Tuesday Poster Session
Category: Biliary/Pancreas
P4315 - Association of Acute Pancreatitis Severity With Risk of New Onset Prediabetes and Diabetes: A Large Real-World Evidence Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- DB
Djibril M. Ba, PhD
Penn State College of Medicine
Hershey, PA
Presenting Author(s)
Djibril M. Ba, PhD1, Ariana Pichardo-Lowden, MD1, David Bradley, MD, MS1, Tian Qiu, MPH1, Yue Zhang, PhD2, Anna Marrie. Cozzi, MPH1, Jennifer Maranki, MD1, Vernon M. Chinchilli, PhD1
1Penn State College of Medicine, Hershey, PA; 2Johns Hopkins Bloomberg School of Public Health, Baltimore, MD
Introduction: Acute pancreatitis (AP) is the third most common gastrointestinal disease in the U.S., accounting for over 300,000 hospitalizations each year. Patients with AP are at a higher risk of developing prediabetes or diabetes mellitus (DM) than those without AP; however, it remains unclear whether the severity of AP influences this risk. The objective of this study was to investigate the associations of AP severity with the risk of prediabetes and DM using real-world data.
Methods: We conducted a retrospective cohort study using the MerativeTM MarketScan® claims database (2016-2022), identifying patients with AP (diagnosed using ICD-10 code: K85) continuously enrolled in the database with no prior history of prediabetes (ICD-10 codes: R73.03, R73.09, R73.01, R73.02) and DM diagnosis (ICD-10 codes: E08-E14) at the study baseline. Severe AP was defined as any of the following within 30 days following the index AP event: ICU admission using revenue codes 0200–0209, or organ failure (ICD-10 codes: N17, J96.0, R57, K85.91, K86.3, A41, R65.2). Mild AP was defined as the absence of any of the above codes during the same period. To reduce the influence of AP, illness-related, and canonical diabetes risk confounding factors and balance characteristics between the two groups (Figure 1), we conducted a propensity score matching using a greedy nearest neighbor approach in conjunction with a 2:1 matching ratio without replacement. Multivariable stratified Cox proportional hazards regression analysis was conducted to determine the association of AP severity with prediabetes and diabetes.
Results: The matched study cohort included 3,554 patients with severe AP and 7,108 patients with mild AP, all aged 18-64 years, with baseline characteristics well balanced between groups, as indicated by standardized mean differences (SMD < 0.1; Figure 1). During six years of follow-up, there were 835 incidents of prediabetes and 833 cases of diabetes (Figure 2). In the stratified multivariable Cox proportional hazards models, severe AP compared to mild AP was associated with higher risk of (1) incident prediabetes, with an adjusted hazard ratio of 1.19 (95% confidence interval [CI], 1.01–1.40; P=0.04), and (2) incident diabetes, with an adjusted hazard ratio of 1.95 (95% CI, 1.66–2.28; P < .001).
Discussion: In this large real-world evidence study, severe AP was associated with a greater risk of new-onset prediabetes and diabetes. The association between the severity of AP and diabetes was nearly two-fold stronger.
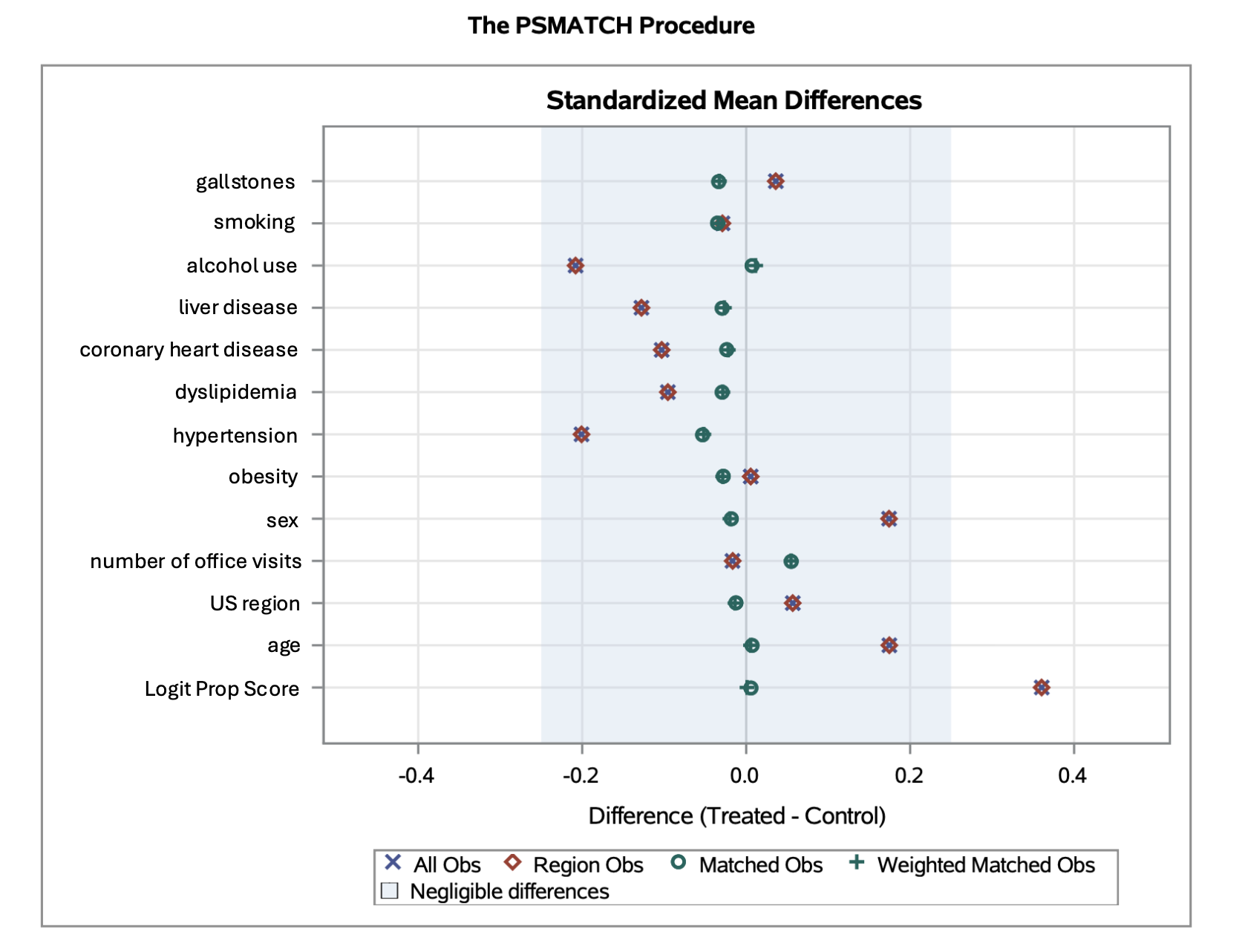
Figure: Figure 1. Propensity Score Matching Confounders

Figure: Figure 2. Kaplan Meier Survival Curves.
