Sunday Poster Session
Category: Small Intestine
P1972 - Diagnostic Yield of Duodenal Biopsy in Unexplained Chronic Diarrhea: A Case of Duodenal AL Amyloidosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Tamiru B. Berake, MD (he/him/his)
Tufts Medical Center
Boston, MA
Presenting Author(s)
Tamiru B. Berake, MD1, Ariel Fischer, MD1, Lense Negash, MD2, Wafa Sarraj, MD3, Erik Holzwanger, MD1, Raymond Comenzo, MD1, Sonia Friedman, MD1
1Tufts Medical Center, Boston, MA; 2New York Medical College, Manhattan, NY; 3Tufts medicine, Boston, MA
Introduction: Duodenal AL (light chain) amyloidosis is a rare but critical cause of chronic diarrhea, often overlooked due to nonspecific symptoms and normal endoscopic findings. Duodenal biopsy with Congo red staining is essential for diagnosis.
Case Description/
Methods: A 78-year-old female with a six-year history of smoldering multiple myeloma presented with two years of progressive, non-bloody watery diarrhea (8–12 episodes/day), 40-pound weight loss, and signs of malabsorption. Extensive GI and infectious workup was unremarkable. Fecal pancreatic elastase was severely reduced (< 10 µg/g).
Upper endoscopy revealed mild duodenal mucosal changes. Duodenal biopsies demonstrated focal lymphangiectasia and thickened submucosal vessels with amorphous eosinophilic deposits on hematoxylin and eosin staining. Congo red stain revealed salmon-pink amyloid deposits, and polarized light microscopy confirmed apple-green birefringence, diagnostic of amyloidosis.
Serum free light chain assay revealed elevated lambda chains (72.9 mg/L) with a skewed kappa/lambda ratio. SPEP showed a monoclonal IgG spike (10.9 g/L). Bone marrow biopsy revealed 10–15% clonal plasma cells with vascular Congo red–positive deposits. Cytogenetics showed monosomy 17, consistent with high-risk plasma cell dyscrasia. She was diagnosed with systemic AL amyloidosis involving the duodenum and pancreas, in the setting of progression to active multiple myeloma.
The patient was initiated on Dara-CyBorD (daratumumab, cyclophosphamide, bortezomib, dexamethasone) and responded rapidly, with lambda chains decreasing to 18.6 mg/L after one cycle. She was also started on pancreatic enzyme replacement therapy, which improved stool consistency and frequency.
Discussion: This case highlights the important role of duodenal biopsy in diagnosing chronic diarrhea of unknown cause, particularly in patients with plasma cell disorders. Even when endoscopic findings appear normal, targeted biopsies using Congo red staining can lead to a diagnosis of gastrointestinal AL amyloidosis. Histological confirmation should be sought in patients experiencing ongoing symptoms, malabsorption, or those with known plasma cell dyscrasias
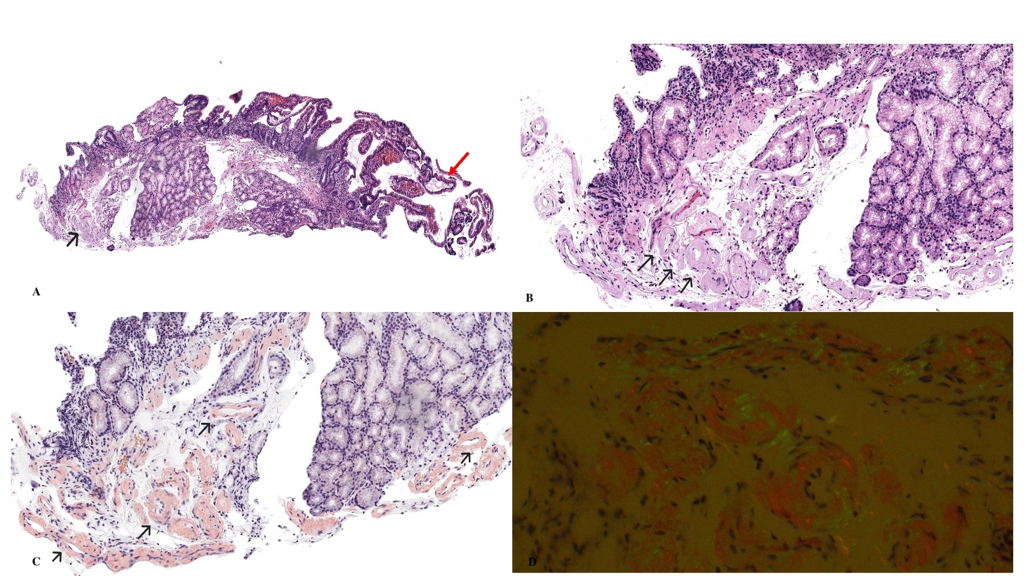
Figure: A. Duodenal biopsy showing focal lymphangiectasia (red arrow) and thickened submucosal blood vessels (black arrow).
