Tuesday Poster Session
Category: Biliary/Pancreas
P4324 - Trends in Acute Pancreatitis Hospitalization and In-Hospital Mortality in the United States (1999-2023): Evaluating the Role of Healthcare Access and Regional Disparities
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Maham Maqsood, MBBS
Allama Iqbal Medical College, Lahore
Lahore, Punjab, Pakistan
Presenting Author(s)
Maryam Saghir, MBBS1, Eshal Saghir, MBBS2, Maham Maqsood, MBBS3, Amjad Zafar, MBBS4, Sahil Jairamani, MBBS5, Maha Sajjad, MBBS6
1Jinnah Sindh Medical University, Karachi, Sindh, Pakistan; 2Dow University of Health Sciences, Karachi, Sindh, Pakistan; 3Allama Iqbal Medical College, Lahore, Lahore, Punjab, Pakistan; 4Jinnah Hospital, Lahore, Lahore, Punjab, Pakistan; 5Liaquat University of Medical and Health Science, Jamshoro, Pakistan, Jamshoro, Sindh, Pakistan; 6King Edward Medical University, Lahore, Lahore, Punjab, Pakistan
Introduction: Acute pancreatitis (AP) is a significant contributor to gastrointestinal mortality and has emerged as a leading cause of gastrointestinal-related hospitalizations in the United States. Despite advances in care, disparities in mortality persist across demographic and geographic groups. This study aims to assess factors influencing hospitalization rates and examine disparities in healthcare access, regional variation, and demographics from 1999-2023.
Methods: A retrospective analysis of AP-related mortality in adults aged ≥25 years was conducted using the CDC WONDER database (1999-2023), using the ICD-10 code K85. Age-adjusted mortality rates (AAMRs) per 100,000 were standardized to the 2000 U.S. population. Joinpoint regression assessed annual percent changes (APC) and average annual percent change (AAPC) by race, ethnicity, region, and urbanization status.
Results: From 1999-2023, 146,835 AP-related deaths were recorded, with most occurring in medical facilities (111,905). National AAMR declined from 3.31 to 2.49, with a significant AAPC of -1.1% (95% CI: -2.12 to -0.07, p=0.036). Men had higher mortality than women (82,454 vs. 64,381), with 2023 AAMRs of 3.14 vs. 1.88 and AAPCs of -1.05% vs. -1.3%. Racially, NH White individuals had the highest mortality (110,870 deaths), with AAMR dropping from 3.07 to 2.72 (AAPC: -0.59, p=0.409). Geographically, the South had the most deaths (59,340, AAPC: -1.43, p=0.062), while the Northeast had the least (23,304, AAPC: -1.6, p=0.073). Non-metropolitan areas had higher AAMRs than metropolitan areas (3.26 vs. 2.57), but metropolitan areas recorded more deaths (100,560, AAPC: -1.42, p=0.003). Southern and Midwestern states, especially South Carolina (3.95), Kentucky (3.94), and Mississippi (3.74), had the highest AAMRs. In contrast, states like New York (2.00), Massachusetts (2.24), and Pennsylvania (2.40) had lower-than-average mortality.
Discussion: Although mortality due to AP has slightly declined over the past 25 years, significant demographic, regional, and healthcare access disparities persist, underscoring the need for equity-focused interventions in high-risk and geographically vulnerable areas.
