Sunday Poster Session
Category: Small Intestine
P1997 - Mesenteric Ischemia as an Atypical Presentation of Antiphospholipid Syndrome
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Reinaldo Hernandez, MD
University District Hospital
San Juan, PR
Presenting Author(s)
Reinaldo Hernandez, MD1, Gretchen Rios Grant, MD1, Steven Velez, MD1, Paloma Velasco, MD1, José Bretón-Arias, MD2, Valeria Rodríguez González, MD3, Mark Vergara-Gómez, MD2
1University District Hospital, San Juan, Puerto Rico; 2University of Puerto Rico School of Medicine, San Juan, Puerto Rico; 3University of Puerto Rico, Medical Sciences Campus, San Juan, Puerto Rico
Introduction: Antiphospholipid syndrome (APS) is an autoimmune condition marked by the ongoing presence of antiphospholipid antibodies. Common presentations may include deep vein thrombosis, pulmonary embolism, stroke, transient ischemic attacks, and pregnancy-related issues such as fetal loss after 10 weeks, repeated miscarriages, or severe preeclampsia. In this report, we present the case of a young male who presented with portal vein, superior mesenteric vein (SMV), and splenic vein thrombosis with associated splenic infarction as initial presentation of APS.
Case Description/
Methods: A 25-year-old male with no past medical history who presented with abdominal pain and distention, rash, early satiety and weight loss. Physical examination revealed an acute abdomen. Abdominopelvic (A/P) CT with IV contrast uncovered a poorly organized inflammatory process within the mesentery of the right lower quadrant medial to the proximal ascending colon; small bowel inflammation, dilation, and a small amount of free fluid in the right pericolic gutter and around the tip of the liver and lower pelvis. Patient underwent exploratory laparotomy with appendectomy, small bowel resection, and primary anastomosis. Biopsies were remarkable for focal acute perforation with fibrous adhesions, serositis, and peri appendicitis. After poor post-operative symptomatic control, patient underwent subsequent A/P CT Angiogram which revealed diffuse small bowel inflammation with free fluid in the lower abdomen/pelvis and portal, SMV, and splenic vein thrombosis with associated splenic infarction. Hypercoagulable workup was remarkable for two positive Lupus Anticoagulant test which were more than 12 weeks apart, confirming APS. Upon discharge, the patient was started on warfarin as an anticoagulation strategy. He has continued to follow up with his primary care physician, hematologist and gastroenterologist with no further venous thromboembolic events (VTE).
Discussion: Colonic or mesenteric ischemia is a rare manifestation of APS, with fewer than 100 reported cases over two decades. This case illustrates an unusual catastrophic onset in a young patient without prior thrombotic events and the importance of early suspicion based on clinical history and physical exam. The American College of Gastroenterology states that while thrombophilia, including APS, may contribute to colonic ischemia, it is not a major cause, and routine testing is only advised in young or recurrent cases.
