangitis. Post ERCP cholangitis definitions were exclusively defined by each study. Exclusion criteria included studies with patient population who had risk factors for incomplete biliary drainage (malignant hilar obstructions), primary sclerosing cholangitis, and post-liver transplant on immunosuppression. Data analysis was performed using R Software.
Results: Our search identified 6701 unique citations. 38 studies were included in the final review (Figure 1). The average incidence of post-ERCP cholangitis was 8.08%, ranging from 0.60% to 71.90%. The median age of all patients in the studies was 61.46. Those with age >60 were more likely to develop post-ERCP cholangitis (2.02 [1.36 - 3.06]), while males were found to have a lower risk (0.68 [0.50 - 0.92]) compared to females. Though based on limited studies, balloon dilation and difficult cannulation were additionally associated with increased risk of cholangitis (7.13 [4.66 - 10.92]), and (5.30 [1.17 - 24.07]), respectively. Biliary sphincterotomy and periampullary diverticulum were not found to have an increased risk, although there was significant heterogeneity between studies.
Discussion: Our comprehensive review of studies over 24 years found an average incidence of PEC to be 8.08% with advancing age being a significant risk factor for PEC in 3.4% of patients over 60 years old. These findings highlight the importance of patient-specific risk stratification and reinforces the need for prophylactic strategies in high-risk populations to reduce the burden of PEC in the modern landscape of ERCP.
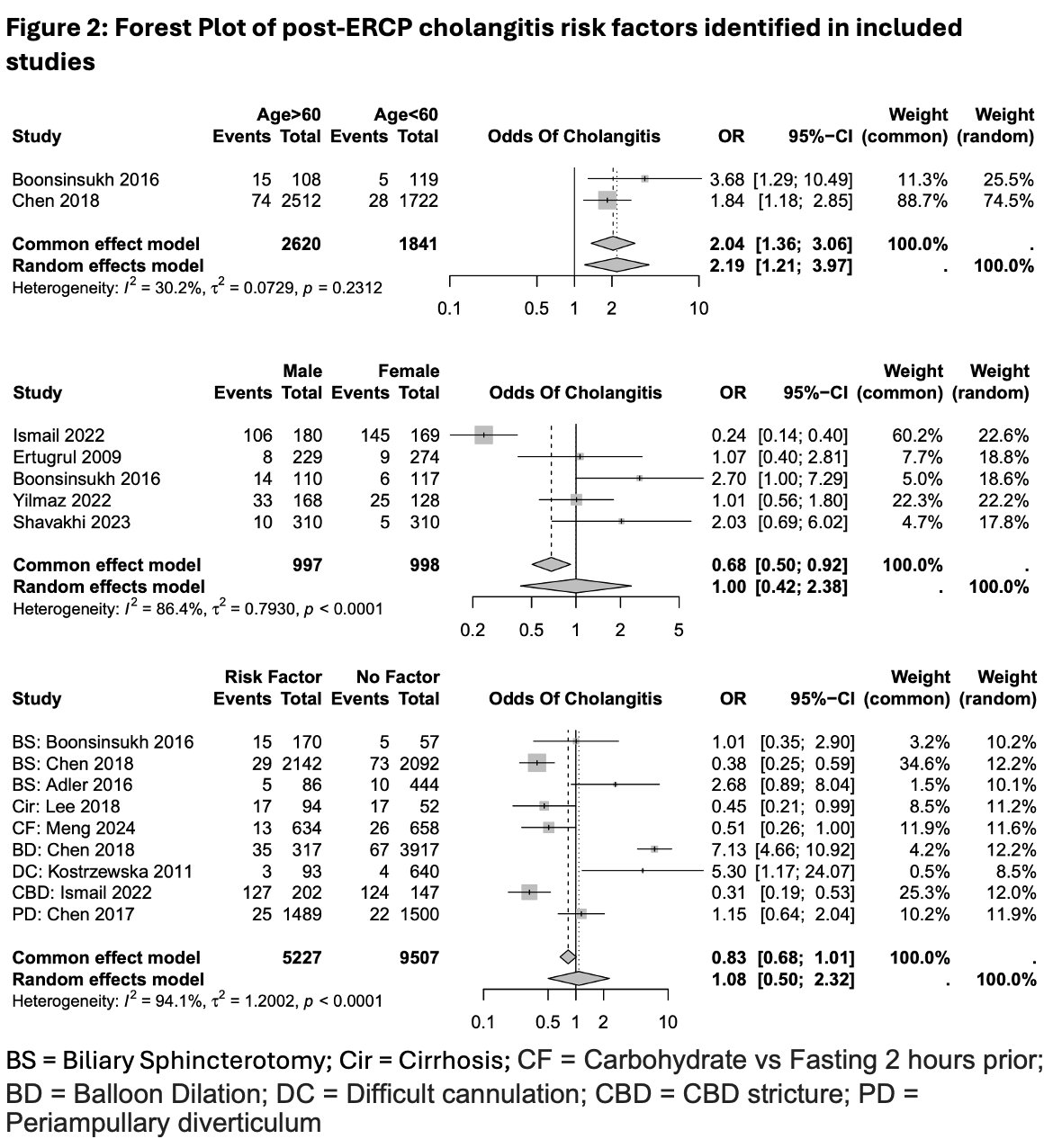
Figure: Figure 1: Study extraction data
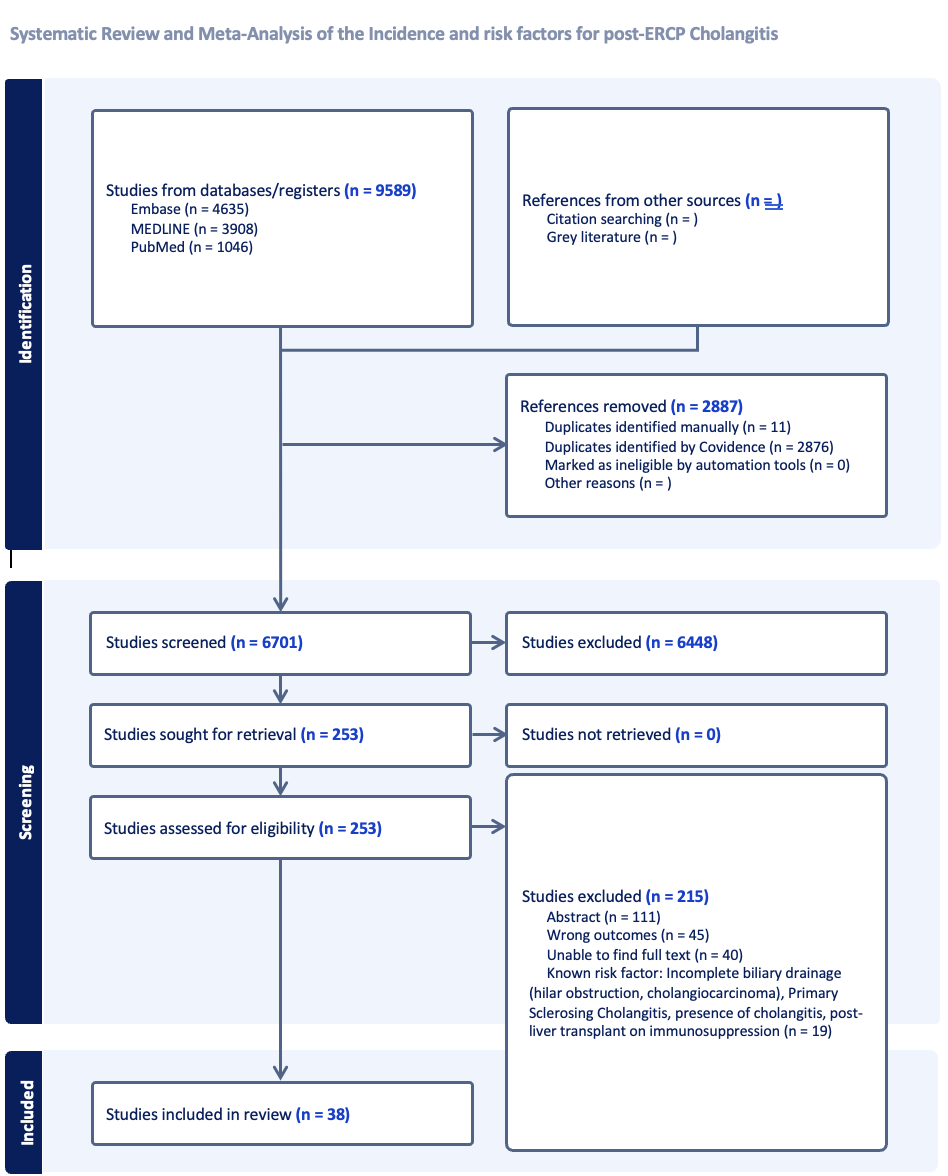
Figure: Figure 2: Forest Plot of post-ERCP cholangitis risk factors identified in included studies
Disclosures:
Harsh Patel indicated no relevant financial relationships.
Kin Li indicated no relevant financial relationships.
Anas Zaher indicated no relevant financial relationships.
Karthik Chandrasekaran indicated no relevant financial relationships.
Drew Wright indicated no relevant financial relationships.
Nicholas Brown indicated no relevant financial relationships.
Harsh Patel, MD1, Kin Li, MD2, Anas Zaher, MD2, Karthik Chandrasekaran, MD2, Drew Wright, 3, Nicholas Brown, MD2. P4332 - Post-Endoscopic Retrograde Cholangiopancreatography (ERCP) Cholangitis: A Comprehensive Systematic Review and Meta-Analysis of Incidence and Predictive Risk Factors, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
