Tuesday Poster Session
Category: Biliary/Pancreas
P4320 - SGLT2 Inhibitors and Chronic Pancreatitis: A Protective Twist in Pancreatic Outcomes
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Victor Osio, MD
Wayne State University School of Medicine / Detroit Medical Center
Detroit, MI
Presenting Author(s)
Victor Osio, MD1, Sahith Kaki, BS2, Chidera Onwuzo, MBBS3, Rashid Abdel-Razeq, MD4, James Rock, DO5, Ellen C. Tan, DO5, Jacob Newman, DO5, Somtochukwu Onwuzo, MD6
1Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 2Lake Erie College of Osteopathic Medicine - Erie, Erie, PA; 3SUNY Upstate Medical University Hospital, Syracuse, NY; 4Cleveland Clinic Foundation, Cleveland, OH; 5Allegheny Health Network, Pittsburgh, PA; 6Allegheny Center for Digestive Health, Pittsburgh, PA
Introduction: Chronic pancreatitis (CP) is a progressive inflammatory disease associated with complications such as exocrine pancreatic insufficiency, pseudocysts, malignancy, and increased mortality. SGLT2 inhibitors have demonstrated anti-inflammatory and antifibrotic properties in preclinical models, but their effect on pancreatic outcomes in CP remains unclear. This study aimed to evaluate whether SGLT2 inhibitor use is associated with improved pancreatic outcomes in patients with CP.
Methods: A validated, multicenter research platform database encompassing more than 70 healthcare systems and over 130 million patients across the United States was utilized to construct this study. Cohort 1 included patients aged 18–65 years with chronic pancreatitis on SGLT2 inhibitors (N = 7,906), while Cohort 2 included patients with chronic pancreatitis not on SGLT2 inhibitors (N = 131,909). Propensity score matching (1:1) was performed, adjusting for demographics and comorbidities. Outcomes assessed included exocrine pancreatic insufficiency, pancreatic stones, pancreatic pseudocysts, pancreatic cancer, and mortality.
