Sunday Poster Session
Category: Small Intestine
P1988 - Well-Differentiated Ileal Neuroendocrine Tumor Presenting With Nonspecific GI Symptoms and Iron Deficiency Anemia
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- BM
Benjamin Mauri, MD
Temple University
Philadelphia, PA
Presenting Author(s)
Benjamin Mauri, MD, Sherifatu Abu, MD, MPH, Neena Mohan, MD
Temple University, Philadelphia, PA
Introduction: Neuroendocrine tumors (NETs) are rare malignancies arising from neuroendocrine cells with an annual incidence of 6.98 per 100,000 persons, a steadily increasing. NETs most commonly occur in the small intestine (44.7%), rectum (19.6%), appendix (16.7%), and colon (10.6%). Clinical presentation is variable and nonspecific with many patients being asymptomatic or with vague symptoms, such as fatigue or abdominal pain. NETs can be indolent with metastatic disease found at time of diagnosis.
Case Description/
Methods: A 44-year-old female with asthma, hypertension, and chronic heavy alcohol use presented to an outpatient GI clinic with several months of intermittent, non-radiating epigastric pain, new onset constipation, and intermittent nausea and vomiting. Lab work showed severe iron deficiency anemia. She underwent EGD and colonoscopy, which showed a solitary nonbleeding ulcer in the terminal ileum (TI) that was unable to be biopsied, an 11 mm polypoid lesion with congestion at the ileocecal valve, and a 6 mm cecal polyp. Immunohistochemical stain of the cecal polyp and abnormal TI mucosa revealed a well-differentiated NET G2 positive for synaptophysin, chromogranin, CD56, AE1/AE3, and Ki-67 = ~10% nuclear positivity. CT enterogram showed mural thickening of the TI, cecum, and ascending colon consistent with enterocolitis, along with segmental bowel wall thickening concerning for inflammation. Ga-68 DOTATATE scan showed