Tuesday Poster Session
Category: Biliary/Pancreas
P4301 - Outcomes of Acute Pancreatitis in Lean vs Non-Lean MASLD Patients: A Nationwide Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Prince A. Ameyaw, MD (he/him/his)
Yale New Haven Health, Bridgeport Hospital
Bridgeport, CT
Presenting Author(s)
Prince A. Ameyaw, MD1, Sarpong Boateng, MD, MPH2, Erika Sandra Ackah, MBChB3, Amita Kasar, MD4, Yussif Issaka, MBChB5, Yazan Al Ajlouni, MD, Mphil6, Basile Njei, MD, PhD, MPH7
1Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 2Yale New Haven Health, Bridgeport, CT; 3Cape Coast Teaching Hospital, Cape Coast, Central, Ghana; 4Poplar Bluff Regional Medical center, Poplar Bluff, MO; 5Bridgeport Hospital, Bridgeport, CT; 6Montefiore Medical Center, New York, NY; 7VA Connecticut Healthcare System and Yale University, West Haven, CT
Introduction: Acute pancreatitis (AP) is a complex disease process characterized by pancreatic autodigestion resulting from pancreatic acinar cell damage. Host characteristics, risk stratification scoring systems, and clinical and laboratory evidence of response to therapy have been shown to predict outcomes in AP. Metabolic dysfunction-associated steatotic liver disease (MASLD) is a key contributor to the severity and outcomes of acute pancreatitis (AP). This study compares the clinical outcomes of AP in patients with lean versus non-lean MASLD
Methods: We identified adult patients (≥18 years) hospitalized with AP and a secondary diagnosis of MASLD from the National Inpatient Sample (NIS 2016-2020). Lean MASLD was operationalized as a subset of non-obese MASLD with a BMI < 25 kg/m². We excluded patients with an ICD-10-CM history of alcohol-related liver disease and viral hepatitis. Outcomes, including mortality, organ failures, medical interventions, length of stay, and healthcare costs, adjusted for inflation to 2020 dollars, were analyzed using multivariable logistic and linear regression models, adjusting for demographic, comorbidities, clinical, and hospital factors.
Results: We included 34,388 hospitalized patients with AP and MASLD, of whom 14,443 (42.0%) were non-lean. Annual admissions increased sharply in lean MASLD patients (5339 in 2016 to 8247 in 2020) compared to non-lean MASLD (2273 to 3635). Non-lean MASLD patients experienced higher inflation-adjusted hospital charges ($5,324.01; 95% CI: $3,273.42–$7,374.61, P < 0.01), a longer length of stay ((adjusted increase 0.25 days; 95% CI: 0.12–0.39, P < 0.05), increased odds of respiratory failure (aOR 4.60; 95% CI: 2.24–9.46, P < 0.01), sepsis (aOR 1.11; 95% CI: 1.00–1.23, P = 0.04), cholecystectomy (aOR 2.05; 95% CI: 1.92–2.19, P < 0.01), ERCP (aOR 1.42 95% CI: 1.11–1.82, P = 0.01) and MACE (aOR1.19; 95% CI:1.05-1.35, P< 0.01). Mortality did not differ significantly between groups (aOR 0.90; 95% CI: 0.69–1.17, P = 0.43). There was no statistically significant difference in decompensating liver events between lean and non-lean MASLD patients with cirrhosis (aOR 0.78; 95% CI: 0.61–1.00, P = 0.05).
Discussion: Our study suggests that lean MASLD patients with AP may experience a higher rate of hospital admissions and distinct clinical profiles, including a similar mortality risk compared to non-lean MASLD patients, indicating a complex relationship between AP outcomes and MASLD beyond BMI.