Results: After matching, 7,446 patients remained in each group. SGLT2 inhibitor use was associated with reduced risks of exocrine pancreatic insufficiency (5.3% vs. 7.3%; OR 0.71; p < 0.001), pancreatic pseudocysts (2.7% vs. 4.6%; OR 0.58; p < 0.001), pancreatic cancer (1.3% vs. 2.3%; OR 0.58; p < 0.001), and mortality (7.0% vs. 12.7%; OR 0.52; p < 0.001). There was no significant difference in the risk of pancreatic stones (0.3% vs. 0.4%; OR 0.84; p = 0.51). Kaplan–Meier analysis confirmed higher survival probabilities for SGLT2 users across all outcomes except stone formation.
Discussion: SGLT2 inhibitor use was associated with significantly improved pancreatic outcomes and reduced all-cause mortality in patients with chronic pancreatitis. These findings suggest a potential protective role and raise important questions about the broader therapeutic applications of SGLT2 inhibitors in this population. Further studies are warranted to confirm these associations and evaluate their potential as disease-modifying agents.
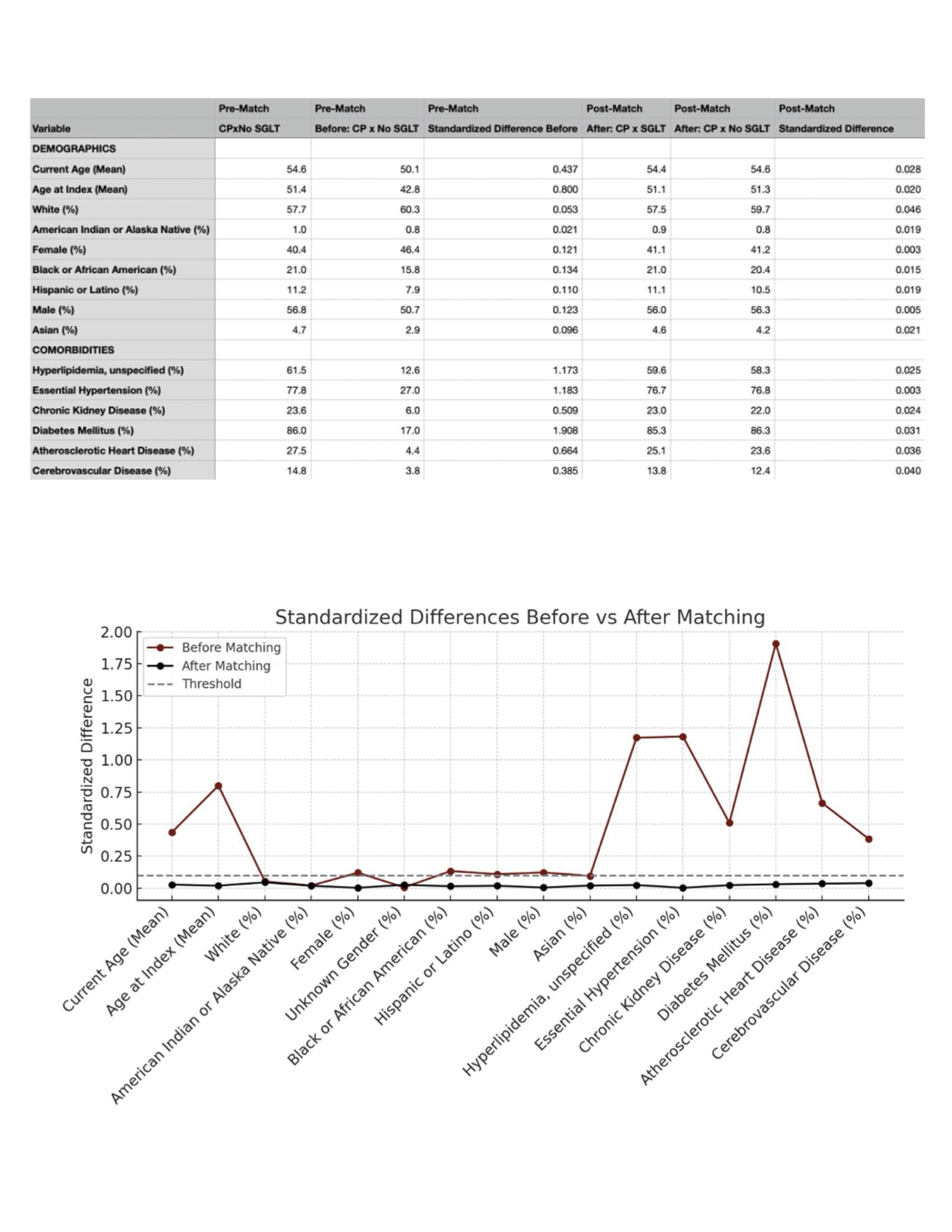
Figure: Table 1: Baseline characteristics of study population before and after matching
Figure 1: Linear graph depicting standardized difference before and after matching
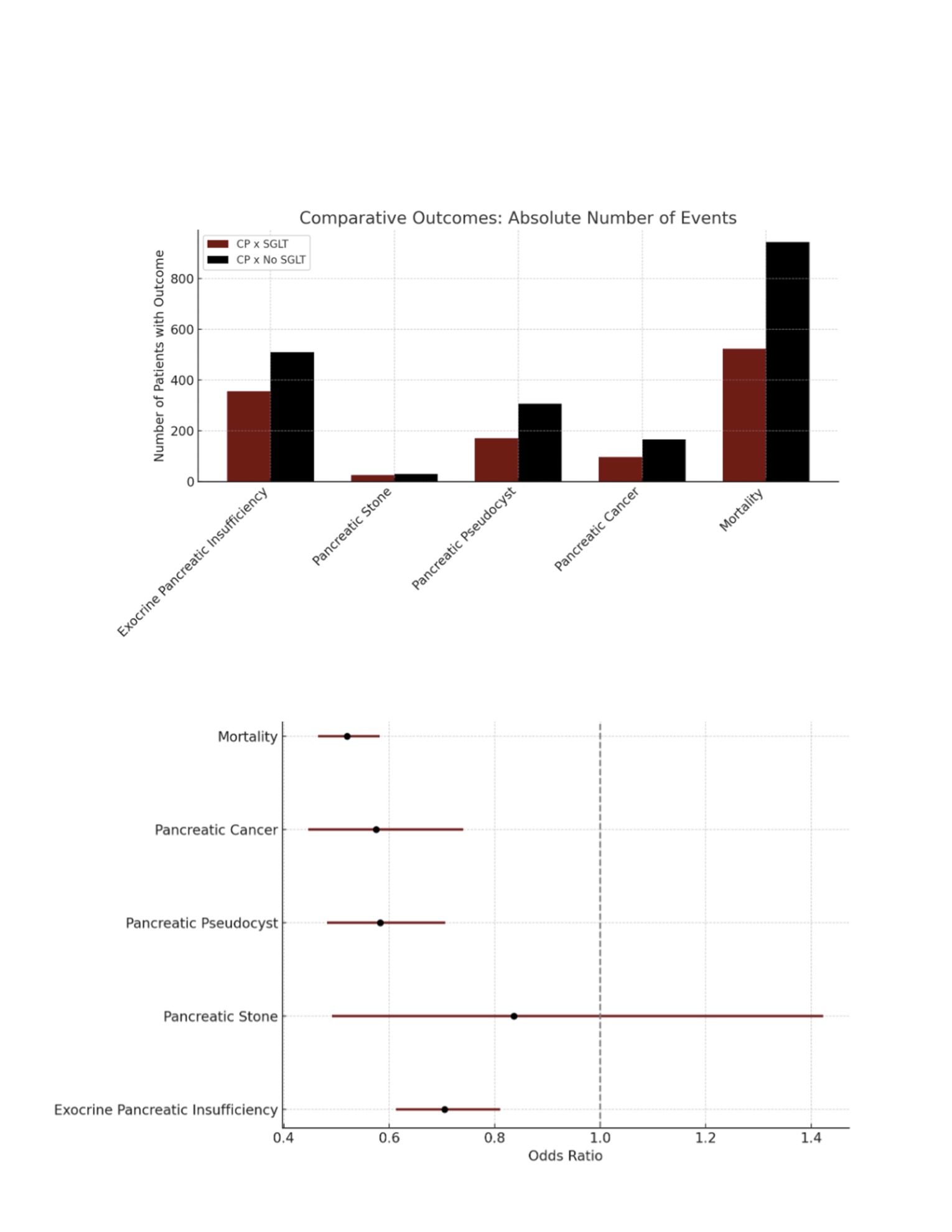
Figure: Figure 2: Bar chart showing number of adverse outcomes by cohort after matching
Figure 3: Forest plot showing Odds ratios with 95% confidence intervals for each outcome, comparing SGLT2 inhibitor users to non-users
Disclosures:
Victor Osio indicated no relevant financial relationships.
Sahith Kaki indicated no relevant financial relationships.
Chidera Onwuzo indicated no relevant financial relationships.
Rashid Abdel-Razeq indicated no relevant financial relationships.
James Rock indicated no relevant financial relationships.
Ellen Tan indicated no relevant financial relationships.
Jacob Newman indicated no relevant financial relationships.
Somtochukwu Onwuzo indicated no relevant financial relationships.