hypermetabolic uptake in the ileocecal region at the known NET site and metastasis to a right ileal mesenteric node, central liver, and duodenum/periduodenal node: with overall grade 4 uptake by Krening score. The ileocecal tumor was resected with a right hemicolectomy. Intraoperatively, all 5 lesions were localized to segment 4B and removed via hepatic segment 4B wedge resection. Surgical pathology confirmed well differentiated NET G2 at the ileocecal valve, in one liver fragment, and in local lymph nodes with extranodal extension. After discharge, she recovered well and will continue with surveillance CT imaging to determine future need for systemic therapies.
Discussion: This case illustrates the indolent nature of NETs and the critical importance of a careful endoscopic examination. Approximately 30% of patients with small bowel NETs have metastatic disease at the time of diagnosis. Timely workup and treatment are key as small intestine NETs with distant metastasis have a median overall survival of about 6 years, and incomplete tumor resection is associated with worse survival.
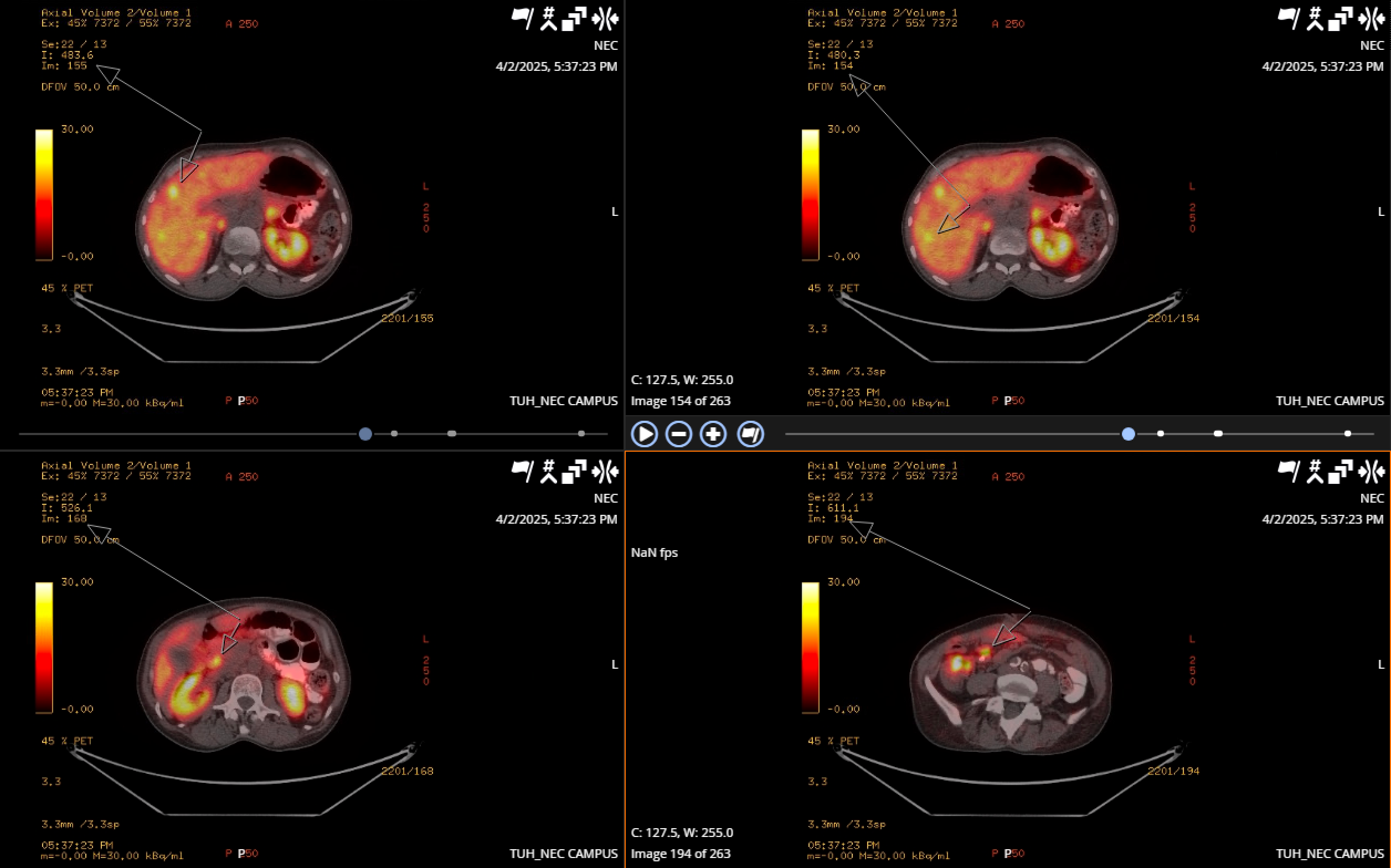
Figure: Image 1a: Polypoid lesion at the ileocecal valve (circle) with congested and abnormal mucosa (arrows). 1b: Solitary ulcer in terminal ileum.
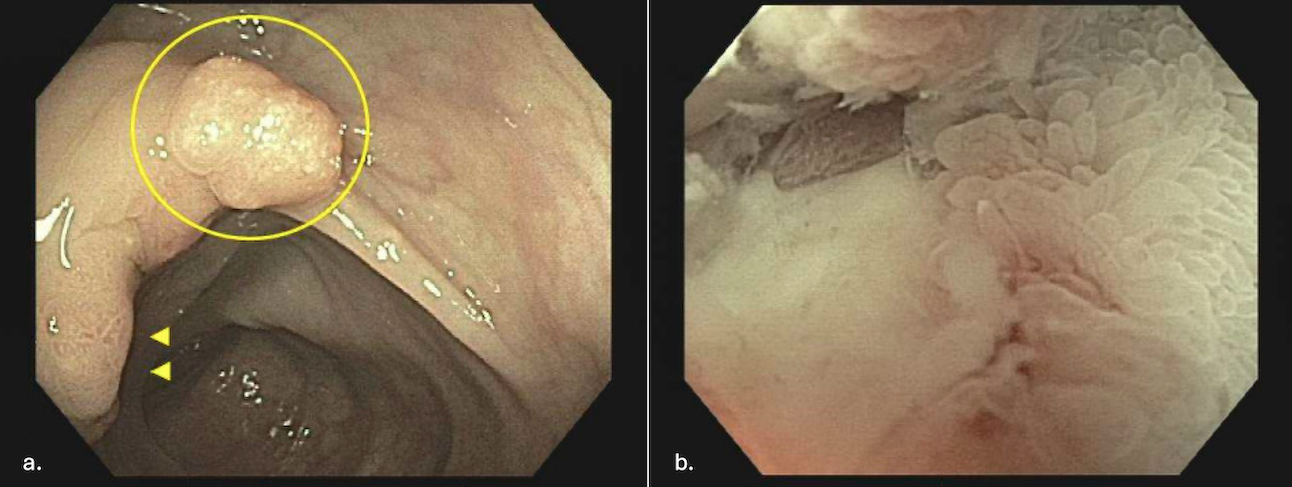
Figure: Image 2: Ga-68 DOTATATE PET scan showing hypermetabolic central liver lesions compatible with metastatic disease, hypermetabolic uptake in the ileocecal region at site of known neuroendocrine malignancy, right ileal mesenteric part calcified node compatible with metastatic disease, and uptake in duodenum versus periduodenal node.
Disclosures:
Benjamin Mauri indicated no relevant financial relationships.
Sherifatu Abu indicated no relevant financial relationships.
Neena Mohan: Cyted – Advisory Committee/Board Member.