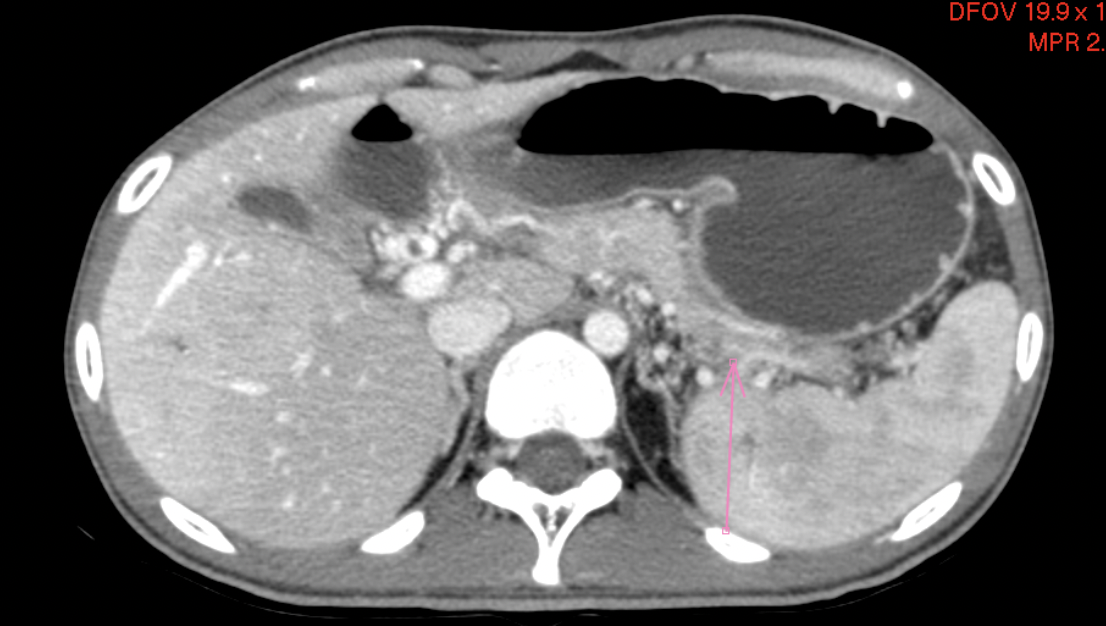
Figure: CT Abdomen/Pelvis with IV Contrast: Complete obliteration of splenic vein (Axial View)
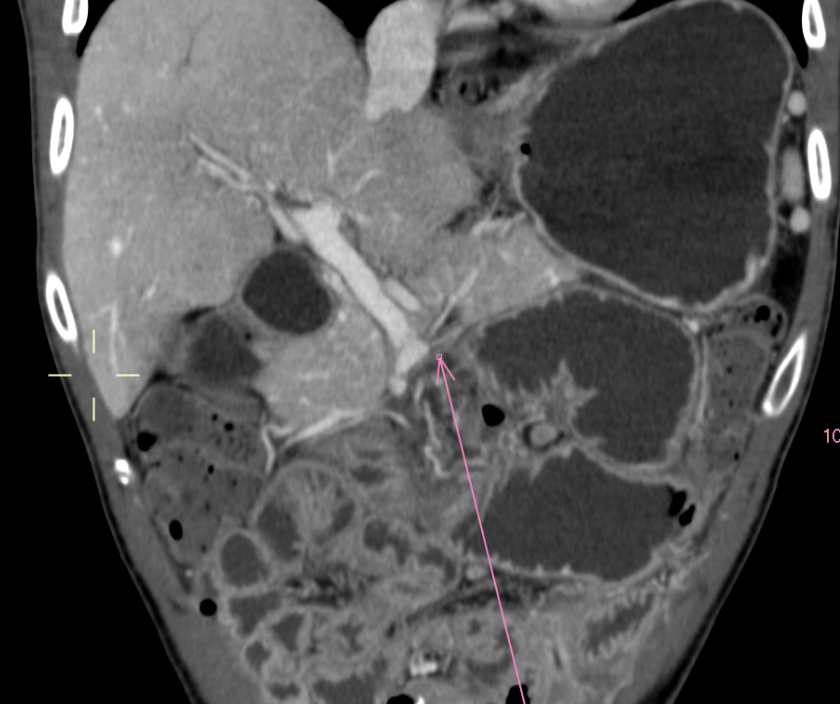
Figure: CT Abdomen/Pelvis with IV Contrast: Complete obliteration of splenic vein (Coronal View)
Disclosures:
Reinaldo Hernandez indicated no relevant financial relationships.
Gretchen Rios Grant indicated no relevant financial relationships.
Steven Velez indicated no relevant financial relationships.
Paloma Velasco indicated no relevant financial relationships.
José Bretón-Arias indicated no relevant financial relationships.
Valeria Rodríguez González indicated no relevant financial relationships.
Mark Vergara-Gómez indicated no relevant financial relationships.
