Tuesday Poster Session
Category: Biliary/Pancreas
P4321 - Comparative Risk of Acute Pancreatitis in Hypertriglyceridemia Patients Treated With SGLT2 Inhibitors vs GLP-1 Receptor Agonists: A Propensity-Score Matched Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ibrahim Shanti, MD (he/him/his)
Marshall University - - Huntington, WV
Huntington, WV
Presenting Author(s)
Ibrahim Shanti, MD1, Abdallah Hussein, MD2, Islam Rajab, MD3, Bisher Mustafa, MD4, Wesam Frandah, MD5, Ahmed Sherif, MD5
1Marshall University - - Huntington, WV, Huntington, WV; 2Virtua Our Lady of Lourdes Hospital, Camden, NJ; 3St. Joseph's University Medical Center, Paterson, NJ; 4Joan C. Edwards School of Medicine, Marshall University, Huntington, WV; 5Marshall University Joan C. Edwards School of Medicine, Huntington, WV
Introduction: Sodium-glucose co-transporter 2 (SGLT2) inhibitors and glucagon-like peptide-1 receptor
agonists (GLP-1 RAs) are widely used antidiabetic agents with demonstrated cardiovascular
and renal benefits. However, their comparative safety profiles regarding pancreatitis and lipid
disorders remain underexplored. This study aimed to evaluate and compare the 1-year risk of
acute pancreatitis and hypertriglyceridemia among users of SGLT2 inhibitors and GLP-1
receptor agonists.
Methods: We performed a retrospective cohort analysis using data from the TriNetX Research Network.
Adults who initiated either an SGLT2 inhibitor or a GLP-1 receptor agonist were identified and
followed for one year. After 1:1 propensity-score matching for baseline demographics and
comorbidities, 22,042 patients were included in each cohort. Primary outcomes were the
incidence of acute pancreatitis and hypertriglyceridemia, defined by ICD-10 codes. Risk
comparisons were assessed using odds ratios (ORs), risk differences, and Cox proportional
hazards models adjusted for medication type.
Results: In propensity-score–matched cohorts of 22,042 patients per arm, the incidence of acute
pancreatitis was higher in patients treated with SGLT2 inhibitors compared to GLP-1
receptor agonists, acute pancreatitis occurred in 0.349% of the SGLT2 users versus
0.263% of the GLP-1 RA(OR 1.33, 95% CI 0.95–1.87; P = 0.10).
In a multivariable Cox regression analysis adjusting for individual medications, For SGLT2
inhibitors, the adjusted hazard ratios were: canagliflozin (aHR < 0.0001, 95% CI 0–0; P =
0.9844), dapagliflozin (aHR 1.22, 95% CI 0.45–3.28; P = 0.6982), empagliflozin (aHR 0.77, 95%
CI 0.34–1.73; P = 0.5249), and ertugliflozin (aHR < 0.0001, 95% CI 0–0; P = 0.9954). For
GLP-1 receptor agonists, results included: albiglutide (aHR < 0.0001, 95% CI 0–0; P = 0.9962),
dulaglutide (aHR 1.19, 95% CI 0.63–2.25; P = 0.5968), semaglutide (aHR 1.58, 95% CI
0.81–3.10; P = 0.1808), liraglutide (aHR 0.59, 95% CI 0.24–1.45; P = 0.2501), and exenatide
(aHR 0.30, 95% CI 0.04–2.17; P = 0.2348).
Discussion: In this large real-world matched cohort study, the risk of acute pancreatitis and
hypertriglyceridemia did not differ significantly between SGLT2 inhibitor and GLP-1 receptor
agonist users. While male sex and older age were independently associated with pancreatitis
risk, no individual agent demonstrated a statistically significant association. These findings
support the pancreatic safety of both classes in routine practice.
