Sunday Poster Session
Category: Small Intestine
P1979 - Multifocal Small Bowel GISTs and Co-Existent NET in a Patient With Neurofibromatosis Type I: A Case Report and Review of the Literature
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Bianca Thakkar, DO
University of Connecticut Health
Farmington, CT
Presenting Author(s)
Bianca Thakkar, DO1, Teresa Da Cunha, MD2, Murali Dharan, 3
1University of Connecticut Health, Farmington, CT; 2University of Connecticut Health, Hartford, CT; 3Employed, Farmington, CT
Introduction: Neurofibromatosis type I (NF1) is a genetic syndrome characterized by mutations in the NF1 gene, often leading to development of multiple benign and malignant neoplasms. Among these, gastrointestinal stromal tumors (GISTs) represent a rare but notable manifestation. Unlike sporadic GISTs, those associated with NF1 typically present as multifocal lesions, predominantly in the small bowel, and are often wild-type for KIT and PDGFRA mutations, with important therapeutic implications.
Case Description/
Methods: A 62-year-old woman with known NF1 and prior duodenal neuroendocrine tumor (NET) presented with abdominal pain. Imaging revealed multiple small bowel masses. She underwent exploratory laparotomy with resection of 33 cm of jejunum containing three palpable masses and an appendectomy. Pathology demonstrated four distinct foci of GIST ranging from 2 mm to 2.8 cm. Immunohistochemistry supported the diagnosis of GIST. A residual duodenal lesion was noted intraoperatively but not resected. Subsequent EUS with tissue acquisition identified a 10.1 × 8.6 mm duodenal NET invading the submucosa and muscularis propria. MRI revealed an enhancing 0.8 cm lesion at the second-third portion of the duodenum and no significant uptake was noted on PET imaging. This lesion is being monitored.
