Sunday Poster Session
Category: Small Intestine
P1985 - A Case of COVID-19 Enteritis Mimicking Crohn’s Disease
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Mohamed K. Osman, MD, MPH
NYC Health + Hospitals/Harlem
New York, NY
Presenting Author(s)
Mohamed K.. Osman, MD, MPH1, Thin Phyu Phyu. Aung, MD2, Joan A.. Culpepper-Morgan, MD, FACG2
1NYC Health + Hospitals/Harlem, New York, NY; 2NYC Health + Hospitals, New York, NY
Introduction: COVID enteritis is intestinal inflammation caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus responsible for COVID-19 infection. We present a patient whose illness suggested inflammatory bowel disease (IBD).
Case Description/
Methods: A 63-year-old female 19 years post Roux-en-Y gastric bypass (RYGB) presented with epigastric pain and watery diarrhea for 5 days. Two weeks prior, she started levofloxacin for cough, then changed to amoxicillin after one week. Pain was constant and 5-9 in severity. Diarrhea was watery, non-bloody, frequent, and associated with anorexia. She denied nausea, vomiting, or heme per os or per rectum. She had mild epigastric tenderness. COVID test was positive. Lactate was 1.6 mmol/l. CT showed a thickened, edematous 10-cm segment of the proximal Roux limb with mesenteric stranding (Figure 1). She received IV fluids, pantoprazole, and sucralfate. Esophagogastroduodenoscopy (EGD) showed a healthy gastrojejunal anastomosis and a 5 cm efferent limb segment with erythema, edema, and exudates (Figure 2). Biopsy revealed benign small bowel mucosa with mild, nonspecific chronic active inflammation, while the anastomotic biopsy showed normal mucosa with preserved architecture. GI PCR, ova and parasite, and C. difficile PCR were negative. She completed 5 days of remdesivir and was discharged. In 2 weeks, pain resolved. She had H. pylori on stool test, and received triple therapy for 2 weeks. ASCA IgA was positive (26 units), ASCA IgG positive (38.8 units), P-ANCA negative, ESR 44 mm/hr, and CRP 67.2 mg/l. At 4 months, fecal calprotectin was still 135 ug/g, and she had +ve IBD panel, consistent with Crohn’s. CRP fell to 9 and ESR to 35. EGD showed normal anastomosis with resolution of efferent jejunal limb erythema. Biopsies showed chronic inactive gastritis and no H. pylori. Colonoscopy was unremarkable including biopsies.
Discussion: Our patient’s symptoms and intestinal ulceration resolved with COVID-19 recovery. The virus binds to ACE2 receptors on enterocytes, causing epithelial damage, cytokine release, increased gut permeability, inflammation, and dysbiosis. RYGB patients may have higher complication risks from altered anatomy and nutrient malabsorption. They are also at increased risk of IBD due to dysbiosis. Our patient had a serology panel suggestive of Crohn’s, despite symptom and endoscopic resolution. H. pylori may have worsened dysbiosis by lowering pouch parietal cells’ acid output, predisposing her to COVID enteritis.
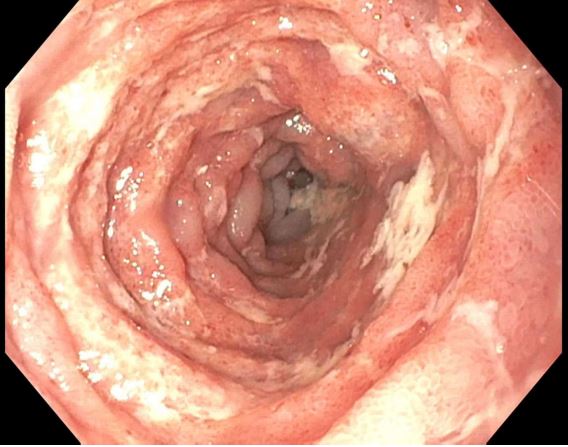
Figure: Figure 1. Long thickened segment of proximal Roux limb (arrow)

Figure: Figure 2. Efferent limb segment with erythema, edema and exudates
Disclosures:
Mohamed Osman indicated no relevant financial relationships.
Thin Aung indicated no relevant financial relationships.
Joan Culpepper-Morgan indicated no relevant financial relationships.
