Sunday Poster Session
Category: Small Intestine
P1981 - A Dark Clue to an Unusual Link - Reno-duodenal Fistula Presenting as Melena
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Rama Hussein, DO (she/her/hers)
Mount Sinai West, Icahn School of Medicine at Mount Sinai
New York City, NY
Presenting Author(s)
Rama Hussein, DO1, Zoe Lawrence, MD2
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York City, NY; 2Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: The prevalence of duodenal fistulas is rare and causes are limited. Perforation of peptic ulcers, severe pancreatitis, complications of intervention such as gastrectomy and endoscopic retrograde cholangio-pancreatography (ERCP) as well as some malignancies have been found to be the causes of duodenal fistulas1. Reno-duodenal fistulas are especially rare and account for < 1.0% of fistulas found between the gastrointestinal and urinary tracts2. Chronic inflammation in the kidneys may lend to fistulization with the duodenum due to their close proximity. We present a rare care of reno-duodenal fistula causing gastrointestinal bleeding.
Case Description/
Methods: An 86-year-old male with history of hypertension, hyperlipidemia, diabetes, H. pylori gastritis and anemia initially presented for generalized weakness, lower abdominal pain and four days of melena. On arrival, the patient's lab work was notable for acute anemia and leukocytosis. Computerized tomography (CT) Abdomen and Pelvis scan was notable for complete cystic and solid irregular degeneration of the right kidney with associated focal emphysema. He was admitted and his hospital course was notable for multiple episodes of melena requiring blood transfusions. Inpatient esophagogastroduodenoscopy (EGD) performed for the evaluation of melena revealed a 15mm fistula in the second portion of the duodenum surrounded by clotted blood (Figure 1.). Biopsies of the surrounding abnormal mucosa were consistent with metastatic carcinoma, consistent with renal origin and kidney biopsy confirmed the diagnosis of renal cell carcinoma. Following goals of care discussion, the patient was discharged to hospice.
Discussion: The presentation of melena in our patient with newly diagnosed renal cell carcinoma secondary to a reno-duodenal fistula emphasizes the need to include fistula formation on the differential when investigating gastrointestinal bleeding. Our case also highlights that although CT imaging did not indicate the presence of a fistula, emphysematous changes should prompt concerns not only of local inflammatory process but also of involvement of nearby air containing structures such as the luminal gastrointestinaI tract as well. This case draws to light the need to maintain a broad differential including rare presentations, particularly when patients are presenting with atypical symptoms for upper gastrointestinal bleeding.
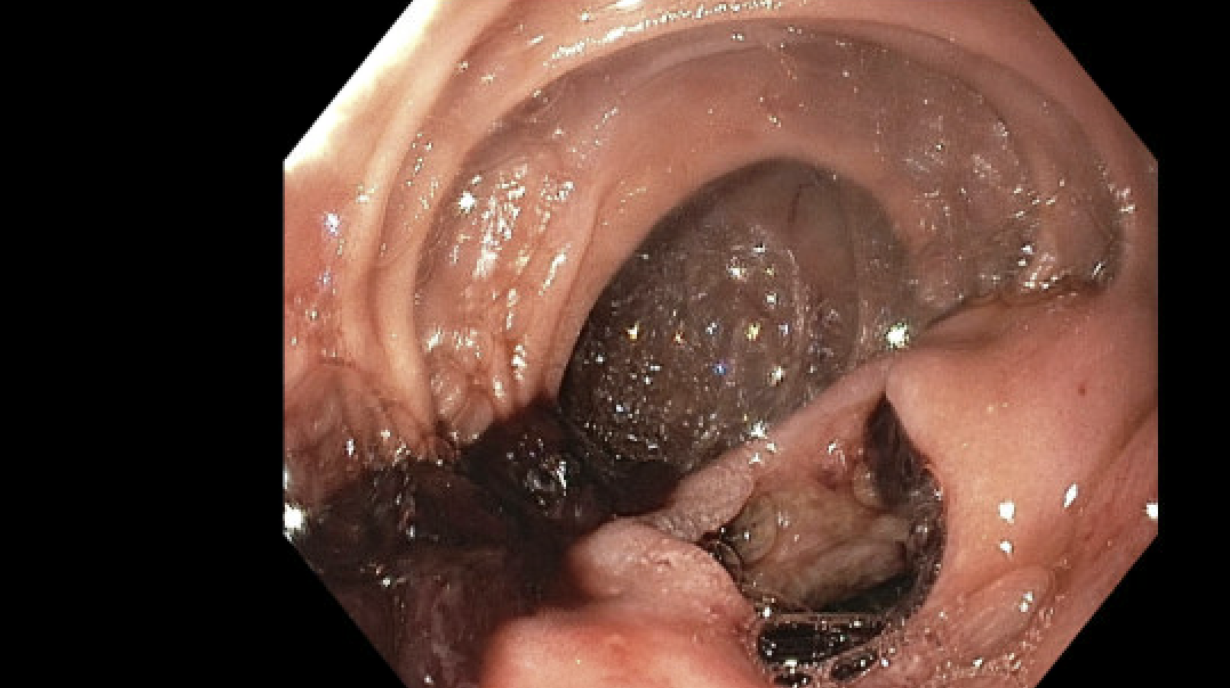
Figure: Fistula with associated thrombus in the second portion of the duodenum.
Disclosures:
Rama Hussein indicated no relevant financial relationships.
Zoe Lawrence indicated no relevant financial relationships.