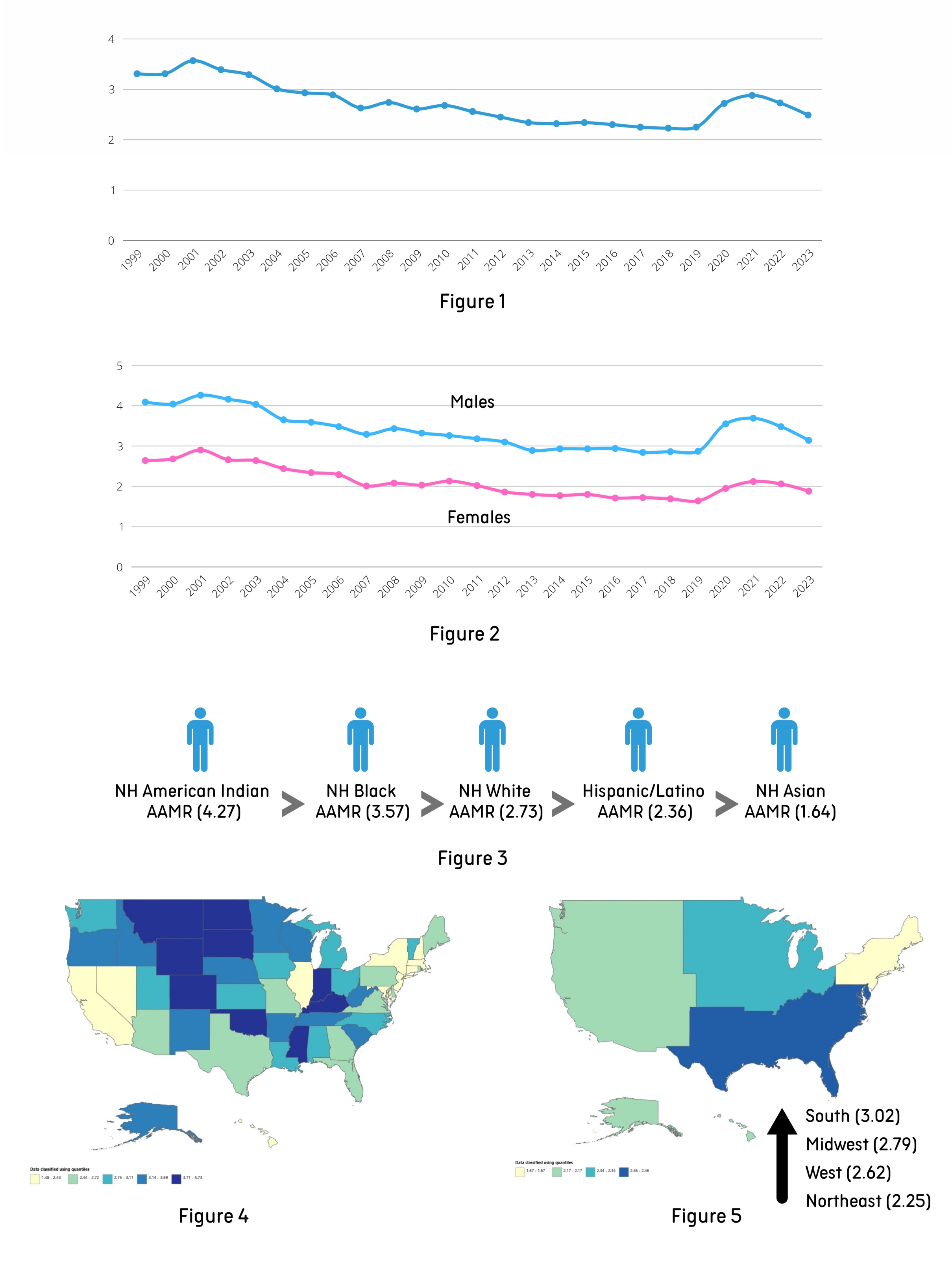
Figure: Figure 1: Overall Age-adjusted Mortality Rates per 100,000 persons
Figure 2: Sex-stratified Trends (Age-adjusted Mortality Rates per 100,000 persons)
Figure 3: Racial Disparities (Age-adjusted Mortality Rates per 100,000 persons)
Figure 4: State-stratified Trends (Age-adjusted Mortality Rates per 100,000 persons)
Figure 5: Census Region-stratified Trends (Age-adjusted Mortality Rates per 100,000 persons)
Disclosures:
Maryam Saghir indicated no relevant financial relationships.
Eshal Saghir indicated no relevant financial relationships.
Maham Maqsood indicated no relevant financial relationships.
Amjad Zafar indicated no relevant financial relationships.
Sahil Jairamani indicated no relevant financial relationships.
Maha Sajjad indicated no relevant financial relationships.
