Sunday Poster Session
Category: Small Intestine
P1977 - Small Bowel Eosinophilia With Eosinophilic Ascites
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- MS
Michael Shen, MD, PhD (he/him/his)
University of Pennsylvania Health System
Philadelphia, PA
Presenting Author(s)
Michael Shen, MD, PhD1, Renata Lerer, MD1, Nathalie Mejia, BA2, Kristen Stashek, MD3, Kristle L.. Lynch, MD4
1University of Pennsylvania Health System, Philadelphia, PA; 2University of Pennsylvania, Philadelphia, PA; 3Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA; 4The University of Pennsylvania, Philadelphia, PA
Introduction: Eosinophilic gastrointestinal diseases (EGIDs) are inflammatory disorders of aberrant eosinophil abundance that can manifest anywhere along the gastrointestinal lumen. Non-esophageal EGIDs including eosinophilic gastritis (EoG), eosinophilic enteritis (EoN), and eosinophilic colitis (EoC) often present with nonspecific symptoms with no formalized guidelines for their diagnosis or treatment.
Case Description/
Methods: A 71-year-old man with untreated HCV, asthma, and allergic rhinitis presented to the emergency room with 3 weeks of postprandial abdominal pain, decreased appetite, 5 pound weight loss, and abdominal swelling. He had recent travel to Cuba and worked as a chef. Vitals were notable for heart rate of 112. Physical examination showed mild LLQ tenderness and mild abdominal distention. Abdominal CT showed abdominopelvic ascites, hepatic surface nodularity, thickening of the gastric body, and diffuse small bowel wall thickening. Labs were notable for moderate peripheral eosinophilia and elevated IgE (figure 1).
The patient underwent EGD with pathology showing duodenal mucosa with >50 eosinophils/HPF. He was discharged after his symptoms improved and repeat EGD 8 weeks later was normal. He was successfully treated for hepatitis C.
Four months later the patient was again hospitalized with worsening abdominal pain and 30 pound weight loss. He again had moderate peripheral eosinophilia and CT enterography showed mild thickening of jejunal loops. Push enteroscopy to mid-jejunum demonstrated erosions and erythema in the gastric antrum and duodenum along with inflammation and ulcerations in the jejunum (Figure 2a-d). Pathology showed a maximum of 83 eosinophils/HPF in the lamina propria of the duodenum and jejunum (Figure 2e-h).
Infectious disease and oncologic workup ruled out parasitic infections and malignancy, respectively, and a diagnosis of EoN was agreed upon. The patient's symptoms improved with initiation of oral prednisone and he was discharged to outpatient follow-up, where he was tapered off prednisone to budesonide.
Discussion: This patient case underscores the need for better understanding of the mechanisms underlying EGIDs. The vast differential diagnoses involving peripheral eosinophilia and nonspecific systemic symptoms made a definitive diagnosis challenging in this patient, especially with inconsistent endoscopic biopsy results. Development and validation of criteria that can specifically diagnose EGIDs will allow for faster treatment of these often debilitating disorders.
