Sunday Poster Session
Category: Small Intestine
P1982 - A Case of Pyloroduodenal Intussusception Secondary to an Intraduodenal Lipoma
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Kenneth C. Barnett, MD
University of Oklahoma Health Sciences Center
Oklahoma City, OK
Presenting Author(s)
Kenneth C. Barnett, MD, Jiteshwar Pannu, MD, Apurva Shrigiriwar, MD, Donald Kastens, MD
University of Oklahoma Health Sciences Center, Oklahoma City, OK
Introduction: Gastrointestinal (GI) lipomas are benign submucosal tumors that are usually encountered as incidental findings in asymptomatic patients, but can rarely lead to complications such as small bowel obstruction (SBO), intussusception and bleeding from overlying ulceration. Herein, we present a case of an intraduodenal lipoma causing pyloroduodenal intussusception, highlighting the importance of timely diagnosis and intervention to prevent bowel obstruction.
Case Description/
Methods: An 82-year-old male, was admitted with intractable nausea and vomiting. Physical exam revealed a mildly distended abdomen and minimal epigastric tenderness without palpable mass. CT abdomen with contrast revealed non-obstructing pyloroduodenal intussusception with an intraduodenal lipoma (5.1x 4 x 3.7 cm) in D2 likely being a lead point for intussusception within the pyloric antrum and D1 telescoping into D2 (Figure A/B). Given the above findings, an urgent general surgery consult was sought. Patient was subsequently taken to the operating room for a robotic reduction, resection, and Heineke-Mikulicz pyloroplasty (Figure C/D). Intraoperative findings revealed a pedunculated duodenal bulb lipoma with a broad stalk. Pathology was consistent with 5.2 x 4.5 x 2.5 cm submucosal lipoma (Figure E). Patient did well post-operatively with gradual advancement of diet.