Benjamin Mauri, MD, Sherifatu Abu, MD, MPH, Neena Mohan, MD. P1988 - Well-Differentiated Ileal Neuroendocrine Tumor Presenting With Nonspecific GI Symptoms and Iron Deficiency Anemia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Temple University, Philadelphia, PA
Introduction: Neuroendocrine tumors (NETs) are rare malignancies arising from neuroendocrine cells with an annual incidence of 6.98 per 100,000 persons, a steadily increasing. NETs most commonly occur in the small intestine (44.7%), rectum (19.6%), appendix (16.7%), and colon (10.6%). Clinical presentation is variable and nonspecific with many patients being asymptomatic or with vague symptoms, such as fatigue or abdominal pain. NETs can be indolent with metastatic disease found at time of diagnosis.
Case Description/
Methods: A 44-year-old female with asthma, hypertension, and chronic heavy alcohol use presented to an outpatient GI clinic with several months of intermittent, non-radiating epigastric pain, new onset constipation, and intermittent nausea and vomiting. Lab work showed severe iron deficiency anemia. She underwent EGD and colonoscopy, which showed a solitary nonbleeding ulcer in the terminal ileum (TI) that was unable to be biopsied, an 11 mm polypoid lesion with congestion at the ileocecal valve, and a 6 mm cecal polyp. Immunohistochemical stain of the cecal polyp and abnormal TI mucosa revealed a well-differentiated NET G2 positive for synaptophysin, chromogranin, CD56, AE1/AE3, and Ki-67 = ~10% nuclear positivity. CT enterogram showed mural thickening of the TI, cecum, and ascending colon consistent with enterocolitis, along with segmental bowel wall thickening concerning for inflammation. Ga-68 DOTATATE scan showed hypermetabolic uptake in the ileocecal region at the known NET site and metastasis to a right ileal mesenteric node, central liver, and duodenum/periduodenal node: with overall grade 4 