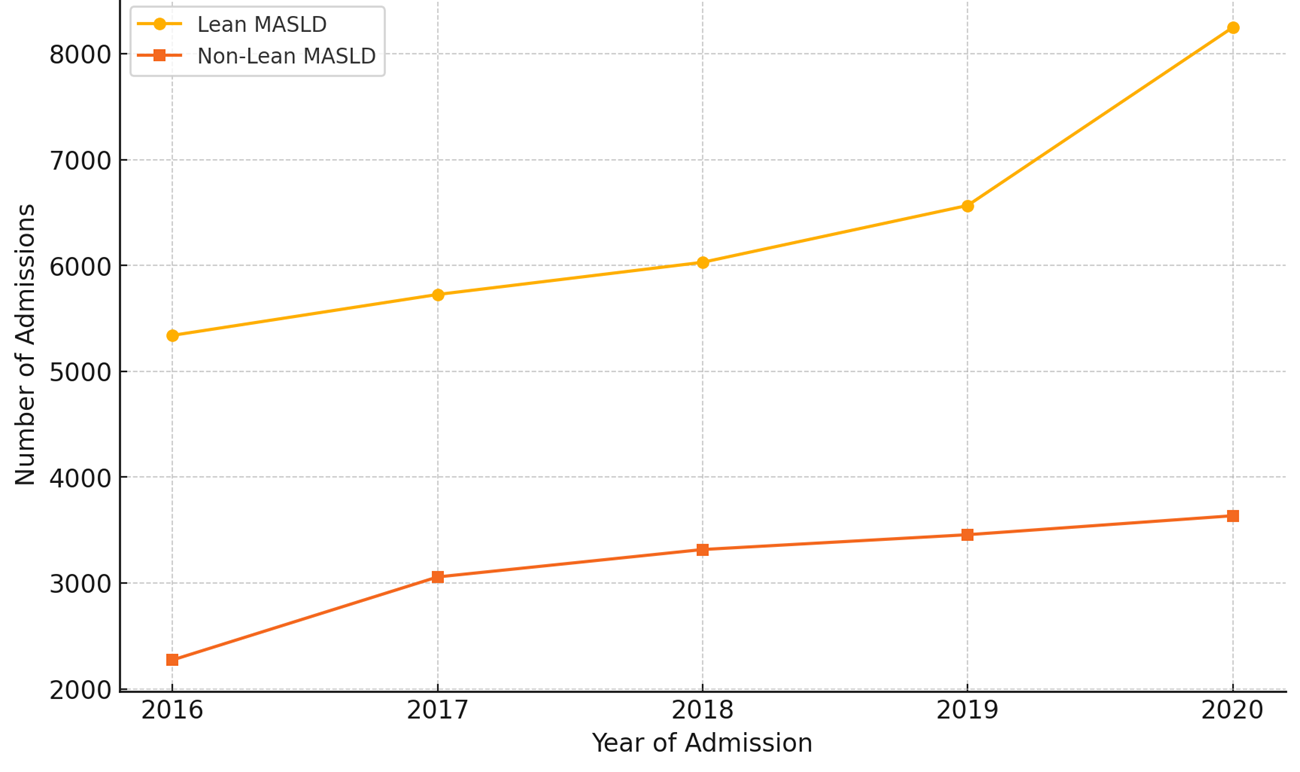
Figure: Yearly Admissions for Acute Pancreatitis with MASLD

Figure: Association between non-lean MASLD and outcomes of AP in US Hospitalized Adults
Disclosures:
Prince Ameyaw indicated no relevant financial relationships.
Sarpong Boateng indicated no relevant financial relationships.
Erika Sandra Ackah indicated no relevant financial relationships.
Amita Kasar indicated no relevant financial relationships.
Yussif Issaka indicated no relevant financial relationships.
Yazan Al Ajlouni indicated no relevant financial relationships.
Basile Njei indicated no relevant financial relationships.
Prince A. Ameyaw, MD1, Sarpong Boateng, MD, MPH2, Erika Sandra Ackah, MBChB3, Amita Kasar, MD4, Yussif Issaka, MBChB5, Yazan Al Ajlouni, MD, Mphil6, Basile Njei, MD, PhD, MPH7. P4301 - Outcomes of Acute Pancreatitis in Lean vs Non-Lean MASLD Patients: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 2Yale New Haven Health, Bridgeport, CT; 3Cape Coast Teaching Hospital, Cape Coast, Central, Ghana; 4Poplar Bluff Regional Medical center, Poplar Bluff, MO; 5Bridgeport Hospital, Bridgeport, CT; 6Montefiore Medical Center, New York, NY; 7VA Connecticut Healthcare System and Yale University, West Haven, CT
Introduction: Acute pancreatitis (AP) is a complex disease process characterized by pancreatic autodigestion resulting from pancreatic acinar cell damage. Host characteristics, risk stratification scoring systems, and clinical and laboratory evidence of response to therapy have been shown to predict outcomes in AP. Metabolic dysfunction-associated steatotic liver disease (MASLD) is a key contributor to the severity and outcomes of acute pancreatitis (AP). This study compares the clinical outcomes of AP in patients with lean versus non-lean MASLD
Methods: We identified adult patients (≥18 years) hospitalized with AP and a secondary diagnosis of MASLD from the National Inpatient Sample (NIS 2016-2020). Lean MASLD was operationalized as a subset of non-obese MASLD with a BMI < 25 kg/m². We excluded patients with an ICD-10-CM history of alcohol-related liver disease and viral hepatitis. Outcomes, including mortality, organ failures, medical interventions, length of stay, and healthcare costs, adjusted for inflation to 2020 dollars, were analyzed using multivariable logistic and linear regression models, adjusting for demographic, comorbidities, clinical, and hospital factors.
Results: We included 34,388 hospitalized patients with AP and MASLD, of whom 14,443 (42.0%) were non-lean. Annual admissions increased sharply in lean MASLD patients (5339 in 2016 to 8247 in 2020) compared to non-lean MASLD (2273 to 3635). Non-lean MASLD patients experienced higher inflation-adjusted hospital charges ($5,324.01; 95% CI: $3,273.42–$7,374.61, P < 0.01), a longer length of stay ((adjusted increase 0.25 days; 95% CI: 0.12–0.39, P < 0.05), increased odds of respiratory failure (aOR 4.60; 95% CI: 2.24–9.46, P < 0.01), sepsis (aOR 1.11; 95% CI: 1.00–1.23, P = 0.04), cholecystectomy (aOR 2.05; 95% CI: 1.92–2.19, P < 0.01), ERCP (aOR 1.42 95% CI: 1.11–1.82, P = 0.01) and MACE (aOR1.19; 95% CI:1.05-1.35, P< 0.01). Mortality did not differ significantly between groups (aOR 0.90; 95% CI: 0.69–1.17, P = 0.43). There was no statistically significant difference in decompensating liver events between lean and non-lean MASLD patients with cirrhosis (aOR 0.78; 95% CI: 0.61–1.00, P = 0.05).