Victor Osio, MD1, Sahith Kaki, BS2, Chidera Onwuzo, MBBS3, Rashid Abdel-Razeq, MD4, James Rock, DO5, Ellen C. Tan, DO5, Jacob Newman, DO5, Somtochukwu Onwuzo, MD6. P4320 - SGLT2 Inhibitors and Chronic Pancreatitis: A Protective Twist in Pancreatic Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 2Lake Erie College of Osteopathic Medicine - Erie, Erie, PA; 3SUNY Upstate Medical University Hospital, Syracuse, NY; 4Cleveland Clinic Foundation, Cleveland, OH; 5Allegheny Health Network, Pittsburgh, PA; 6Allegheny Center for Digestive Health, Pittsburgh, PA
Introduction: Chronic pancreatitis (CP) is a progressive inflammatory disease associated with complications such as exocrine pancreatic insufficiency, pseudocysts, malignancy, and increased mortality. SGLT2 inhibitors have demonstrated anti-inflammatory and antifibrotic properties in preclinical models, but their effect on pancreatic outcomes in CP remains unclear. This study aimed to evaluate whether SGLT2 inhibitor use is associated with improved pancreatic outcomes in patients with CP.
Methods: A validated, multicenter research platform database encompassing more than 70 healthcare systems and over 130 million patients across the United States was utilized to construct this study. Cohort 1 included patients aged 18–65 years with chronic pancreatitis on SGLT2 inhibitors (N = 7,906), while Cohort 2 included patients with chronic pancreatitis not on SGLT2 inhibitors (N = 131,909). Propensity score matching (1:1) was performed, adjusting for demographics and comorbidities. Outcomes assessed included exocrine pancreatic insufficiency, pancreatic stones, pancreatic pseudocysts, pancreatic cancer, and mortality.
Results: After matching, 7,446 patients remained in each group. SGLT2 inhibitor use was associated with reduced risks of exocrine pancreatic insufficiency (5.3% vs. 7.3%; OR 0.71; p < 0.001), pancreatic pseudocysts (2.7% vs. 4.6%; OR 0.58; p < 0.001), pancreatic cancer (1.3% vs. 2.3%; OR 0.58; p < 0.001), and mortality (7.0% vs. 12.7%; OR 0.52; p < 0.001). There was no significant difference in the risk of pancreatic stones (0.3% vs. 0.4%; OR 0.84; p = 0.51). Kaplan–Meier analysis confirmed higher survival probabilities for SGLT2 users across all outcomes except stone formation.