B. Higher magnification demonstrates amorphous eosinophilic (hyaline) material deposits within the vessel walls (black arrows).
C. Congo red stain of the same section reveals homogeneous salmon-pink amyloid deposits within the vessel walls (black arrows).
D. Under polarized light, the blood vessels exhibit characteristic apple-green birefringence, consistent with amyloid deposition
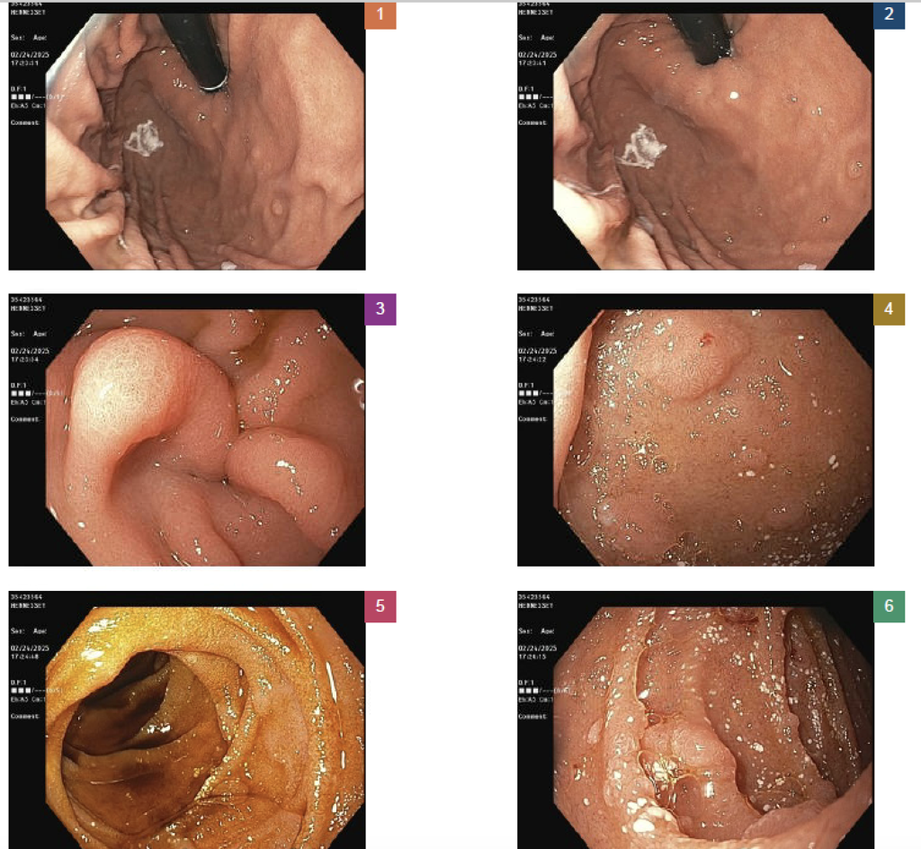
Figure: Duodenal lymphangiectasia and villous changes on esophagogastroduodenoscopy
Disclosures:
Tamiru Berake indicated no relevant financial relationships.
Ariel Fischer indicated no relevant financial relationships.
Lense Negash indicated no relevant financial relationships.
Wafa Sarraj indicated no relevant financial relationships.
Erik Holzwanger indicated no relevant financial relationships.
Raymond Comenzo indicated no relevant financial relationships.
Sonia Friedman indicated no relevant financial relationships.
