Tuesday Poster Session
Category: Biliary/Pancreas
P4299 - Stapled Versus Hand-Sewn Anastomosis in Pancreaticoduodenectomy: A Systematic Review and Meta-Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Fariha Hasan, MD
Cooper University Hospital
Camden, NJ
Presenting Author(s)
Fariha Hasan, MD1, Zain Ul Abideen, MBBS2, Muhammad Hassan Waseem, MBBS3, Sania Aimen, MBBS4, Noor Ul Huda Ramzan, MD5, Hareesha Rishab Bharadwaj, 6, Dushyant S. Dahiya, MD7, Hassan Aziz, MD8
1Cooper University Hospital, Camden, NJ; 2King Edward Medical University, Lahore, Punjab, Pakistan; 3Allama Iqbal Medical College, Lahore, Punjab, Pakistan; 4Quetta Institute of Medical Sciences, Quetta, Balochistan, Pakistan; 5University of Texas Southwestern Medical Center, Dallas, TX; 6The University of Manchester, Manchester, England, United Kingdom; 7University of Kansas School of Medicine, Kansas City, KS; 8University of Iowa, Iowa City, IA
Introduction: The optimal anastomotic method for pancreaticoduodenectomy (PD) remains a subject of debate. This meta-analysis aimed to assess the postoperative outcomes of Stapled anastomosis (SA) versus Hand-sewn anastomosis (HA) of gastro/duodenojejunostomy in pancreaticoduodenectomy.
Methods: Electronic databases including PubMed, Cochrane Library and ScienceDirect were searched from inception till January 2025. This review adhered closely to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. The Risk Ratios (RR) along with the 95% Confidence Intervals (CI) were pooled under the random effects model using the Review Manager version 5.4.1 for the dichotomous outcomes. The primary and secondary endpoints of interest were clinically relevant delayed gastric emptying (CR-DGE), anastomotic bleeding, anastomotic leakage, intra-abdominal abscess, mortality, and postoperative pancreatic fistula (POPF). The quality assessment was done through the Cochrane Risk of Bias (RoB) 2.0 tool and the Newcastle Ottawa Scale. Publication bias was assessed visually through the funnel plots and statistically through Egger’s regression test. A leave-one-out sensitivity analysis was conducted to explore the source of heterogeneity.
Results: Nine studies encompassing a total of 1,738 patients were included in this meta-analysis. SA group showed a significant increase in the risk of anastomotic bleeding (RR=7.39, 95%CI:[2.20,24.81]; p=0.001; I2=0%). SA was assoicated with a low risk of clinically relevant delayed gastric emptying but the results were statisticallly non-significant (RR= 0.64; 95%CI:[0.38,1.07]; p=0.09; I2=75%). Similarly, other outcomes including the anastomotic leak (RR= 0.74; 95%CI:[0.27,2.03]; p=0.56; I2=0%), intra-abdominal abscess (RR= 1.36; 95%CI:[0.83,2.24]; p=0.22; I2=33%), postoperative pancreatic fistula (RR= 1.02; 95%CI:[0.84,1.25]; p=0.82; I2=0%) and mortality (RR= 2.45; 95%CI:[0.36,16.83]; p=0.36; I2=12%) were comparable between the two anastomotic techniques.
Discussion: SA significantly increases the risk of anastomotic bleeding compared to HA in pancreaticoduodenectomy, while other postoperative outcomes, including DGE, anastomotic leakage, and mortality, remain comparable. These results highlight the need for cautious patient selection and careful surgical planning when opting for SA methods. Further studies are warranted to optimize stapling techniques and better define their role in clinical practice.