Reinaldo Hernandez, MD1, Gretchen Rios Grant, MD1, Steven Velez, MD1, Paloma Velasco, MD1, José Bretón-Arias, MD2, Valeria Rodríguez González, MD3, Mark Vergara-Gómez, MD2. P1997 - Mesenteric Ischemia as an Atypical Presentation of Antiphospholipid Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University District Hospital, San Juan, Puerto Rico; 2University of Puerto Rico School of Medicine, San Juan, Puerto Rico; 3University of Puerto Rico, Medical Sciences Campus, San Juan, Puerto Rico
Introduction: Antiphospholipid syndrome (APS) is an autoimmune condition marked by the ongoing presence of antiphospholipid antibodies. Common presentations may include deep vein thrombosis, pulmonary embolism, stroke, transient ischemic attacks, and pregnancy-related issues such as fetal loss after 10 weeks, repeated miscarriages, or severe preeclampsia. In this report, we present the case of a young male who presented with portal vein, superior mesenteric vein (SMV), and splenic vein thrombosis with associated splenic infarction as initial presentation of APS.
Case Description/
Methods: A 25-year-old male with no past medical history who presented with abdominal pain and distention, rash, early satiety and weight loss. Physical examination revealed an acute abdomen. Abdominopelvic (A/P) CT with IV contrast uncovered a poorly organized inflammatory process within the mesentery of the right lower quadrant medial to the proximal ascending colon; small bowel inflammation, dilation, and a small amount of free fluid in the right pericolic gutter and around the tip of the liver and lower pelvis. Patient underwent exploratory laparotomy with appendectomy, small bowel resection, and primary anastomosis. Biopsies were remarkable for focal acute perforation with fibrous adhesions, serositis, and peri appendicitis. After poor post-operative symptomatic control, patient underwent subsequent A/P CT Angiogram which revealed diffuse small bowel inflammation with free fluid in the lower abdomen/pelvis and