Mohamed K.. Osman, MD, MPH1, Thin Phyu Phyu. Aung, MD2, Joan A.. Culpepper-Morgan, MD, FACG2. P1985 - A Case of COVID-19 Enteritis Mimicking Crohn’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NYC Health + Hospitals/Harlem, New York, NY; 2NYC Health + Hospitals, New York, NY
Introduction: COVID enteritis is intestinal inflammation caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus responsible for COVID-19 infection. We present a patient whose illness suggested inflammatory bowel disease (IBD).
Case Description/
Methods: A 63-year-old female 19 years post Roux-en-Y gastric bypass (RYGB) presented with epigastric pain and watery diarrhea for 5 days. Two weeks prior, she started levofloxacin for cough, then changed to amoxicillin after one week. Pain was constant and 5-9 in severity. Diarrhea was watery, non-bloody, frequent, and associated with anorexia. She denied nausea, vomiting, or heme per os or per rectum. She had mild epigastric tenderness. COVID test was positive. Lactate was 1.6 mmol/l. CT showed a thickened, edematous 10-cm segment of the proximal Roux limb with mesenteric stranding (Figure 1). She received IV fluids, pantoprazole, and sucralfate. Esophagogastroduodenoscopy (EGD) showed a healthy gastrojejunal anastomosis and a 5 cm efferent limb segment with erythema, edema, and exudates (Figure 2). Biopsy revealed benign small bowel mucosa with mild, nonspecific chronic active inflammation, while the anastomotic biopsy showed normal mucosa with preserved architecture. GI PCR, ova and parasite, and C. difficile PCR were negative. She completed 5 days of remdesivir and was discharged. In 2 weeks, pain resolved. She had H. pylori on stool test, and received triple therapy for 2 weeks. ASCA IgA was positive (26 units), ASCA IgG positive (38.8 units), P-ANCA negative, ESR 44 mm/hr, and CRP 67.2 mg/l. At 4 months, fecal calprotectin was still 135 ug/g, and she had +ve IBD panel, consistent with Crohn’s. CRP fell to 9 and ESR to 35. EGD showed normal anastomosis with resolution of efferent jejunal limb erythema. Biopsies showed chronic inactive gastritis and no H. pylori. Colonoscopy was unremarkable including biopsies.
Discussion: Our patient’s symptoms and intestinal ulceration resolved with COVID-19 recovery. The virus binds to ACE2 receptors on enterocytes, causing epithelial damage, cytokine release, increased gut permeability, inflammation, and dysbiosis. RYGB patients may have higher complication risks from altered anatomy and nutrient malabsorption. They are also at increased risk of IBD due to dysbiosis. Our patient had a serology panel suggestive of Crohn’s, despite symptom and endoscopic resolution. H. pylori may have worsened dysbiosis by lowering pouch parietal cells’ acid output, predisposing her to COVID enteritis.
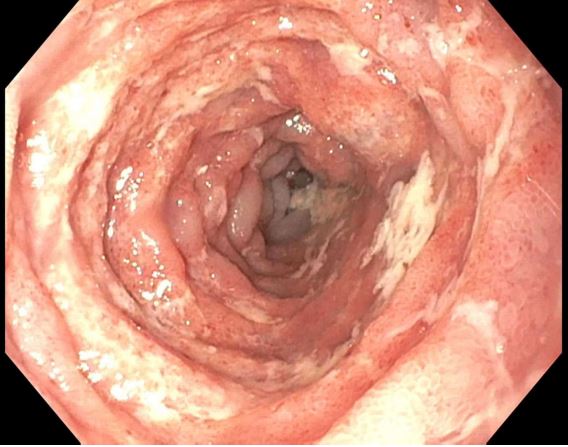
Figure: Figure 1. Long thickened segment of proximal Roux limb (arrow)

Figure: Figure 2. Efferent limb segment with erythema, edema and exudates
Disclosures:
Mohamed Osman indicated no relevant financial relationships.
Thin Aung indicated no relevant financial relationships.
Joan Culpepper-Morgan indicated no relevant financial relationships.
Mohamed K.. Osman, MD, MPH1, Thin Phyu Phyu. Aung, MD2, Joan A.. Culpepper-Morgan, MD, FACG2. P1985 - A Case of COVID-19 Enteritis Mimicking Crohn’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