Discussion: NF1-associated GISTs are clinically and genetically distinct from sporadic GISTs. They tend to be multifocal, located in the small intestine, and are frequently negative for KIT or PDGFRA mutations. Consequently, tyrosine kinase inhibitors like imatinib are often less effective. The co-occurrence of GIST and NET in NF1, as seen in this case, is extremely rare and poses diagnostic and management challenges. Surgical resection remains the mainstay of treatment, although the approach must be individualized due to the multifocality and complex anatomical involvement.
This case highlights the importance of recognizing the unique presentation and molecular behavior of NF1-associated GISTs. The coexistence of multifocal GIST and NET further complicates management, underscoring the need for a multidisciplinary approach. More research is needed to develop standardized protocols for this rare clinical scenario.
References:
1. Wang X, Wu Y, Cao X, Zhang X, Cheng Y, Kong L. Medicine (Baltimore), February 12, 2021, Volume 100, Issue 6, e24635.
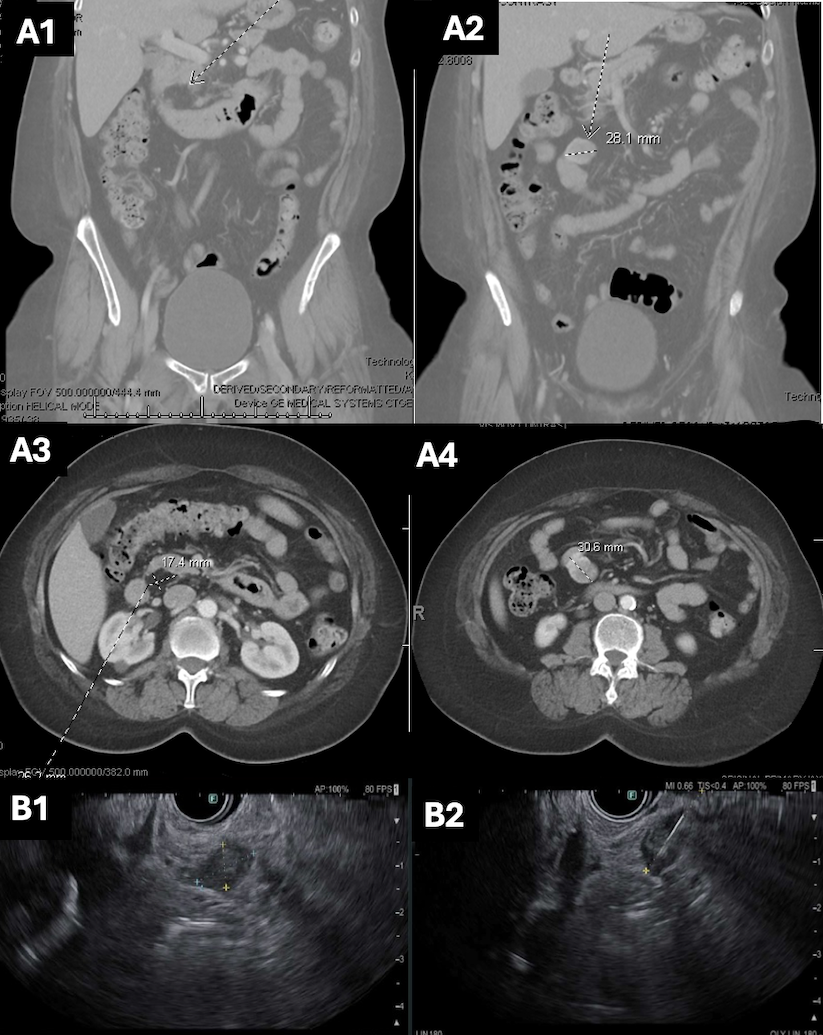
Figure: Figure 1:
A1-A4. CT Abdomen/pelvis with several non-obstructing small bowel masses visualized, concerning for gastrointestinal stromal tumors associated with NF1.
B1-B2. Endoscopic ultrasound with a mucosal lesion (B1) in the duodenum and an intramural (subepithelial) lesion (B2) in the duodenum that appeared to originate from within the muscularis propria. Fine needle aspiration was collected.
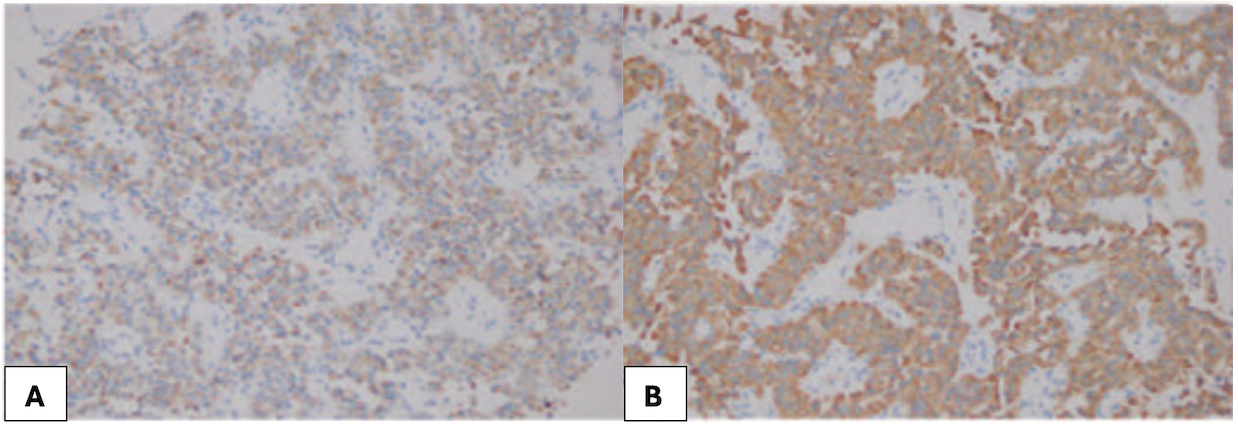
Figure: An example of immunohistochemistry findings of ultrasound-guided abdominal biopsy for neuroendocrine tumor. Hematoxylin-eosin staining (×200); Tumor cells are positive for Chromogranin A (A) and Synaptophysin (B) [1].
Disclosures:
Bianca Thakkar indicated no relevant financial relationships.
Teresa Da Cunha indicated no relevant financial relationships.
Murali Dharan indicated no relevant financial relationships.