Maryam Saghir, MBBS1, Eshal Saghir, MBBS2, Maham Maqsood, MBBS3, Amjad Zafar, MBBS4, Sahil Jairamani, MBBS5, Maha Sajjad, MBBS6. P4324 - Trends in Acute Pancreatitis Hospitalization and In-Hospital Mortality in the United States (1999-2023): Evaluating the Role of Healthcare Access and Regional Disparities, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Jinnah Sindh Medical University, Karachi, Sindh, Pakistan; 2Dow University of Health Sciences, Karachi, Sindh, Pakistan; 3Allama Iqbal Medical College, Lahore, Lahore, Punjab, Pakistan; 4Jinnah Hospital, Lahore, Lahore, Punjab, Pakistan; 5Liaquat University of Medical and Health Science, Jamshoro, Pakistan, Jamshoro, Sindh, Pakistan; 6King Edward Medical University, Lahore, Lahore, Punjab, Pakistan
Introduction: Acute pancreatitis (AP) is a significant contributor to gastrointestinal mortality and has emerged as a leading cause of gastrointestinal-related hospitalizations in the United States. Despite advances in care, disparities in mortality persist across demographic and geographic groups. This study aims to assess factors influencing hospitalization rates and examine disparities in healthcare access, regional variation, and demographics from 1999-2023.
Methods: A retrospective analysis of AP-related mortality in adults aged ≥25 years was conducted using the CDC WONDER database (1999-2023), using the ICD-10 code K85. Age-adjusted mortality rates (AAMRs) per 100,000 were standardized to the 2000 U.S. population. Joinpoint regression assessed annual percent changes (APC) and average annual percent change (AAPC) by race, ethnicity, region, and urbanization status.
Results: From 1999-2023, 146,835 AP-related deaths were recorded, with most occurring in medical facilities (111,905). National AAMR declined from 3.31 to 2.49, with a significant AAPC of -1.1% (95% CI: -2.12 to -0.07, p=0.036). Men had higher mortality than women (82,454 vs. 64,381), with 2023 AAMRs of 3.14 vs. 1.88 and AAPCs of -1.05% vs. -1.3%. Racially, NH White individuals had the highest mortality (110,870 deaths), with AAMR dropping from 3.07 to 2.72 (AAPC: -0.59, p=0.409). Geographically, the South had the most deaths (59,340, AAPC: -1.43, p=0.062), while the Northeast had the least (23,304, AAPC: -1.6, p=0.073). Non-metropolitan areas had higher AAMRs than metropolitan areas (3.26 vs. 2.57), but metropolitan areas recorded more deaths (100,560, AAPC: -1.42, p=0.003). Southern and Midwestern states, especially South Carolina (3.95), Kentucky (3.94), and Mississippi (3.74), had the highest AAMRs. In contrast, states like New York (2.00), Massachusetts (2.24), and Pennsylvania (2.40) had lower-than-average mortality.
Discussion: Although mortality due to AP has slightly declined over the past 25 years, significant demographic, regional, and healthcare access disparities persist, underscoring the need for equity-focused interventions in high-risk and geographically vulnerable areas.