Discussion: Gastric and duodenal lipomas account for about 4% of all GI lipomas. While usually asymptomatic, larger lipomas (particularly those >2 cm) can cause complications like bleeding, SBO, or intussusception. Adult intussusception is rare and typically has a pathological lead point, unlike in children, and is commonly seen in the jejunum/ileum due to retroperitoneal adherence of the duodenum (except D1 segment). Lipomas (especially when submucosal and pedunculated), can act as such lead points, resulting in intermittent or acute symptoms similar to our case. CT is the imaging modality of choice, showing characteristic fat-density masses and sometimes the "target" sign of intussusception. Management depends on symptoms and suspicion of malignancy; endoscopic resection can be considered for smaller, low risk lesions whereas surgical approach is preferred for larger, symptomatic lesions causing complications. In this case, an intraduodenal lipoma served as the lead point for intussusception, an uncommon but important cause of adult SBO, necessitating prompt recognition and surgical management.
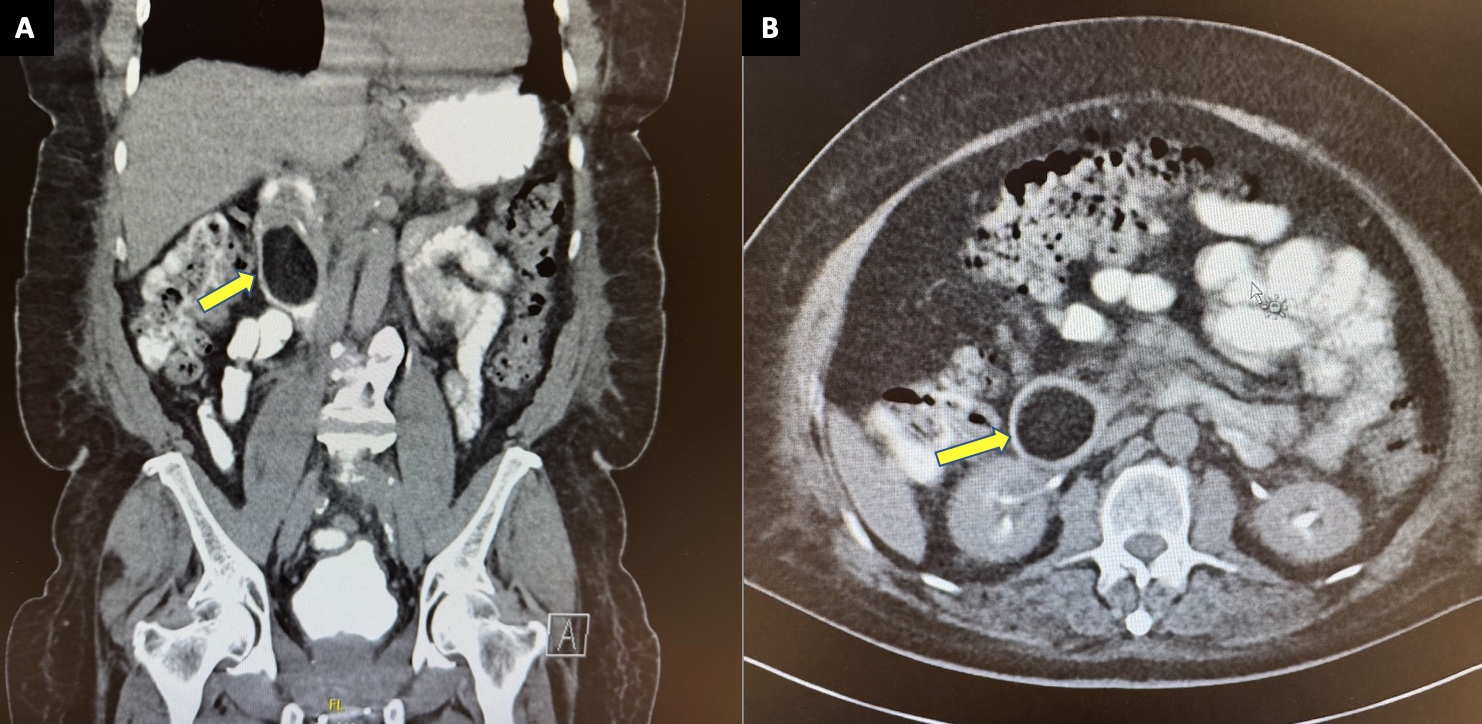
Figure: Figure A (Coronal) and B (Axial) showing large 5.1 x 4 x 3.7cm intraduodenal lipoma and pyloroduodenal intussusception (yellow arrow).
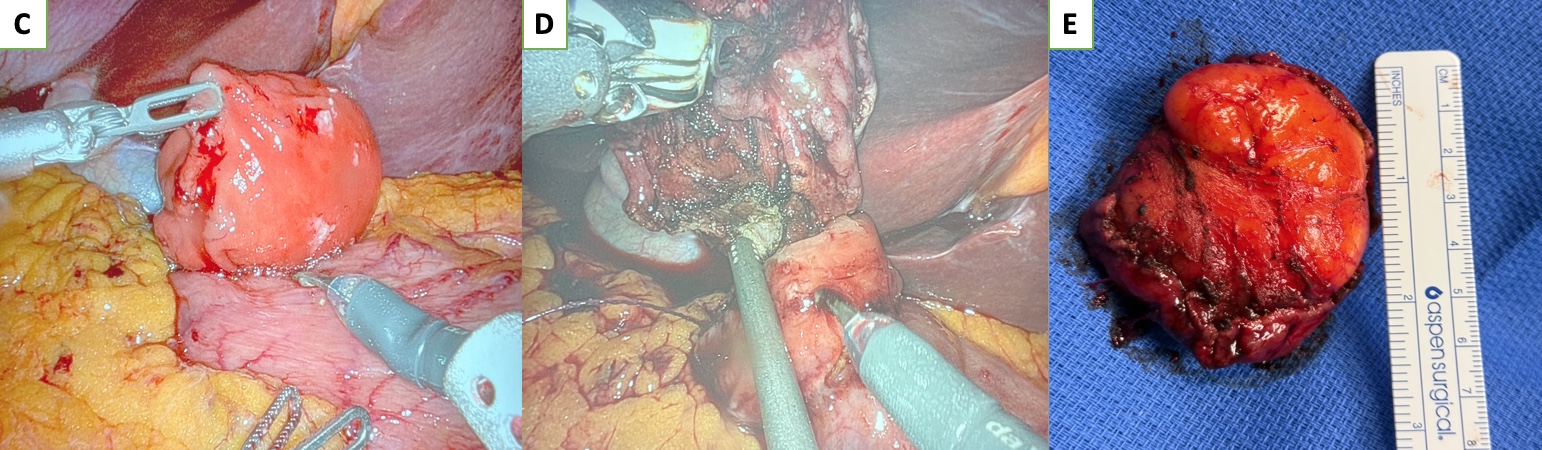
Figure: Figure C, D, and E show robotic surgical resection and measurement of resected intraduodenal lipoma.
Disclosures:
Kenneth Barnett indicated no relevant financial relationships.
Jiteshwar Pannu indicated no relevant financial relationships.
Apurva Shrigiriwar indicated no relevant financial relationships.
Donald Kastens indicated no relevant financial relationships.