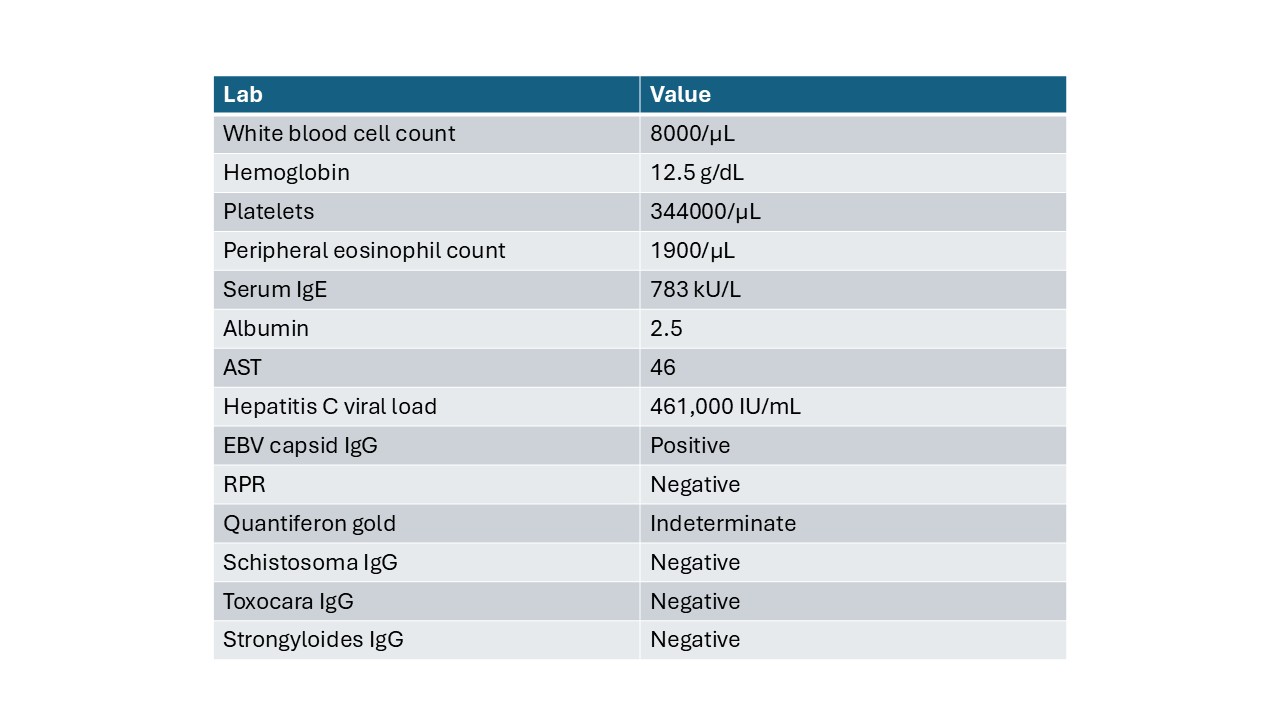
Figure: Figure 1. Notable lab values
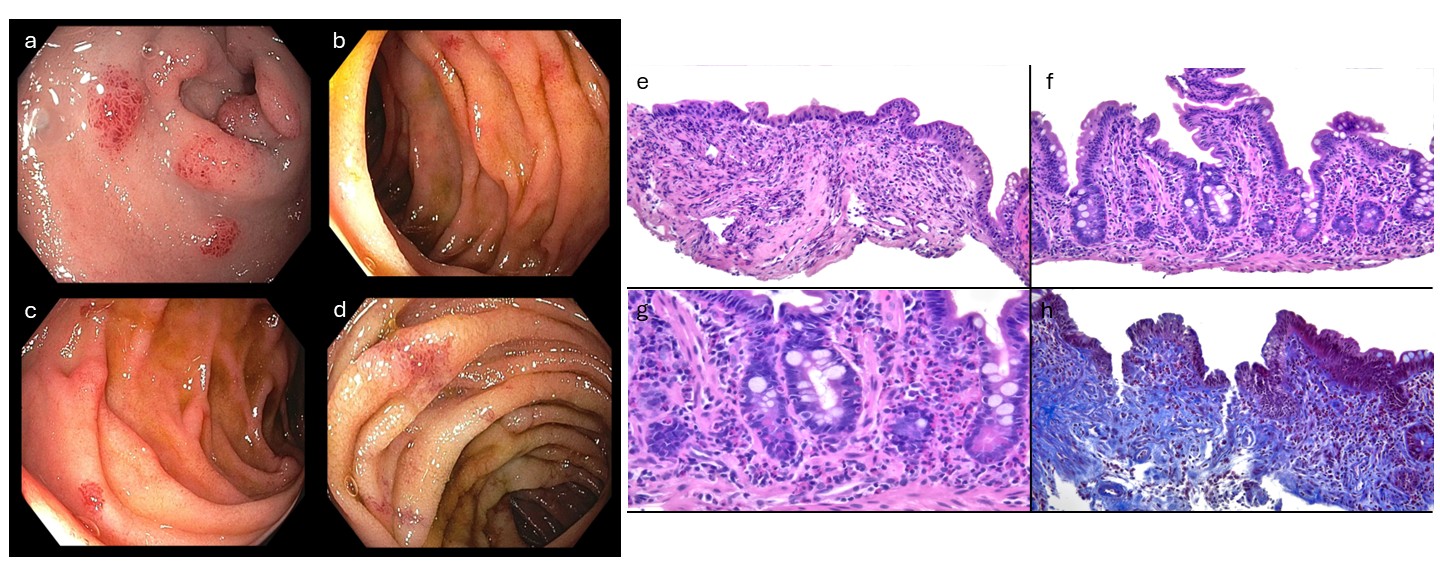
Figure: Figure 2. Endoscopic images taken during push enteroscopy performed during the patient’s second hospitalization demonstrating patchy small bowel erythema with areas of ulceration. a) duodenal bulb. b and c) duodenum. d) jejunum.