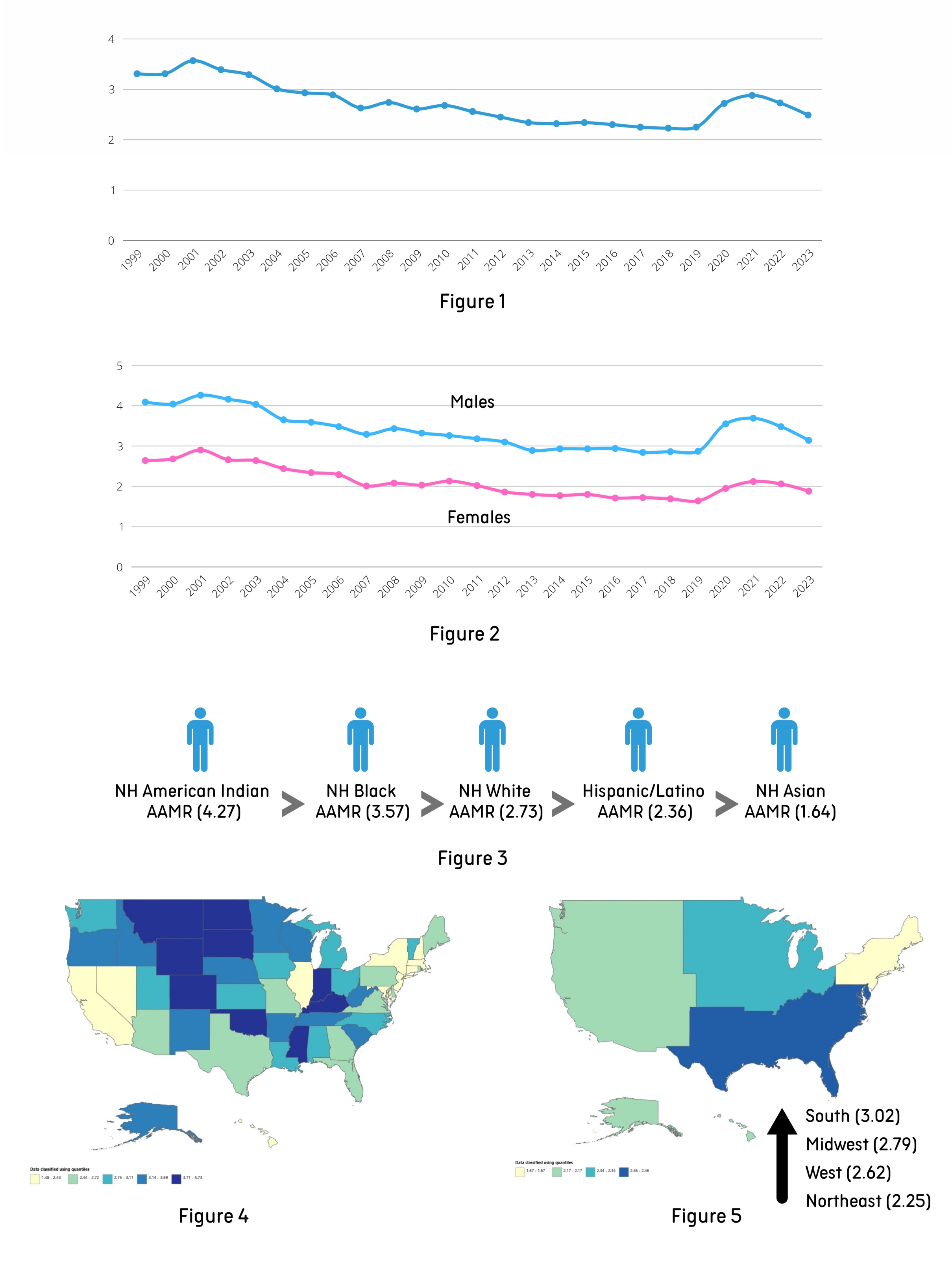
Figure: Figure 1: Overall Age-adjusted Mortality Rates per 100,000 persons
Figure 2: Sex-stratified Trends (Age-adjusted Mortality Rates per 100,000 persons)
Figure 3: Racial Disparities (Age-adjusted Mortality Rates per 100,000 persons)
Figure 4: State-stratified Trends (Age-adjusted Mortality Rates per 100,000 persons)
Figure 5: Census Region-stratified Trends (Age-adjusted Mortality Rates per 100,000 persons)
Disclosures:
Maryam Saghir indicated no relevant financial relationships.
Eshal Saghir indicated no relevant financial relationships.
Maham Maqsood indicated no relevant financial relationships.
Amjad Zafar indicated no relevant financial relationships.
Sahil Jairamani indicated no relevant financial relationships.
Maha Sajjad indicated no relevant financial relationships.
Maryam Saghir, MBBS1, Eshal Saghir, MBBS2, Maham Maqsood, MBBS3, Amjad Zafar, MBBS4, Sahil Jairamani, MBBS5, Maha Sajjad, MBBS6. P4324 - Trends in Acute Pancreatitis Hospitalization and In-Hospital Mortality in the United States (1999-2023): Evaluating the Role of Healthcare Access and Regional Disparities, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