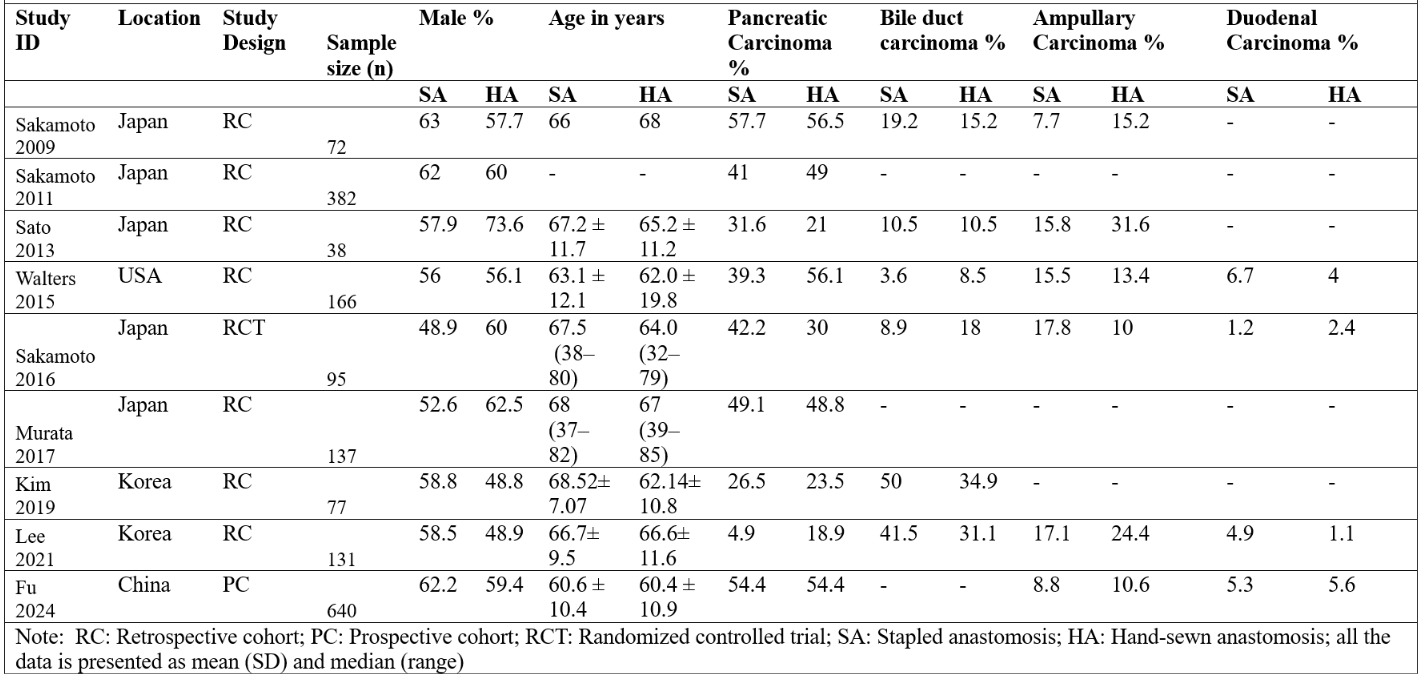
Figure: Figure 1: Forest Plots for (A)Anastomotic Bleeding (B)Clinically Relevant Delayed Gastric Emptying (C)Anastomotic Leak (D)Mortality
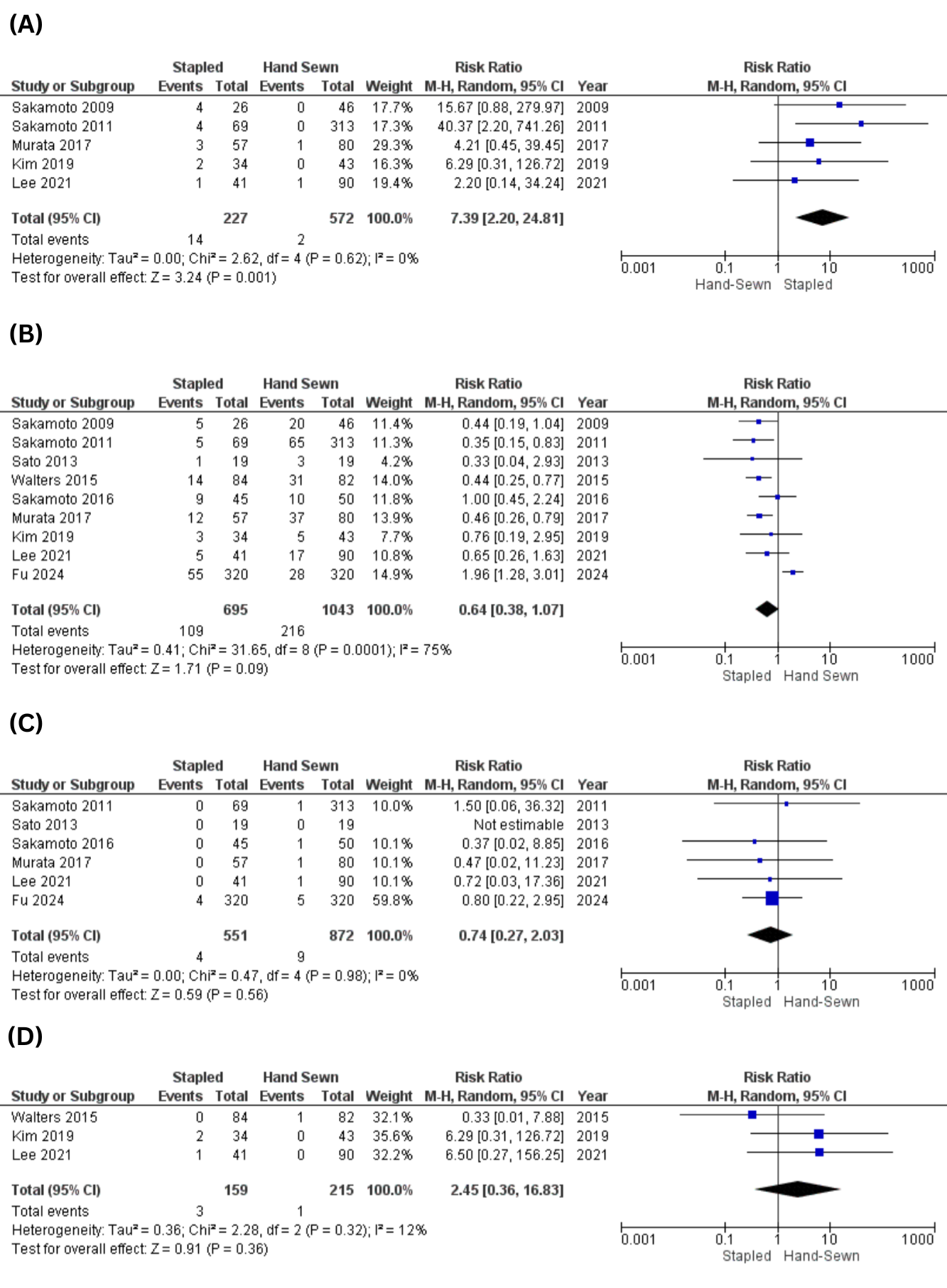
Figure: Figure 2: Baseline Characteristics of the Included Studies
Disclosures:
Fariha Hasan indicated no relevant financial relationships.
Zain Ul Abideen indicated no relevant financial relationships.
Muhammad Hassan Waseem indicated no relevant financial relationships.
Sania Aimen indicated no relevant financial relationships.
Noor Ul Huda Ramzan indicated no relevant financial relationships.
Hareesha Rishab Bharadwaj indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Hassan Aziz indicated no relevant financial relationships.
Fariha Hasan, MD1, Zain Ul Abideen, MBBS2, Muhammad Hassan Waseem, MBBS3, Sania Aimen, MBBS4, Noor Ul Huda Ramzan, MD5, Hareesha Rishab Bharadwaj, 6, Dushyant S. Dahiya, MD7, Hassan Aziz, MD8. P4299 - Stapled Versus Hand-Sewn Anastomosis in Pancreaticoduodenectomy: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cooper University Hospital, Camden, NJ; 2King Edward Medical University, Lahore, Punjab, Pakistan; 3Allama Iqbal Medical College, Lahore, Punjab, Pakistan; 4Quetta Institute of Medical Sciences, Quetta, Balochistan, Pakistan; 5University of Texas Southwestern Medical Center, Dallas, TX; 6The University of Manchester, Manchester, England, United Kingdom; 7University of Kansas School of Medicine, Kansas City, KS; 8University of Iowa, Iowa City, IA
Introduction: The optimal anastomotic method for pancreaticoduodenectomy (PD) remains a subject of debate. This meta-analysis aimed to assess the postoperative outcomes of Stapled anastomosis (SA) versus Hand-sewn anastomosis (HA) of gastro/duodenojejunostomy in pancreaticoduodenectomy.
Methods: Electronic databases including PubMed, Cochrane Library and ScienceDirect were searched from inception till January 2025. This review adhered closely to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. The Risk Ratios (RR) along with the 95% Confidence Intervals (CI) were pooled under the random effects model using the Review Manager version 5.4.1 for the dichotomous outcomes. The primary and secondary endpoints of interest were clinically relevant delayed gastric emptying (CR-DGE), anastomotic bleeding, anastomotic leakage, intra-abdominal abscess, mortality, and postoperative pancreatic fistula (POPF). The quality assessment was done through the Cochrane Risk of Bias (RoB) 2.0 tool and the Newcastle Ottawa Scale. Publication bias was assessed visually through the funnel plots and statistically through Egger’s regression test. A leave-one-out sensitivity analysis was conducted to explore the source of heterogeneity.