Tamiru B. Berake, MD1, Ariel Fischer, MD1, Lense Negash, MD2, Wafa Sarraj, MD3, Erik Holzwanger, MD1, Raymond Comenzo, MD1, Sonia Friedman, MD1. P1972 - Diagnostic Yield of Duodenal Biopsy in Unexplained Chronic Diarrhea: A Case of Duodenal AL Amyloidosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Tufts Medical Center, Boston, MA; 2New York Medical College, Manhattan, NY; 3Tufts medicine, Boston, MA
Introduction: Duodenal AL (light chain) amyloidosis is a rare but critical cause of chronic diarrhea, often overlooked due to nonspecific symptoms and normal endoscopic findings. Duodenal biopsy with Congo red staining is essential for diagnosis.
Case Description/
Methods: A 78-year-old female with a six-year history of smoldering multiple myeloma presented with two years of progressive, non-bloody watery diarrhea (8–12 episodes/day), 40-pound weight loss, and signs of malabsorption. Extensive GI and infectious workup was unremarkable. Fecal pancreatic elastase was severely reduced (< 10 µg/g).
Upper endoscopy revealed mild duodenal mucosal changes. Duodenal biopsies demonstrated focal lymphangiectasia and thickened submucosal vessels with amorphous eosinophilic deposits on hematoxylin and eosin staining. Congo red stain revealed salmon-pink amyloid deposits, and polarized light microscopy confirmed apple-green birefringence, diagnostic of amyloidosis.
Serum free light chain assay revealed elevated lambda chains (72.9 mg/L) with a skewed kappa/lambda ratio. SPEP showed a monoclonal IgG spike (10.9 g/L). Bone marrow biopsy revealed 10–15% clonal plasma cells with vascular Congo red–positive deposits. Cytogenetics showed monosomy 17, consistent with high-risk plasma cell dyscrasia. She was diagnosed with systemic AL amyloidosis involving the duodenum and pancreas, in the setting of progression to active multiple myeloma.
The patient was initiated on Dara-CyBorD (daratumumab, cyclophosphamide, bortezomib, dexamethasone) and responded rapidly, with lambda chains decreasing to 18.6 mg/L after one cycle. She was also started on pancreatic enzyme replacement therapy, which improved stool consistency and frequency.
Discussion: This case highlights the important role of duodenal biopsy in diagnosing chronic diarrhea of unknown cause, particularly in patients with plasma cell disorders. Even when endoscopic findings appear normal, targeted biopsies using Congo red staining can lead to a diagnosis of gastrointestinal AL amyloidosis. Histological confirmation should be sought in patients experiencing ongoing symptoms, malabsorption, or those with known plasma cell dyscrasias
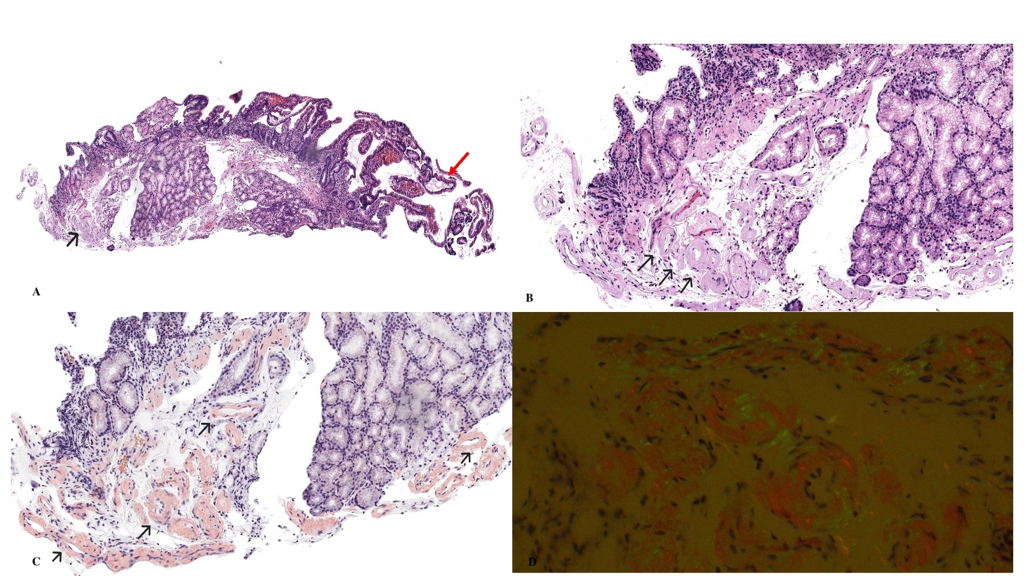
Figure: A. Duodenal biopsy showing focal lymphangiectasia (red arrow) and thickened submucosal blood vessels (black arrow).