Kenneth C. Barnett, MD, Jiteshwar Pannu, MD, Apurva Shrigiriwar, MD, Donald Kastens, MD. P1982 - A Case of Pyloroduodenal Intussusception Secondary to an Intraduodenal Lipoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Oklahoma Health Sciences Center, Oklahoma City, OK
Introduction: Gastrointestinal (GI) lipomas are benign submucosal tumors that are usually encountered as incidental findings in asymptomatic patients, but can rarely lead to complications such as small bowel obstruction (SBO), intussusception and bleeding from overlying ulceration. Herein, we present a case of an intraduodenal lipoma causing pyloroduodenal intussusception, highlighting the importance of timely diagnosis and intervention to prevent bowel obstruction.
Case Description/
Methods: An 82-year-old male, was admitted with intractable nausea and vomiting. Physical exam revealed a mildly distended abdomen and minimal epigastric tenderness without palpable mass. CT abdomen with contrast revealed non-obstructing pyloroduodenal intussusception with an intraduodenal lipoma (5.1x 4 x 3.7 cm) in D2 likely being a lead point for intussusception within the pyloric antrum and D1 telescoping into D2 (Figure A/B). Given the above findings, an urgent general surgery consult was sought. Patient was subsequently taken to the operating room for a robotic reduction, resection, and Heineke-Mikulicz pyloroplasty (Figure C/D). Intraoperative findings revealed a pedunculated duodenal bulb lipoma with a broad stalk. Pathology was consistent with 5.2 x 4.5 x 2.5 cm submucosal lipoma (Figure E). Patient did well post-operatively with gradual advancement of diet.