Representative images from histology obtained during patient’s second hospitalization. Images have had white balancing, background debris removal, sharpening and contrasting performed, but no manipulation to the histologic features seen .
e (small intestine, H&E): A section of small intestine showing crypt drop out and scattered lamina propria eosinophils.
f,g (small intestine, H&E, 100x, 400x): Microscopic examination showing an eosinophilic infiltrate involving both the lamina propria and the intestinal crypt epithelium.
h (small intestine, trichrome, 200x): Trichrome stain demonstrating lamina propria collagenization, as well as the eosinophilic infiltrate.
Disclosures:
Michael Shen indicated no relevant financial relationships.
Renata Lerer indicated no relevant financial relationships.
Nathalie Mejia indicated no relevant financial relationships.
Kristen Stashek indicated no relevant financial relationships.
Kristle Lynch: Medtronic – Consultant. Phathom – Consultant. Sanofi/Regeneron – Consultant. Uniquity – Consultant.
Michael Shen, MD, PhD1, Renata Lerer, MD1, Nathalie Mejia, BA2, Kristen Stashek, MD3, Kristle L.. Lynch, MD4. P1977 - Small Bowel Eosinophilia With Eosinophilic Ascites, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Pennsylvania Health System, Philadelphia, PA; 2University of Pennsylvania, Philadelphia, PA; 3Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA; 4The University of Pennsylvania, Philadelphia, PA
Introduction: Eosinophilic gastrointestinal diseases (EGIDs) are inflammatory disorders of aberrant eosinophil abundance that can manifest anywhere along the gastrointestinal lumen. Non-esophageal EGIDs including eosinophilic gastritis (EoG), eosinophilic enteritis (EoN), and eosinophilic colitis (EoC) often present with nonspecific symptoms with no formalized guidelines for their diagnosis or treatment.
Case Description/
Methods: A 71-year-old man with untreated HCV, asthma, and allergic rhinitis presented to the emergency room with 3 weeks of postprandial abdominal pain, decreased appetite, 5 pound weight loss, and abdominal swelling. He had recent travel to Cuba and worked as a chef. Vitals were notable for heart rate of 112. Physical examination showed mild LLQ tenderness and mild abdominal distention. Abdominal CT showed abdominopelvic ascites, hepatic surface nodularity, thickening of the gastric body, and diffuse small bowel wall thickening. Labs were notable for moderate peripheral eosinophilia and elevated IgE (figure 1).
The patient underwent EGD with pathology showing duodenal mucosa with >50 eosinophils/HPF. He was discharged after his symptoms improved and repeat EGD 8 weeks later was normal. He was successfully treated for hepatitis C.
Four months later the patient was again hospitalized with worsening abdominal pain and 30 pound weight loss. He again had moderate peripheral eosinophilia and CT enterography showed mild thickening of jejunal loops. Push enteroscopy to mid-jejunum demonstrated erosions and erythema in the gastric antrum and duodenum along with inflammation and ulcerations in the jejunum (Figure 2a-d). Pathology showed a maximum of 83 eosinophils/HPF in the lamina propria of the duodenum and jejunum (Figure 2e-h).