Disclosures:
Djibril Ba indicated no relevant financial relationships.
Ariana Pichardo-Lowden indicated no relevant financial relationships.
David Bradley indicated no relevant financial relationships.
Tian Qiu indicated no relevant financial relationships.
Yue Zhang indicated no relevant financial relationships.
Anna Cozzi indicated no relevant financial relationships.
Jennifer Maranki indicated no relevant financial relationships.
Vernon Chinchilli indicated no relevant financial relationships.
Djibril M. Ba, PhD1, Ariana Pichardo-Lowden, MD1, David Bradley, MD, MS1, Tian Qiu, MPH1, Yue Zhang, PhD2, Anna Marrie. Cozzi, MPH1, Jennifer Maranki, MD1, Vernon M. Chinchilli, PhD1. P4315 - Association of Acute Pancreatitis Severity With Risk of New Onset Prediabetes and Diabetes: A Large Real-World Evidence Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Penn State College of Medicine, Hershey, PA; 2Johns Hopkins Bloomberg School of Public Health, Baltimore, MD
Introduction: Acute pancreatitis (AP) is the third most common gastrointestinal disease in the U.S., accounting for over 300,000 hospitalizations each year. Patients with AP are at a higher risk of developing prediabetes or diabetes mellitus (DM) than those without AP; however, it remains unclear whether the severity of AP influences this risk. The objective of this study was to investigate the associations of AP severity with the risk of prediabetes and DM using real-world data.
Methods: We conducted a retrospective cohort study using the MerativeTM MarketScan® claims database (2016-2022), identifying patients with AP (diagnosed using ICD-10 code: K85) continuously enrolled in the database with no prior history of prediabetes (ICD-10 codes: R73.03, R73.09, R73.01, R73.02) and DM diagnosis (ICD-10 codes: E08-E14) at the study baseline. Severe AP was defined as any of the following within 30 days following the index AP event: ICU admission using revenue codes 0200–0209, or organ failure (ICD-10 codes: N17, J96.0, R57, K85.91, K86.3, A41, R65.2). Mild AP was defined as the absence of any of the above codes during the same period. To reduce the influence of AP, illness-related, and canonical diabetes risk confounding factors and balance characteristics between the two groups (Figure 1), we conducted a propensity score matching using a greedy nearest neighbor approach in conjunction with a 2:1 matching ratio without replacement. Multivariable stratified Cox proportional hazards regression analysis was conducted to determine the association of AP severity with prediabetes and diabetes.
Results: The matched study cohort included 3,554 patients with severe AP and 7,108 patients with mild AP, all aged 18-64 years, with baseline characteristics well balanced between groups, as indicated by standardized mean differences (SMD < 0.1; Figure 1). During six years of follow-up, there were 835 incidents of prediabetes and 833 cases of diabetes (Figure 2). In the stratified multivariable Cox proportional hazards models, severe AP compared to mild AP was associated with higher risk of (1) incident prediabetes, with an adjusted hazard ratio of 1.19 (95% confidence interval [CI], 1.01–1.40; P=0.04), and (2) incident diabetes, with an adjusted hazard ratio of 1.95 (95% CI, 1.66–2.28; P < .001).