Discussion: Gastric and duodenal lipomas account for about 4% of all GI lipomas. While usually asymptomatic, larger lipomas (particularly those >2 cm) can cause complications like bleeding, SBO, or intussusception. Adult intussusception is rare and typically has a pathological lead point, unlike in children, and is commonly seen in the jejunum/ileum due to retroperitoneal adherence of the duodenum (except D1 segment). Lipomas (especially when submucosal and pedunculated), can act as such lead points, resulting in intermittent or acute symptoms similar to our case. CT is the imaging modality of choice, showing characteristic fat-density masses and sometimes the "target" sign of intussusception. Management depends on symptoms and suspicion of malignancy; endoscopic resection can be considered for smaller, low risk lesions whereas surgical approach is preferred for larger, symptomatic lesions causing complications. In this case, an intraduodenal lipoma served as the lead point for intussusception, an uncommon but important cause of adult SBO, necessitating prompt recognition and surgical management.
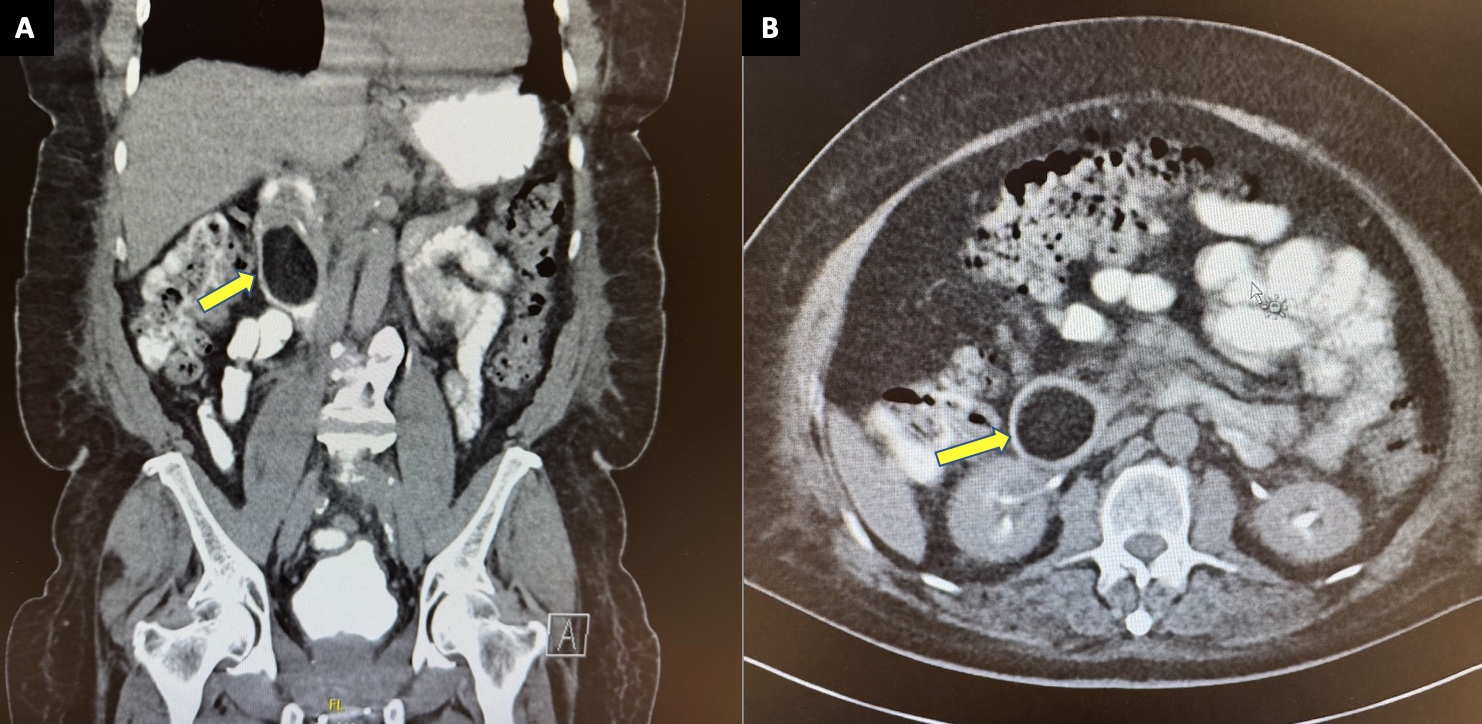
Figure: Figure A (Coronal) and B (Axial) showing large 5.1 x 4 x 3.7cm intraduodenal lipoma and pyloroduodenal intussusception (yellow arrow).
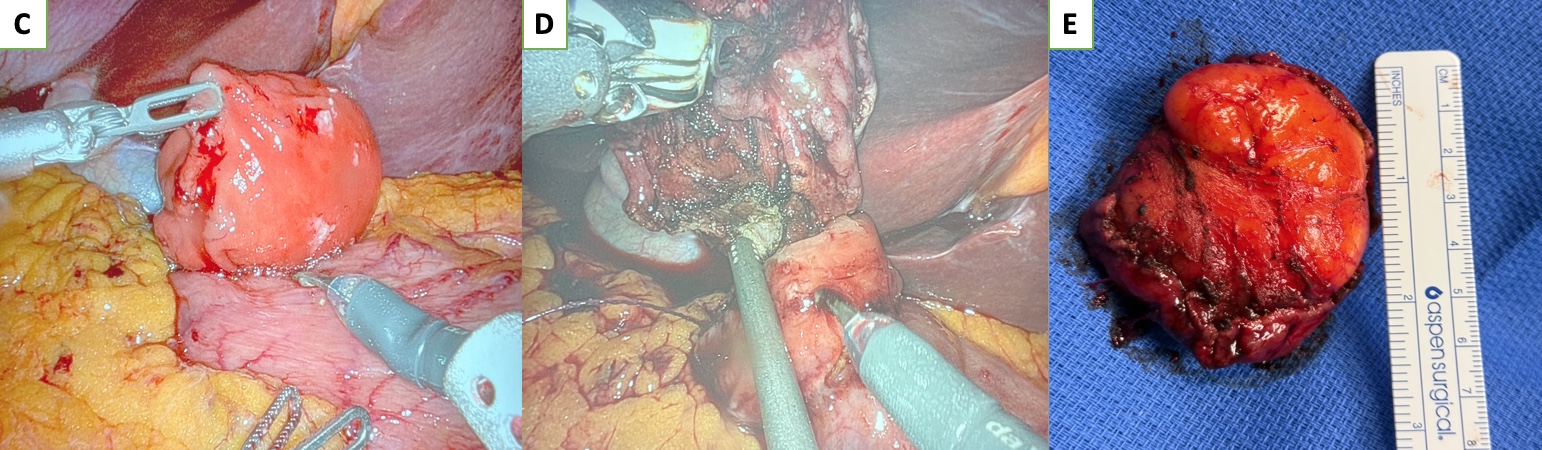
Figure: Figure C, D, and E show robotic surgical resection and measurement of resected intraduodenal lipoma.
Disclosures:
Kenneth Barnett indicated no relevant financial relationships.
Jiteshwar Pannu indicated no relevant financial relationships.
Apurva Shrigiriwar indicated no relevant financial relationships.
Donald Kastens indicated no relevant financial relationships.
Kenneth C. Barnett, MD, Jiteshwar Pannu, MD, Apurva Shrigiriwar, MD, Donald Kastens, MD. P1982 - A Case of Pyloroduodenal Intussusception Secondary to an Intraduodenal Lipoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