Results: Nine studies encompassing a total of 1,738 patients were included in this meta-analysis. SA group showed a significant increase in the risk of anastomotic bleeding (RR=7.39, 95%CI:[2.20,24.81]; p=0.001; I2=0%). SA was assoicated with a low risk of clinically relevant delayed gastric emptying but the results were statisticallly non-significant (RR= 0.64; 95%CI:[0.38,1.07]; p=0.09; I2=75%). Similarly, other outcomes including the anastomotic leak (RR= 0.74; 95%CI:[0.27,2.03]; p=0.56; I2=0%), intra-abdominal abscess (RR= 1.36; 95%CI:[0.83,2.24]; p=0.22; I2=33%), postoperative pancreatic fistula (RR= 1.02; 95%CI:[0.84,1.25]; p=0.82; I2=0%) and mortality (RR= 2.45; 95%CI:[0.36,16.83]; p=0.36; I2=12%) were comparable between the two anastomotic techniques.
Discussion: SA significantly increases the risk of anastomotic bleeding compared to HA in pancreaticoduodenectomy, while other postoperative outcomes, including DGE, anastomotic leakage, and mortality, remain comparable. These results highlight the need for cautious patient selection and careful surgical planning when opting for SA methods. Further studies are warranted to optimize stapling techniques and better define their role in clinical practice.