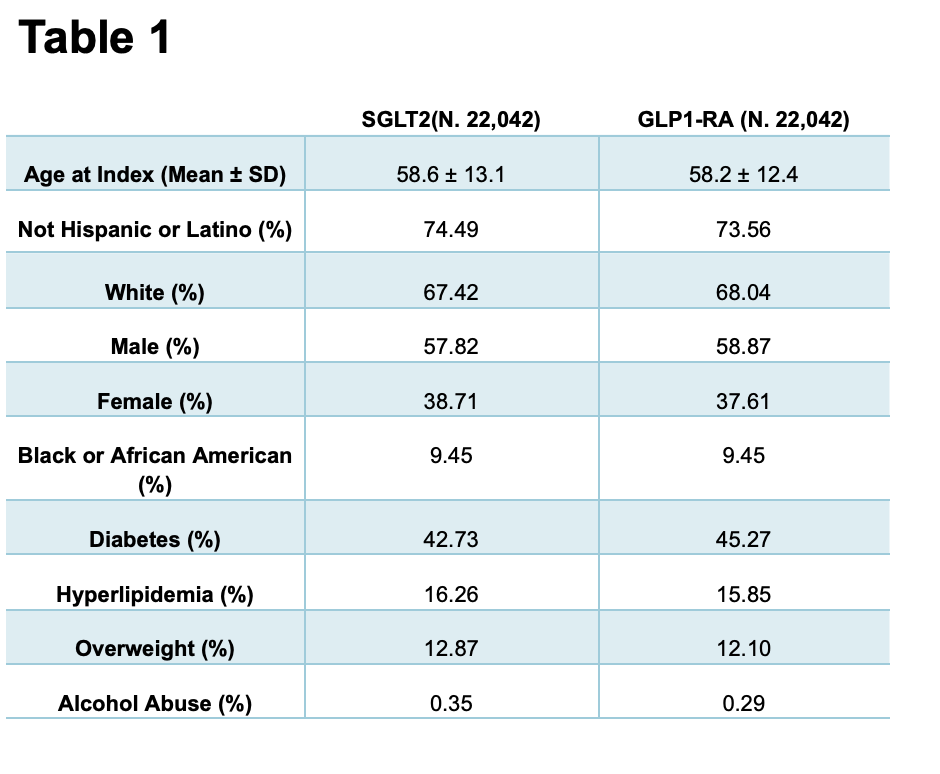
Figure: Table 1: Baseline Demographic and Clinical Characteristics of Patients Treated with SGLT2 Inhibitors vs. GLP1 Receptor Agonists
Disclosures:
Ibrahim Shanti indicated no relevant financial relationships.
Abdallah Hussein indicated no relevant financial relationships.
Islam Rajab indicated no relevant financial relationships.
Bisher Mustafa indicated no relevant financial relationships.
Wesam Frandah: Boston Scientific – Advisor or Review Panel Member, Consultant. Merritt – Consultant. Olympus corporation of America – Consultant.
Ahmed Sherif indicated no relevant financial relationships.
Ibrahim Shanti, MD1, Abdallah Hussein, MD2, Islam Rajab, MD3, Bisher Mustafa, MD4, Wesam Frandah, MD5, Ahmed Sherif, MD5. P4321 - Comparative Risk of Acute Pancreatitis in Hypertriglyceridemia Patients Treated With SGLT2 Inhibitors vs GLP-1 Receptor Agonists: A Propensity-Score Matched Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Marshall University - - Huntington, WV, Huntington, WV; 2Virtua Our Lady of Lourdes Hospital, Camden, NJ; 3St. Joseph's University Medical Center, Paterson, NJ; 4Joan C. Edwards School of Medicine, Marshall University, Huntington, WV; 5Marshall University Joan C. Edwards School of Medicine, Huntington, WV
Introduction: Sodium-glucose co-transporter 2 (SGLT2) inhibitors and glucagon-like peptide-1 receptor
agonists (GLP-1 RAs) are widely used antidiabetic agents with demonstrated cardiovascular
and renal benefits. However, their comparative safety profiles regarding pancreatitis and lipid
disorders remain underexplored. This study aimed to evaluate and compare the 1-year risk of
acute pancreatitis and hypertriglyceridemia among users of SGLT2 inhibitors and GLP-1
receptor agonists.
Methods: We performed a retrospective cohort analysis using data from the TriNetX Research Network.
Adults who initiated either an SGLT2 inhibitor or a GLP-1 receptor agonist were identified and
followed for one year. After 1:1 propensity-score matching for baseline demographics and
comorbidities, 22,042 patients were included in each cohort. Primary outcomes were the
incidence of acute pancreatitis and hypertriglyceridemia, defined by ICD-10 codes. Risk
comparisons were assessed using odds ratios (ORs), risk differences, and Cox proportional
hazards models adjusted for medication type.
Results: In propensity-score–matched cohorts of 22,042 patients per arm, the incidence of acute
pancreatitis was higher in patients treated with SGLT2 inhibitors compared to GLP-1
receptor agonists, acute pancreatitis occurred in 0.349% of the SGLT2 users versus
0.263% of the GLP-1 RA(OR 1.33, 95% CI 0.95–1.87; P = 0.10).