Discussion: SGLT2 inhibitor use was associated with significantly improved pancreatic outcomes and reduced all-cause mortality in patients with chronic pancreatitis. These findings suggest a potential protective role and raise important questions about the broader therapeutic applications of SGLT2 inhibitors in this population. Further studies are warranted to confirm these associations and evaluate their potential as disease-modifying agents.
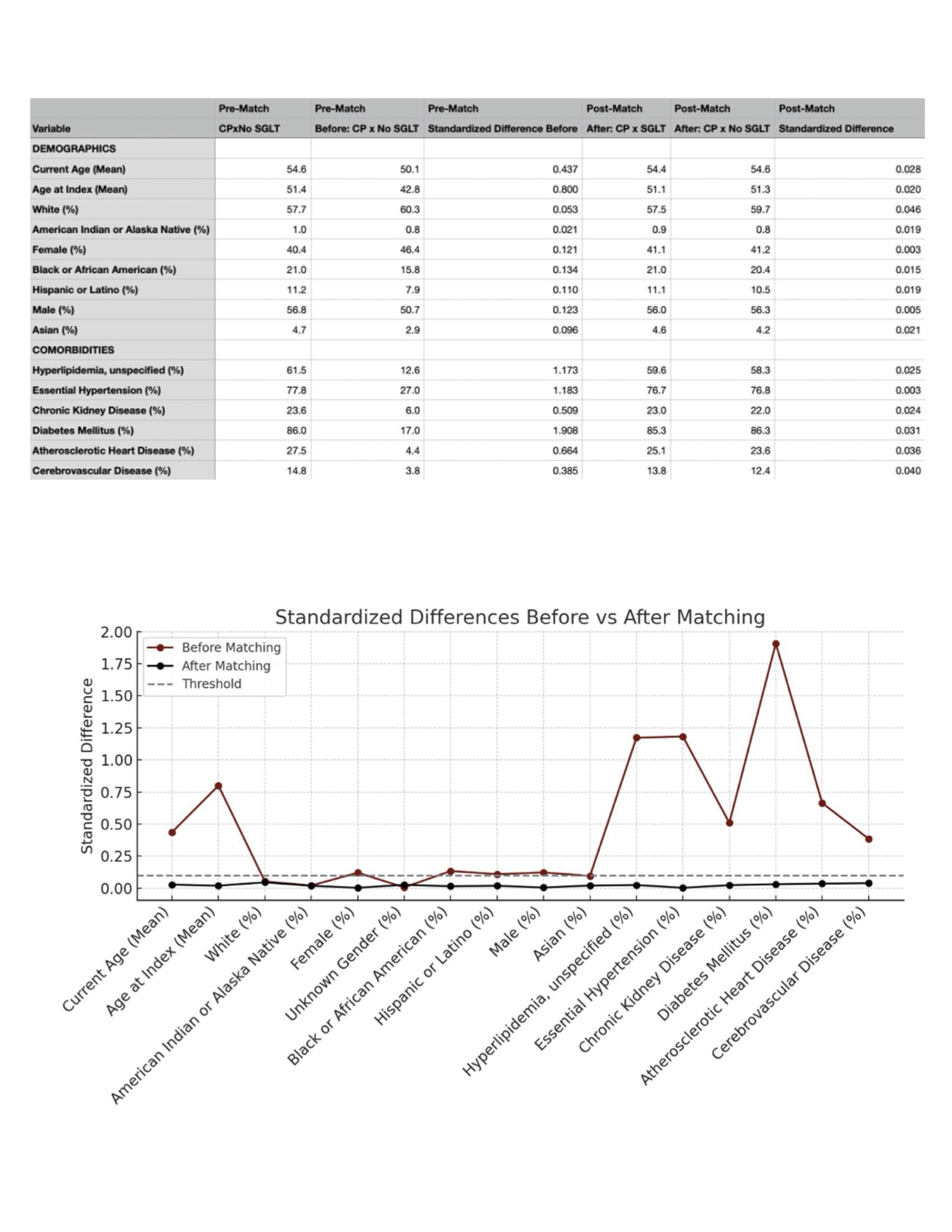
Figure: Table 1: Baseline characteristics of study population before and after matching
Figure 1: Linear graph depicting standardized difference before and after matching
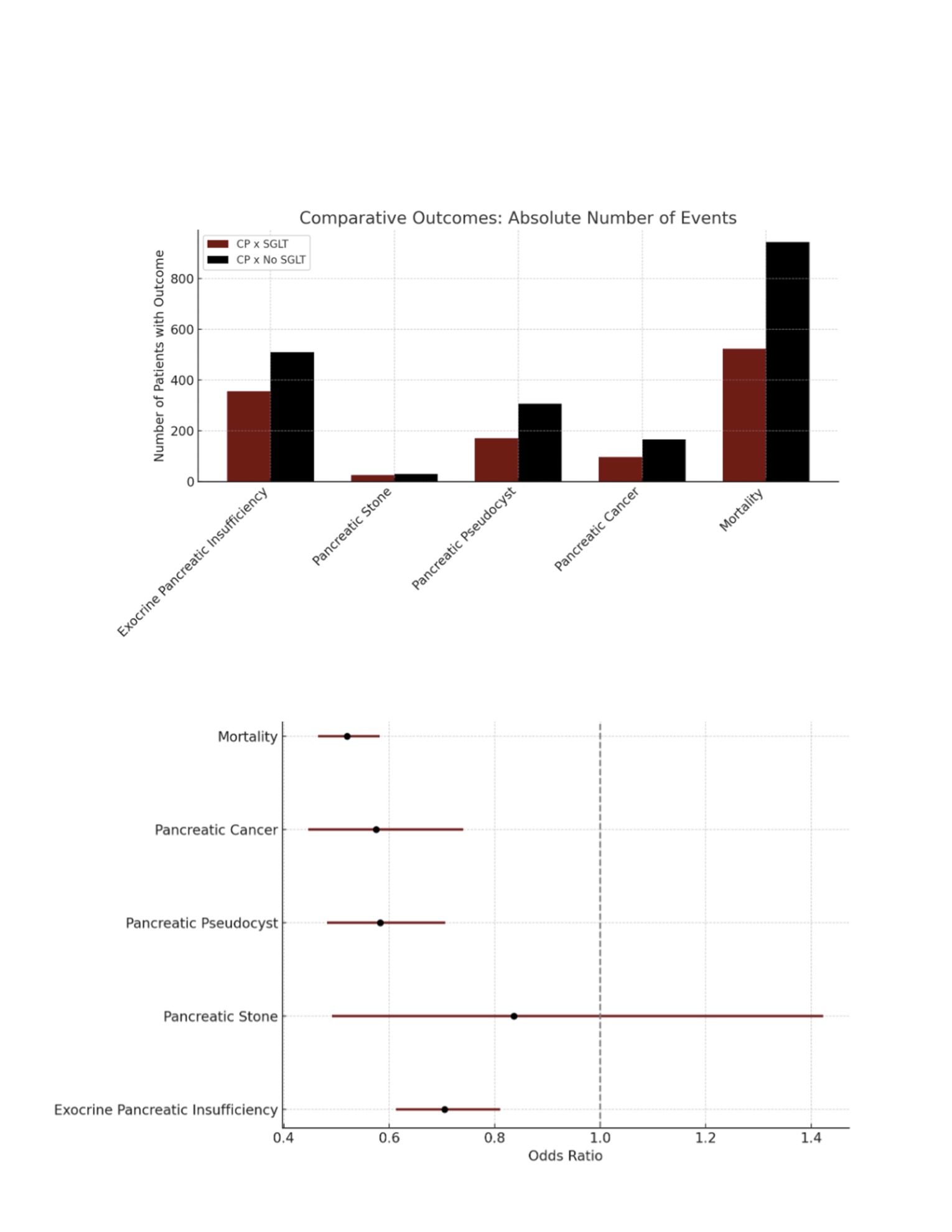
Figure: Figure 2: Bar chart showing number of adverse outcomes by cohort after matching
Figure 3: Forest plot showing Odds ratios with 95% confidence intervals for each outcome, comparing SGLT2 inhibitor users to non-users
Disclosures:
Victor Osio indicated no relevant financial relationships.
Sahith Kaki indicated no relevant financial relationships.
Chidera Onwuzo indicated no relevant financial relationships.
Rashid Abdel-Razeq indicated no relevant financial relationships.
James Rock indicated no relevant financial relationships.
Ellen Tan indicated no relevant financial relationships.
Jacob Newman indicated no relevant financial relationships.
Somtochukwu Onwuzo indicated no relevant financial relationships.
Victor Osio, MD1, Sahith Kaki, BS2, Chidera Onwuzo, MBBS3, Rashid Abdel-Razeq, MD4, James Rock, DO5, Ellen C. Tan, DO5, Jacob Newman, DO5, Somtochukwu Onwuzo, MD6. P4320 - SGLT2 Inhibitors and Chronic Pancreatitis: A Protective Twist in Pancreatic Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