Bianca Thakkar, DO1, Teresa Da Cunha, MD2, Murali Dharan, 3. P1979 - Multifocal Small Bowel GISTs and Co-Existent NET in a Patient With Neurofibromatosis Type I: A Case Report and Review of the Literature, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Connecticut Health, Farmington, CT; 2University of Connecticut Health, Hartford, CT; 3Employed, Farmington, CT
Introduction: Neurofibromatosis type I (NF1) is a genetic syndrome characterized by mutations in the NF1 gene, often leading to development of multiple benign and malignant neoplasms. Among these, gastrointestinal stromal tumors (GISTs) represent a rare but notable manifestation. Unlike sporadic GISTs, those associated with NF1 typically present as multifocal lesions, predominantly in the small bowel, and are often wild-type for KIT and PDGFRA mutations, with important therapeutic implications.
Case Description/
Methods: A 62-year-old woman with known NF1 and prior duodenal neuroendocrine tumor (NET) presented with abdominal pain. Imaging revealed multiple small bowel masses. She underwent exploratory laparotomy with resection of 33 cm of jejunum containing three palpable masses and an appendectomy. Pathology demonstrated four distinct foci of GIST ranging from 2 mm to 2.8 cm. Immunohistochemistry supported the diagnosis of GIST. A residual duodenal lesion was noted intraoperatively but not resected. Subsequent EUS with tissue acquisition identified a 10.1 × 8.6 mm duodenal NET invading the submucosa and muscularis propria. MRI revealed an enhancing 0.8 cm lesion at the second-third portion of the duodenum and no significant uptake was noted on PET imaging. This lesion is being monitored.