uptake by Krening score. The ileocecal tumor was resected with a right hemicolectomy. Intraoperatively, all 5 lesions were localized to segment 4B and removed via hepatic segment 4B wedge resection. Surgical pathology confirmed well differentiated NET G2 at the ileocecal valve, in one liver fragment, and in local lymph nodes with extranodal extension. After discharge, she recovered well and will continue with surveillance CT imaging to determine future need for systemic therapies.
Discussion: This case illustrates the indolent nature of NETs and the critical importance of a careful endoscopic examination. Approximately 30% of patients with small bowel NETs have metastatic disease at the time of diagnosis. Timely workup and treatment are key as small intestine NETs with distant metastasis have a median overall survival of about 6 years, and incomplete tumor resection is associated with worse survival.
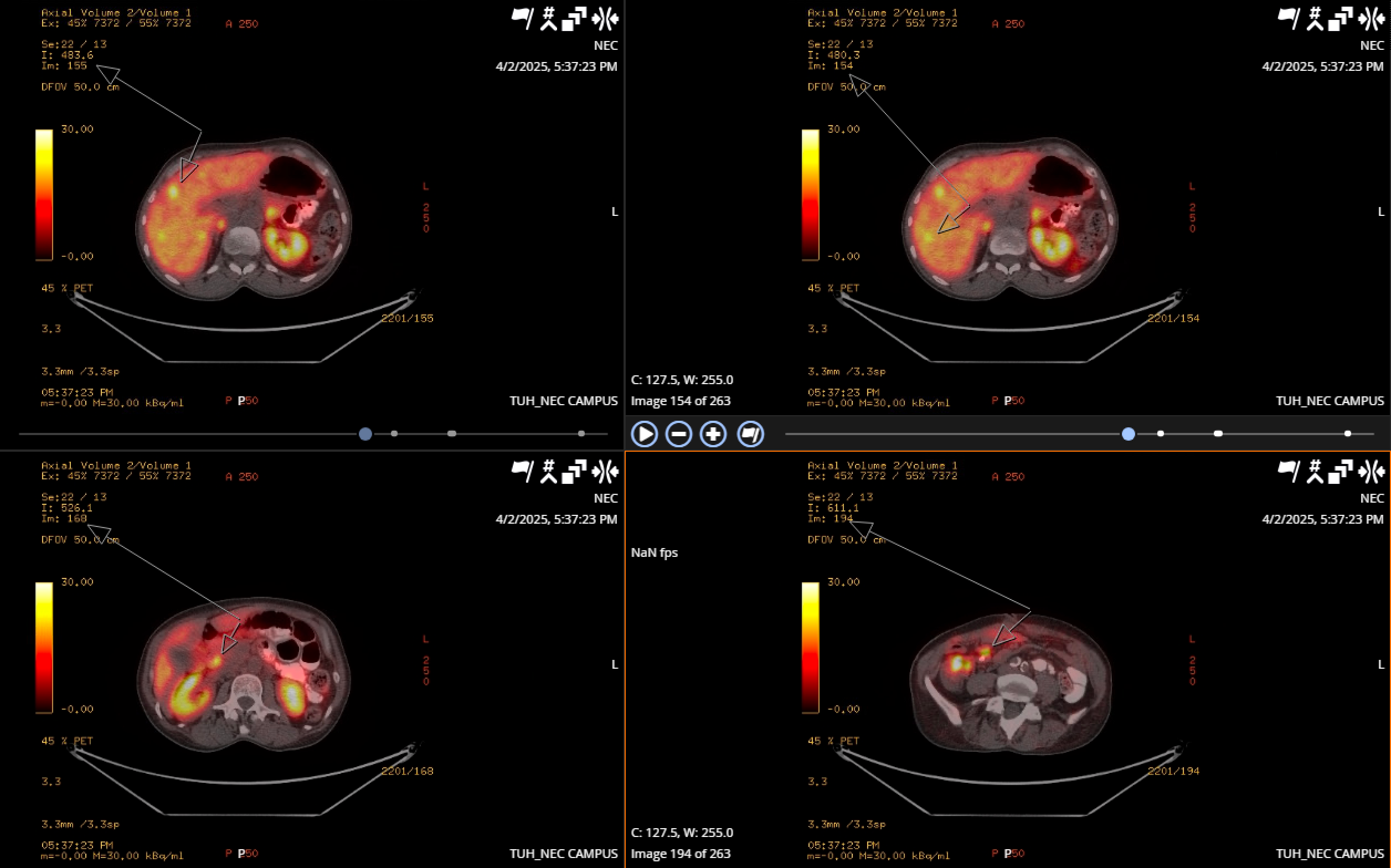
Figure: Image 1a: Polypoid lesion at the ileocecal valve (circle) with congested and abnormal mucosa (arrows). 1b: Solitary ulcer in terminal ileum.
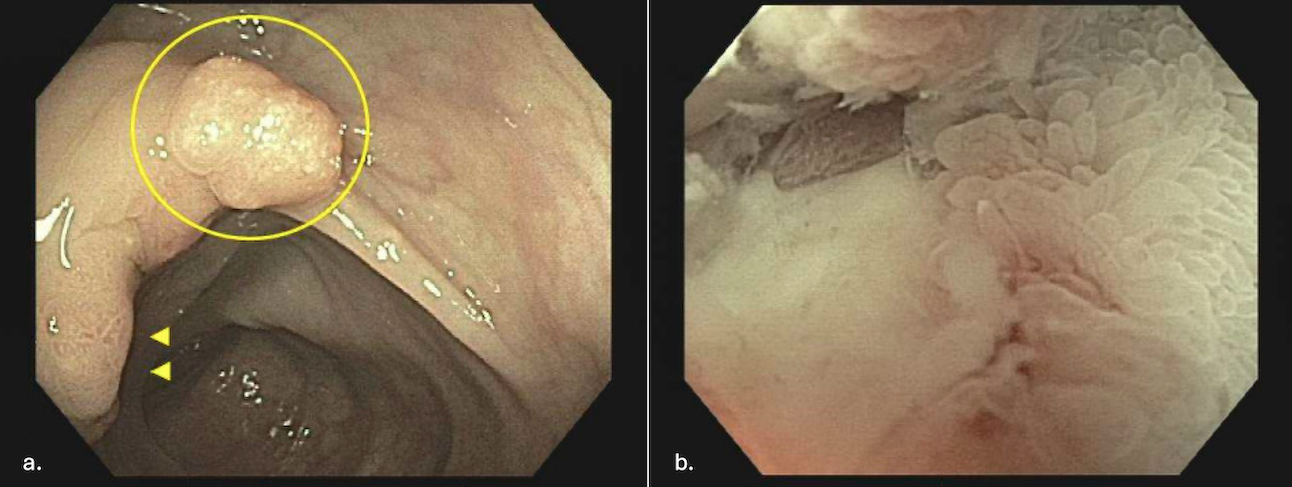
Figure: Image 2: Ga-68 DOTATATE PET scan showing hypermetabolic central liver lesions compatible with metastatic disease, hypermetabolic uptake in the ileocecal region at site of known neuroendocrine malignancy, right ileal mesenteric part calcified node compatible with metastatic disease, and uptake in duodenum versus periduodenal node.
Disclosures:
Benjamin Mauri indicated no relevant financial relationships.
Sherifatu Abu indicated no relevant financial relationships.
Neena Mohan: Cyted – Advisory Committee/Board Member.
Benjamin Mauri, MD, Sherifatu Abu, MD, MPH, Neena Mohan, MD. P1988 - Well-Differentiated Ileal Neuroendocrine Tumor Presenting With Nonspecific GI Symptoms and Iron Deficiency Anemia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