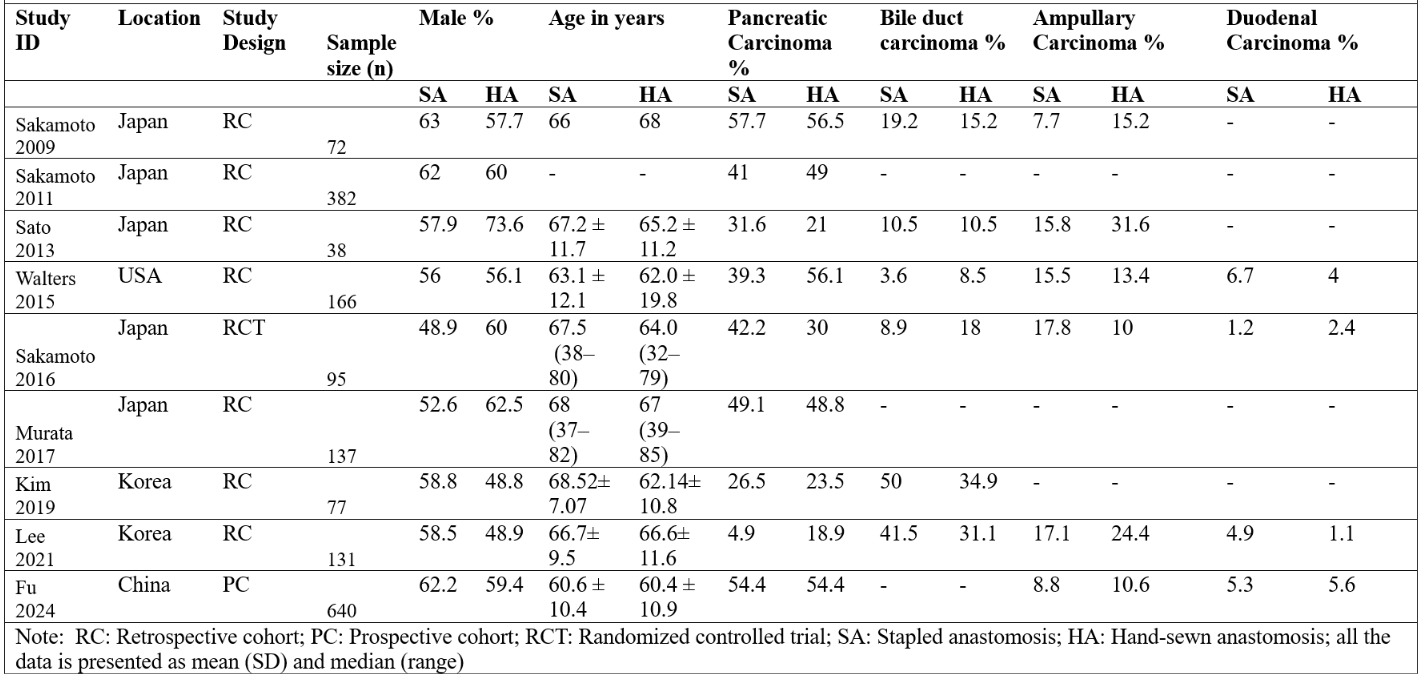
Figure: Figure 1: Forest Plots for (A)Anastomotic Bleeding (B)Clinically Relevant Delayed Gastric Emptying (C)Anastomotic Leak (D)Mortality
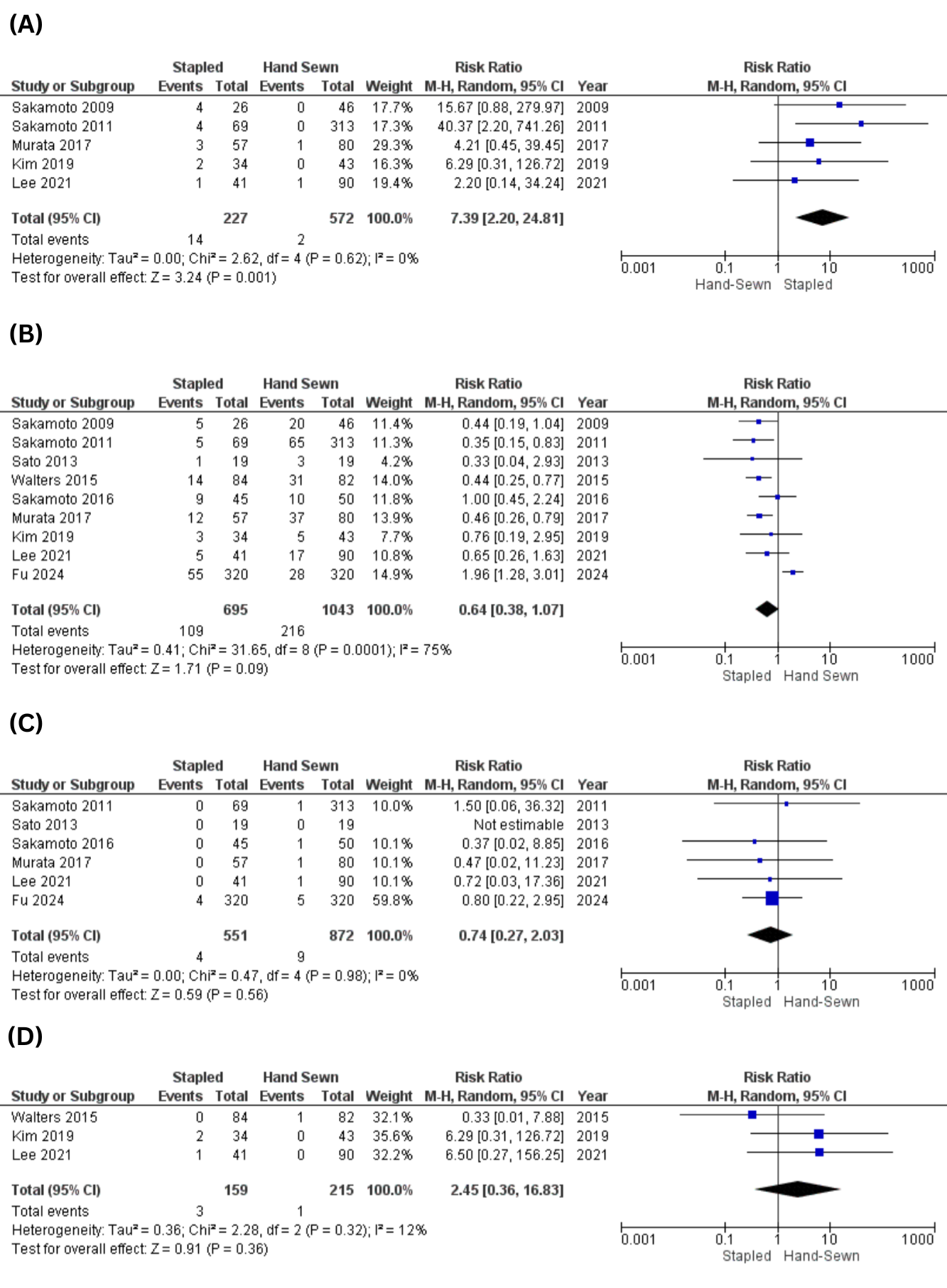
Figure: Figure 2: Baseline Characteristics of the Included Studies
Disclosures:
Fariha Hasan indicated no relevant financial relationships.
Zain Ul Abideen indicated no relevant financial relationships.
Muhammad Hassan Waseem indicated no relevant financial relationships.
Sania Aimen indicated no relevant financial relationships.
Noor Ul Huda Ramzan indicated no relevant financial relationships.
Hareesha Rishab Bharadwaj indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Hassan Aziz indicated no relevant financial relationships.
Fariha Hasan, MD1, Zain Ul Abideen, MBBS2, Muhammad Hassan Waseem, MBBS3, Sania Aimen, MBBS4, Noor Ul Huda Ramzan, MD5, Hareesha Rishab Bharadwaj, 6, Dushyant S. Dahiya, MD7, Hassan Aziz, MD8. P4299 - Stapled Versus Hand-Sewn Anastomosis in Pancreaticoduodenectomy: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