Rama Hussein, DO1, Zoe Lawrence, MD2. P1981 - A Dark Clue to an Unusual Link - Reno-duodenal Fistula Presenting as Melena, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York City, NY; 2Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: The prevalence of duodenal fistulas is rare and causes are limited. Perforation of peptic ulcers, severe pancreatitis, complications of intervention such as gastrectomy and endoscopic retrograde cholangio-pancreatography (ERCP) as well as some malignancies have been found to be the causes of duodenal fistulas1. Reno-duodenal fistulas are especially rare and account for < 1.0% of fistulas found between the gastrointestinal and urinary tracts2. Chronic inflammation in the kidneys may lend to fistulization with the duodenum due to their close proximity. We present a rare care of reno-duodenal fistula causing gastrointestinal bleeding.
Case Description/
Methods: An 86-year-old male with history of hypertension, hyperlipidemia, diabetes, H. pylori gastritis and anemia initially presented for generalized weakness, lower abdominal pain and four days of melena. On arrival, the patient's lab work was notable for acute anemia and leukocytosis. Computerized tomography (CT) Abdomen and Pelvis scan was notable for complete cystic and solid irregular degeneration of the right kidney with associated focal emphysema. He was admitted and his hospital course was notable for multiple episodes of melena requiring blood transfusions. Inpatient esophagogastroduodenoscopy (EGD) performed for the evaluation of melena revealed a 15mm fistula in the second portion of the duodenum surrounded by clotted blood (Figure 1.). Biopsies of the surrounding abnormal mucosa were consistent with metastatic carcinoma, consistent with renal origin and kidney biopsy confirmed the diagnosis of renal cell carcinoma. Following goals of care discussion, the patient was discharged to hospice.
Discussion: The presentation of melena in our patient with newly diagnosed renal cell carcinoma secondary to a reno-duodenal fistula emphasizes the need to include fistula formation on the differential when investigating gastrointestinal bleeding. Our case also highlights that although CT imaging did not indicate the presence of a fistula, emphysematous changes should prompt concerns not only of local inflammatory process but also of involvement of nearby air containing structures such as the luminal gastrointestinaI tract as well. This case draws to light the need to maintain a broad differential including rare presentations, particularly when patients are presenting with atypical symptoms for upper gastrointestinal bleeding.
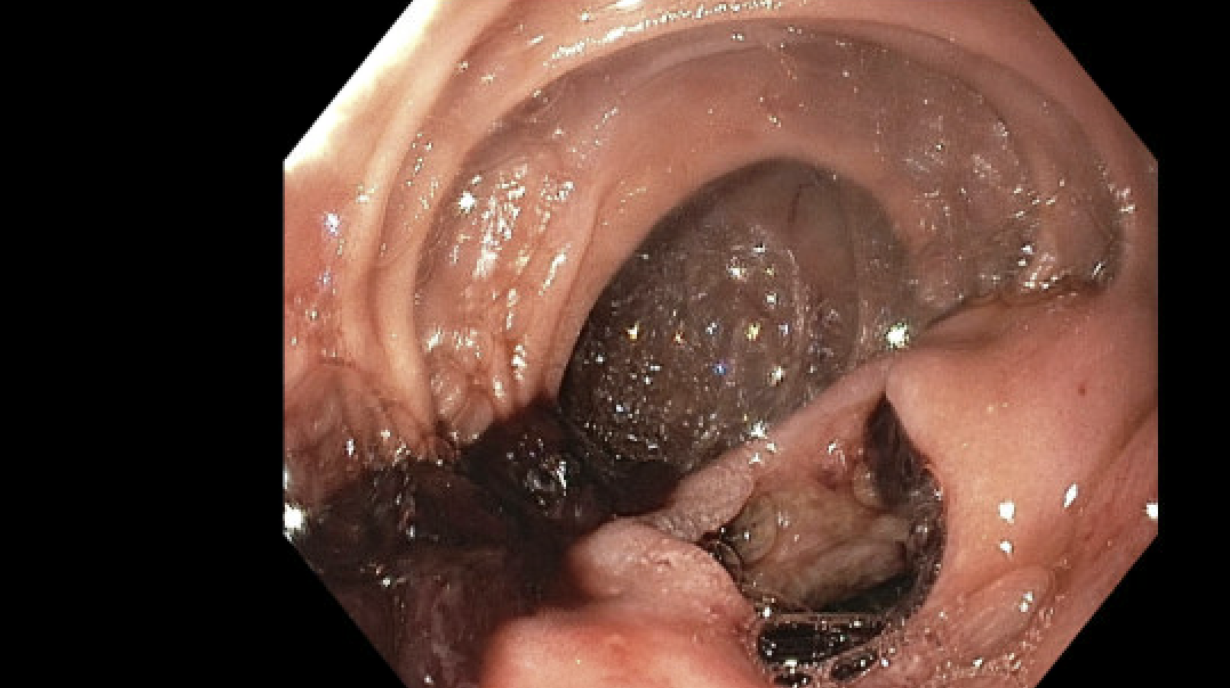
Figure: Fistula with associated thrombus in the second portion of the duodenum.
Disclosures:
Rama Hussein indicated no relevant financial relationships.
Zoe Lawrence indicated no relevant financial relationships.
Rama Hussein, DO1, Zoe Lawrence, MD2. P1981 - A Dark Clue to an Unusual Link - Reno-duodenal Fistula Presenting as Melena, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