In a multivariable Cox regression analysis adjusting for individual medications, For SGLT2
inhibitors, the adjusted hazard ratios were: canagliflozin (aHR < 0.0001, 95% CI 0–0; P =
0.9844), dapagliflozin (aHR 1.22, 95% CI 0.45–3.28; P = 0.6982), empagliflozin (aHR 0.77, 95%
CI 0.34–1.73; P = 0.5249), and ertugliflozin (aHR < 0.0001, 95% CI 0–0; P = 0.9954). For
GLP-1 receptor agonists, results included: albiglutide (aHR < 0.0001, 95% CI 0–0; P = 0.9962),
dulaglutide (aHR 1.19, 95% CI 0.63–2.25; P = 0.5968), semaglutide (aHR 1.58, 95% CI
0.81–3.10; P = 0.1808), liraglutide (aHR 0.59, 95% CI 0.24–1.45; P = 0.2501), and exenatide
(aHR 0.30, 95% CI 0.04–2.17; P = 0.2348).
Discussion: In this large real-world matched cohort study, the risk of acute pancreatitis and
hypertriglyceridemia did not differ significantly between SGLT2 inhibitor and GLP-1 receptor
agonist users. While male sex and older age were independently associated with pancreatitis
risk, no individual agent demonstrated a statistically significant association. These findings
support the pancreatic safety of both classes in routine practice.
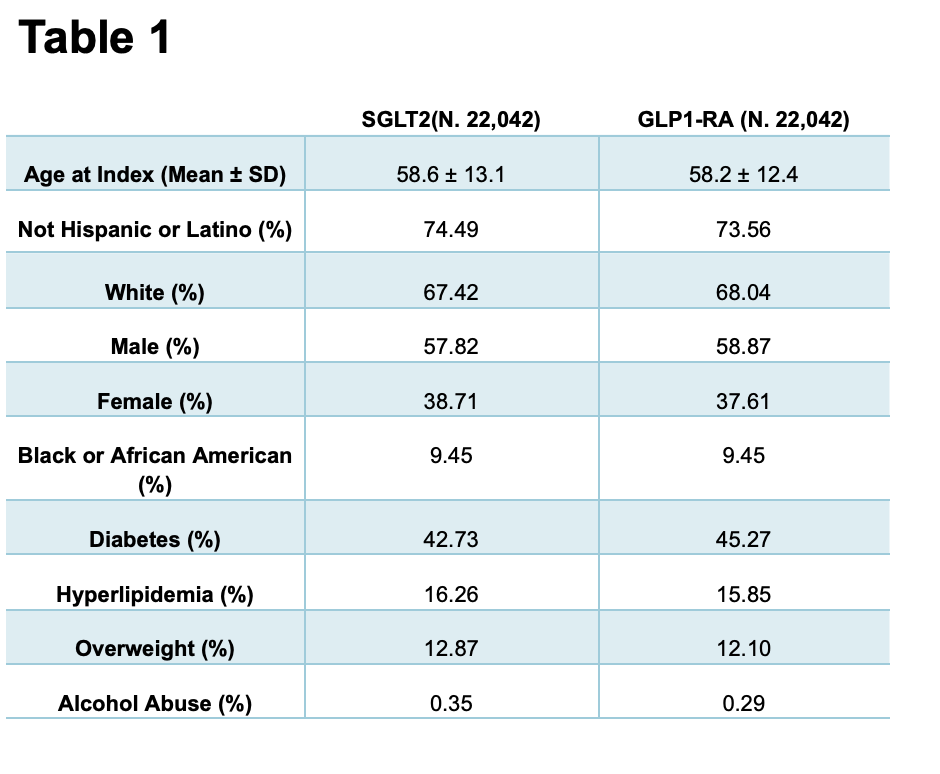
Figure: Table 1: Baseline Demographic and Clinical Characteristics of Patients Treated with SGLT2 Inhibitors vs. GLP1 Receptor Agonists
Disclosures:
Ibrahim Shanti indicated no relevant financial relationships.
Abdallah Hussein indicated no relevant financial relationships.
Islam Rajab indicated no relevant financial relationships.
Bisher Mustafa indicated no relevant financial relationships.
Wesam Frandah: Boston Scientific – Advisor or Review Panel Member, Consultant. Merritt – Consultant. Olympus corporation of America – Consultant.
Ahmed Sherif indicated no relevant financial relationships.
Ibrahim Shanti, MD1, Abdallah Hussein, MD2, Islam Rajab, MD3, Bisher Mustafa, MD4, Wesam Frandah, MD5, Ahmed Sherif, MD5. P4321 - Comparative Risk of Acute Pancreatitis in Hypertriglyceridemia Patients Treated With SGLT2 Inhibitors vs GLP-1 Receptor Agonists: A Propensity-Score Matched Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