Discussion: In this large real-world evidence study, severe AP was associated with a greater risk of new-onset prediabetes and diabetes. The association between the severity of AP and diabetes was nearly two-fold stronger.
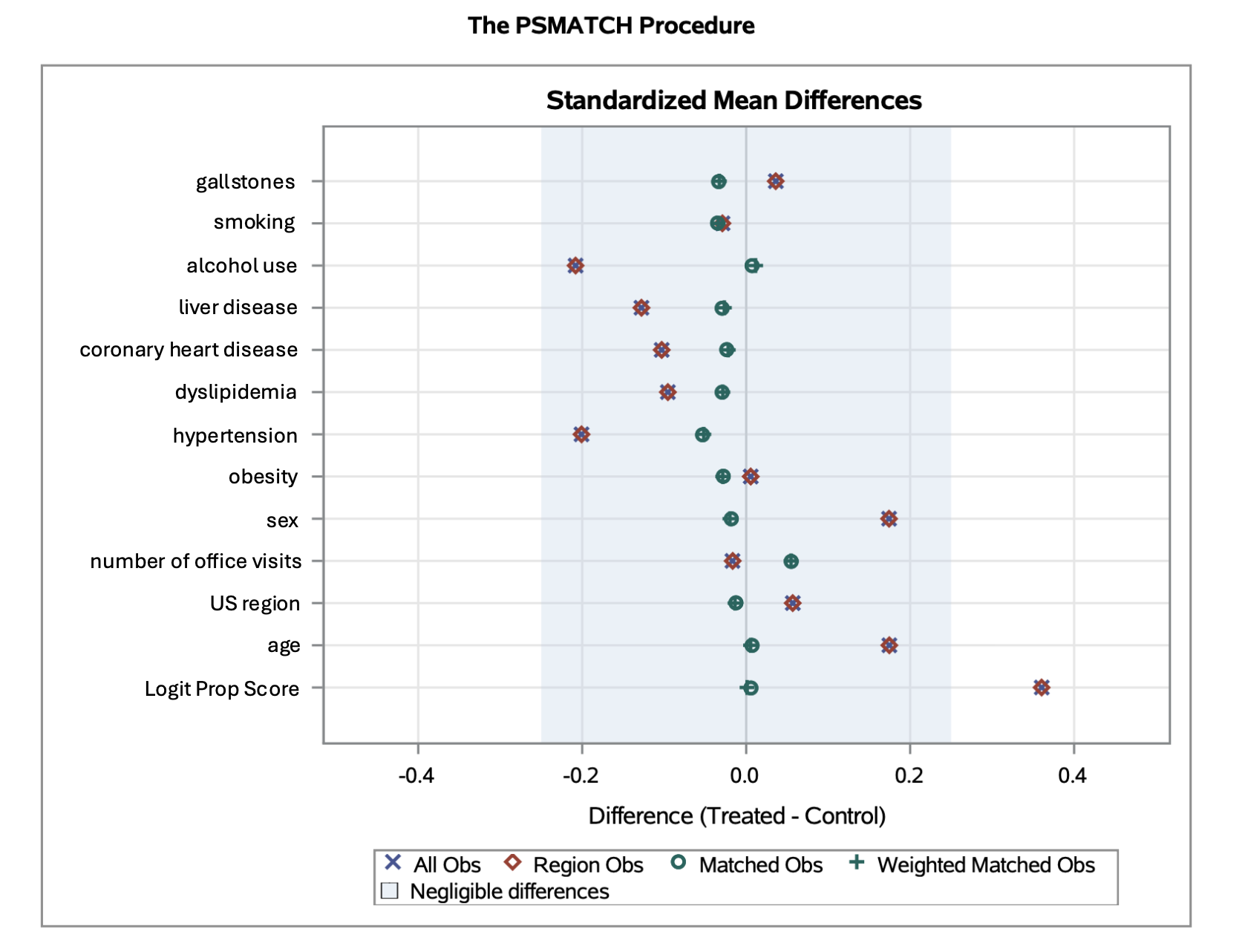
Figure: Figure 1. Propensity Score Matching Confounders

Figure: Figure 2. Kaplan Meier Survival Curves.
Disclosures:
Djibril Ba indicated no relevant financial relationships.
Ariana Pichardo-Lowden indicated no relevant financial relationships.
David Bradley indicated no relevant financial relationships.
Tian Qiu indicated no relevant financial relationships.
Yue Zhang indicated no relevant financial relationships.
Anna Cozzi indicated no relevant financial relationships.
Jennifer Maranki indicated no relevant financial relationships.
Vernon Chinchilli indicated no relevant financial relationships.
Djibril M. Ba, PhD1, Ariana Pichardo-Lowden, MD1, David Bradley, MD, MS1, Tian Qiu, MPH1, Yue Zhang, PhD2, Anna Marrie. Cozzi, MPH1, Jennifer Maranki, MD1, Vernon M. Chinchilli, PhD1. P4315 - Association of Acute Pancreatitis Severity With Risk of New Onset Prediabetes and Diabetes: A Large Real-World Evidence Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