B. Higher magnification demonstrates amorphous eosinophilic (hyaline) material deposits within the vessel walls (black arrows).
C. Congo red stain of the same section reveals homogeneous salmon-pink amyloid deposits within the vessel walls (black arrows).
D. Under polarized light, the blood vessels exhibit characteristic apple-green birefringence, consistent with amyloid deposition
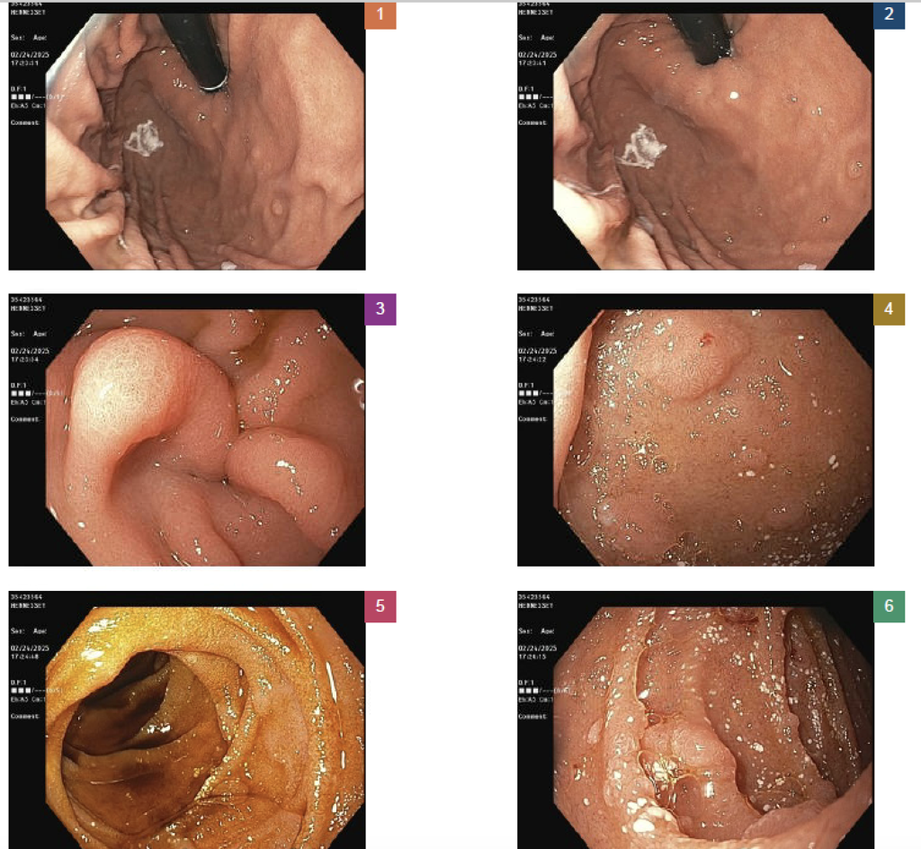
Figure: Duodenal lymphangiectasia and villous changes on esophagogastroduodenoscopy
Disclosures:
Tamiru Berake indicated no relevant financial relationships.
Ariel Fischer indicated no relevant financial relationships.
Lense Negash indicated no relevant financial relationships.
Wafa Sarraj indicated no relevant financial relationships.
Erik Holzwanger indicated no relevant financial relationships.
Raymond Comenzo indicated no relevant financial relationships.
Sonia Friedman indicated no relevant financial relationships.
Tamiru B. Berake, MD1, Ariel Fischer, MD1, Lense Negash, MD2, Wafa Sarraj, MD3, Erik Holzwanger, MD1, Raymond Comenzo, MD1, Sonia Friedman, MD1. P1972 - Diagnostic Yield of Duodenal Biopsy in Unexplained Chronic Diarrhea: A Case of Duodenal AL Amyloidosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