Discussion: NF1-associated GISTs are clinically and genetically distinct from sporadic GISTs. They tend to be multifocal, located in the small intestine, and are frequently negative for KIT or PDGFRA mutations. Consequently, tyrosine kinase inhibitors like imatinib are often less effective. The co-occurrence of GIST and NET in NF1, as seen in this case, is extremely rare and poses diagnostic and management challenges. Surgical resection remains the mainstay of treatment, although the approach must be individualized due to the multifocality and complex anatomical involvement.
This case highlights the importance of recognizing the unique presentation and molecular behavior of NF1-associated GISTs. The coexistence of multifocal GIST and NET further complicates management, underscoring the need for a multidisciplinary approach. More research is needed to develop standardized protocols for this rare clinical scenario.
References:
1. Wang X, Wu Y, Cao X, Zhang X, Cheng Y, Kong L. Medicine (Baltimore), February 12, 2021, Volume 100, Issue 6, e24635.
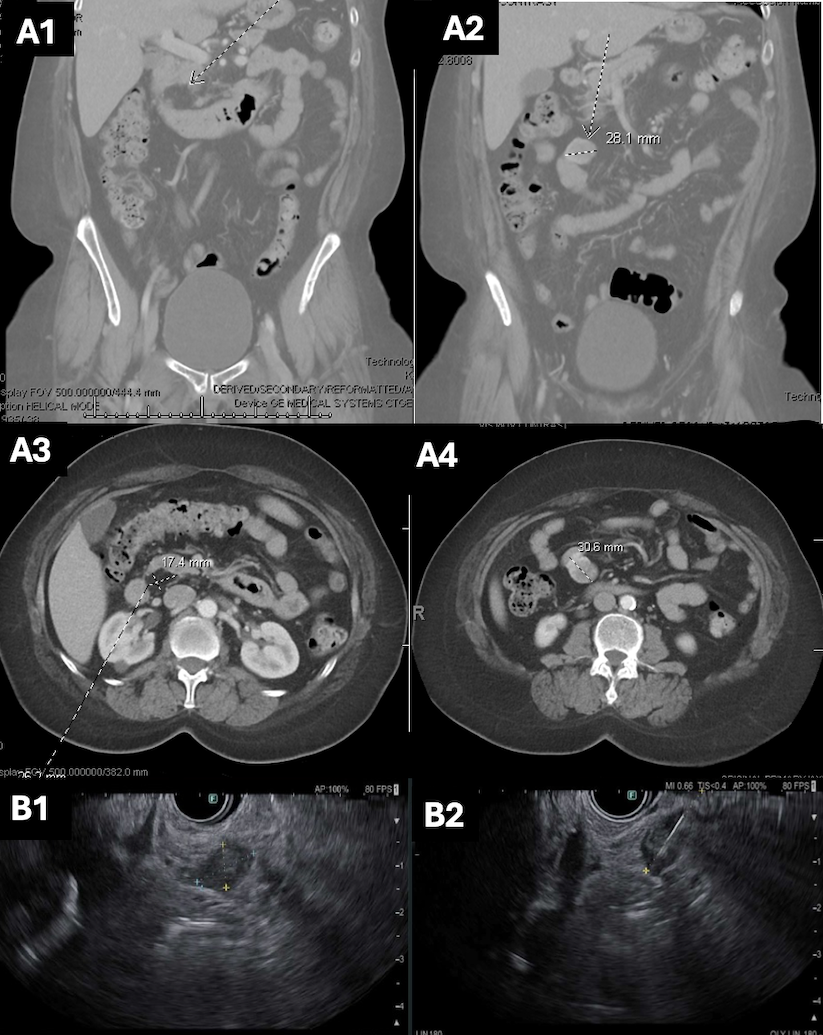
Figure: Figure 1:
A1-A4. CT Abdomen/pelvis with several non-obstructing small bowel masses visualized, concerning for gastrointestinal stromal tumors associated with NF1.
B1-B2. Endoscopic ultrasound with a mucosal lesion (B1) in the duodenum and an intramural (subepithelial) lesion (B2) in the duodenum that appeared to originate from within the muscularis propria. Fine needle aspiration was collected.
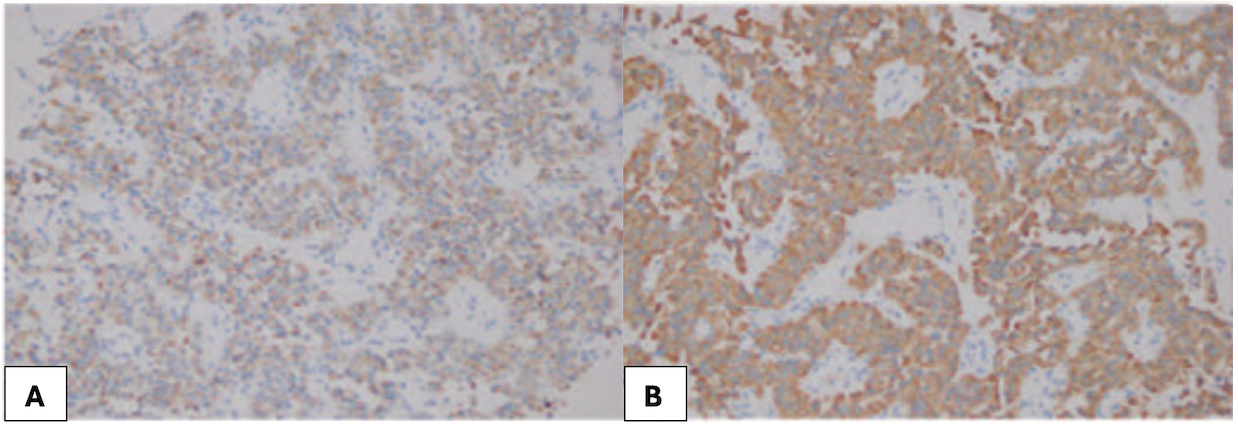
Figure: An example of immunohistochemistry findings of ultrasound-guided abdominal biopsy for neuroendocrine tumor. Hematoxylin-eosin staining (×200); Tumor cells are positive for Chromogranin A (A) and Synaptophysin (B) [1].
Disclosures:
Bianca Thakkar indicated no relevant financial relationships.
Teresa Da Cunha indicated no relevant financial relationships.
Murali Dharan indicated no relevant financial relationships.
Bianca Thakkar, DO1, Teresa Da Cunha, MD2, Murali Dharan, 3. P1979 - Multifocal Small Bowel GISTs and Co-Existent NET in a Patient With Neurofibromatosis Type I: A Case Report and Review of the Literature, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