Infectious disease and oncologic workup ruled out parasitic infections and malignancy, respectively, and a diagnosis of EoN was agreed upon. The patient's symptoms improved with initiation of oral prednisone and he was discharged to outpatient follow-up, where he was tapered off prednisone to budesonide.
Discussion: This patient case underscores the need for better understanding of the mechanisms underlying EGIDs. The vast differential diagnoses involving peripheral eosinophilia and nonspecific systemic symptoms made a definitive diagnosis challenging in this patient, especially with inconsistent endoscopic biopsy results. Development and validation of criteria that can specifically diagnose EGIDs will allow for faster treatment of these often debilitating disorders.
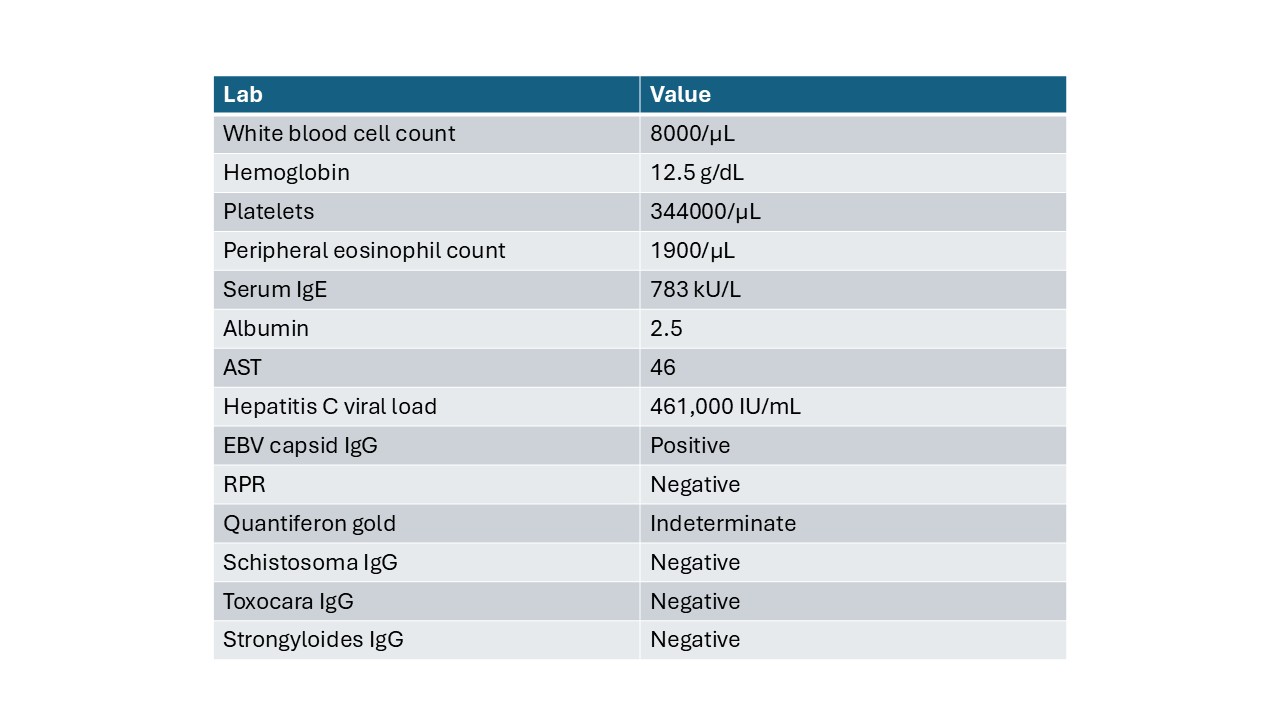
Figure: Figure 1. Notable lab values
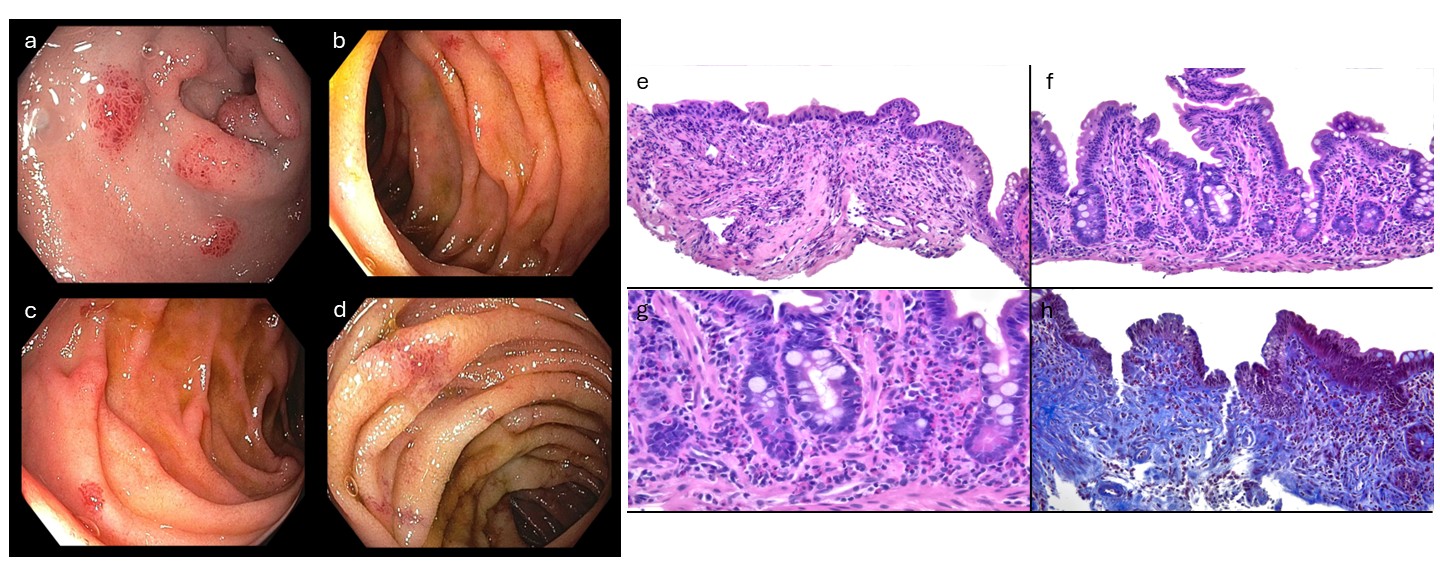
Figure: Figure 2. Endoscopic images taken during push enteroscopy performed during the patient’s second hospitalization demonstrating patchy small bowel erythema with areas of ulceration. a) duodenal bulb. b and c) duodenum. d) jejunum.
Representative images from histology obtained during patient’s second hospitalization. Images have had white balancing, background debris removal, sharpening and contrasting performed, but no manipulation to the histologic features seen .
e (small intestine, H&E): A section of small intestine showing crypt drop out and scattered lamina propria eosinophils.
f,g (small intestine, H&E, 100x, 400x): Microscopic examination showing an eosinophilic infiltrate involving both the lamina propria and the intestinal crypt epithelium.
h (small intestine, trichrome, 200x): Trichrome stain demonstrating lamina propria collagenization, as well as the eosinophilic infiltrate.
Disclosures:
Michael Shen indicated no relevant financial relationships.
Renata Lerer indicated no relevant financial relationships.
Nathalie Mejia indicated no relevant financial relationships.
Kristen Stashek indicated no relevant financial relationships.
Kristle Lynch: Medtronic – Consultant. Phathom – Consultant. Sanofi/Regeneron – Consultant. Uniquity – Consultant.
Michael Shen, MD, PhD1, Renata Lerer, MD1, Nathalie Mejia, BA2, Kristen Stashek, MD3, Kristle L.. Lynch, MD4. P1977 - Small Bowel Eosinophilia With Eosinophilic Ascites, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