Discussion: Our study suggests that lean MASLD patients with AP may experience a higher rate of hospital admissions and distinct clinical profiles, including a similar mortality risk compared to non-lean MASLD patients, indicating a complex relationship between AP outcomes and MASLD beyond BMI.
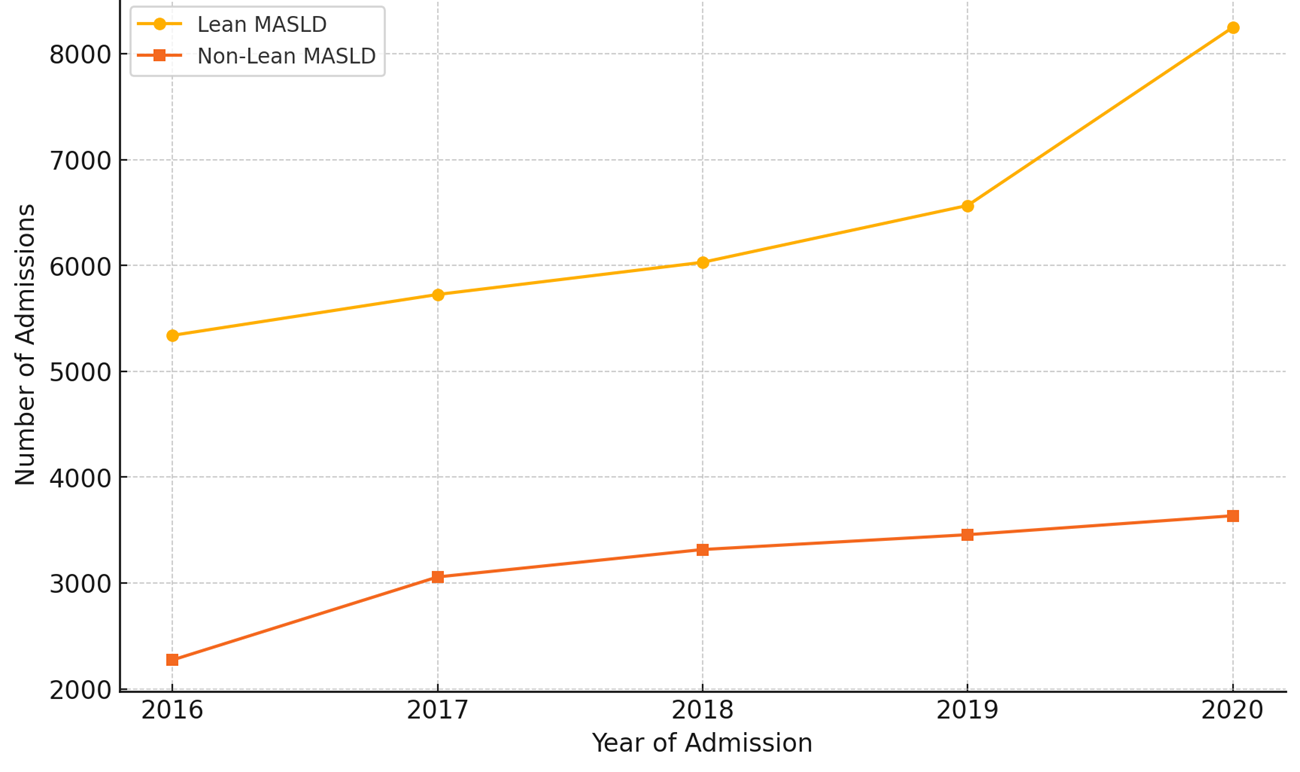
Figure: Yearly Admissions for Acute Pancreatitis with MASLD

Figure: Association between non-lean MASLD and outcomes of AP in US Hospitalized Adults
Disclosures:
Prince Ameyaw indicated no relevant financial relationships.
Sarpong Boateng indicated no relevant financial relationships.
Erika Sandra Ackah indicated no relevant financial relationships.
Amita Kasar indicated no relevant financial relationships.
Yussif Issaka indicated no relevant financial relationships.
Yazan Al Ajlouni indicated no relevant financial relationships.
Basile Njei indicated no relevant financial relationships.
Prince A. Ameyaw, MD1, Sarpong Boateng, MD, MPH2, Erika Sandra Ackah, MBChB3, Amita Kasar, MD4, Yussif Issaka, MBChB5, Yazan Al Ajlouni, MD, Mphil6, Basile Njei, MD, PhD, MPH7. P4301 - Outcomes of Acute Pancreatitis in Lean vs Non-Lean MASLD Patients: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