portal, SMV, and splenic vein thrombosis with associated splenic infarction. Hypercoagulable workup was remarkable for two positive Lupus Anticoagulant test which were more than 12 weeks apart, confirming APS. Upon discharge, the patient was started on warfarin as an anticoagulation strategy. He has continued to follow up with his primary care physician, hematologist and gastroenterologist with no further venous thromboembolic events (VTE).
Discussion: Colonic or mesenteric ischemia is a rare manifestation of APS, with fewer than 100 reported cases over two decades. This case illustrates an unusual catastrophic onset in a young patient without prior thrombotic events and the importance of early suspicion based on clinical history and physical exam. The American College of Gastroenterology states that while thrombophilia, including APS, may contribute to colonic ischemia, it is not a major cause, and routine testing is only advised in young or recurrent cases.
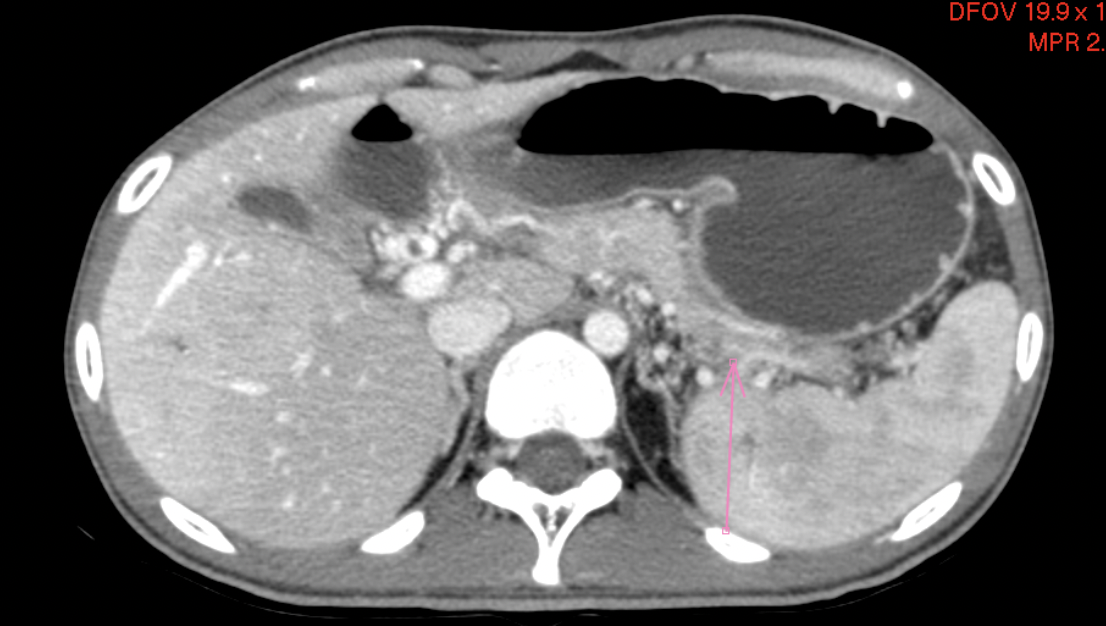
Figure: CT Abdomen/Pelvis with IV Contrast: Complete obliteration of splenic vein (Axial View)
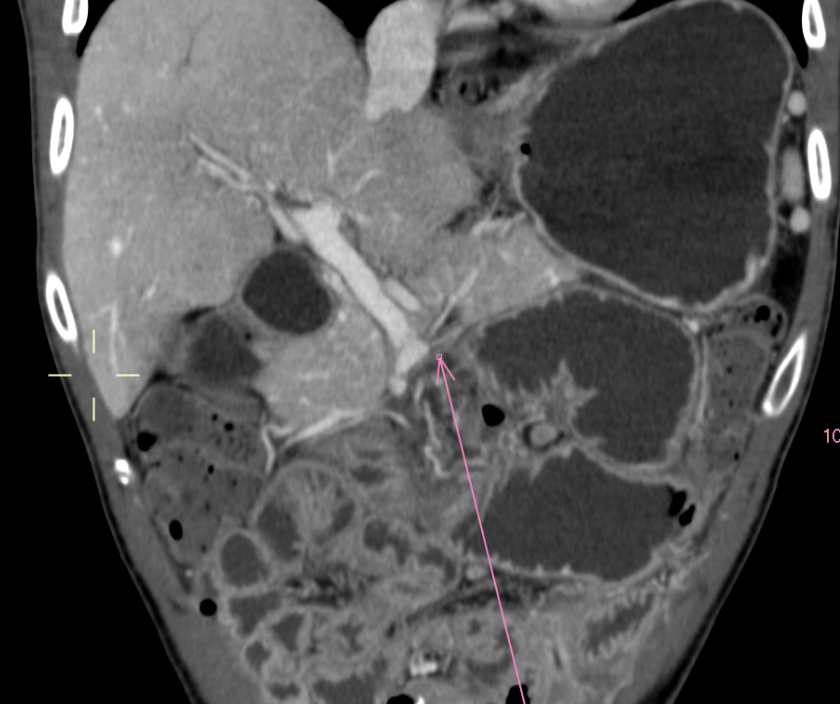
Figure: CT Abdomen/Pelvis with IV Contrast: Complete obliteration of splenic vein (Coronal View)
Disclosures:
Reinaldo Hernandez indicated no relevant financial relationships.
Gretchen Rios Grant indicated no relevant financial relationships.
Steven Velez indicated no relevant financial relationships.
Paloma Velasco indicated no relevant financial relationships.
José Bretón-Arias indicated no relevant financial relationships.
Valeria Rodríguez González indicated no relevant financial relationships.
Mark Vergara-Gómez indicated no relevant financial relationships.
Reinaldo Hernandez, MD1, Gretchen Rios Grant, MD1, Steven Velez, MD1, Paloma Velasco, MD1, José Bretón-Arias, MD2, Valeria Rodríguez González, MD3, Mark Vergara-Gómez, MD2. P1997 - Mesenteric Ischemia as an Atypical Presentation of Antiphospholipid Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
