Sunday Poster Session
Category: Small Intestine
P1967 - Endoscopic Resection of an Incidental Gangliocytic Paraganglioma Complicated by Delayed Bleeding: Lessons in Procedural Planning
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Wesley Chow, MD (he/him/his)
Scripps Mercy Hospital
San Diego, CA
Presenting Author(s)
Wesley Chow, MD1, Evan Wilder, MD2, Olivia Lanser, MD2, Phataraporn Thorson, MD3, Douglas Hunt, MD3, Han Zhang, MD2
1Scripps Mercy Hospital, San Diego, CA; 2Scripps Green Hospital, La Jolla, CA; 3Scripps Clinic, La Jolla, CA
Introduction: Gangliocytic paraganglioma (GP) is a rare neuroendocrine tumor typically located in the duodenum. While frequently asymptomatic, it may present with abdominal pain and gastrointestinal (GI) hemorrhage. Due to its resemblance to other GI malignancies, biopsy is required for diagnosis. Here, we present a case of an incidental gangliocytic paraganglioma removed endoscopically and complicated by delayed post-polypectomy bleeding.
Case Description/
Methods: A 60-year-old male with coronary artery disease (stents placed 2 years prior, on dual antiplatelet, aspirin and plavix, therapy (DAPT)), thyroid cancer with hemithyroidectomy and Parkinson's disease presented with dysphagia and abdominal pain for one year. His labs and CT abdomen/pelvis were normal.
Esophagogastroduodenoscopy (EGD) found an atypical pedunculated submucosal mass in the second part of the duodenum with normal overlying mucosa. Endoscopic ultrasound (EUS) noted a 17.2 × 14.1 mm heterogenous, isoechoic mass with a hypoechoic nodularity at its apex and small feeding vessel on doppler. This mass was completely resected by hot snare polypectomy and two hemoclips were placed for hemostasis. Plavix was held for 7 days prior to the procedure. On pathology, immunohistochemical stain was positive for AE1/AE3, S100 protein, chromogranin, and synaptophysin and negative for CD117, confirming gangliocytic paraganglioma.
He presented five days post-polypectomy with melena and symptomatic anemia (Hgb 13.5 to 8.8 g/dL, baseline 15 g/dL) after resuming DAPT 1-day post-procedure. EGD noted bleeding at the polypectomy site that was controlled with epinephrine, bipolar cautery, and a hemoclip. DAPT was de-escalated to aspirin only. One year later, EGD and EUS found no residual tumor or evidence of lymphadenopathy.
Discussion: GPs are characterized by three histologic cell types: epithelioid (AE1/AE3), schwannian (S100), and ganglion (chromogranin or synaptophysin). Accurate diagnosis is essential to avoid misdiagnosis of more aggressive malignancies, such as GI stromal tumors or metastases. Endoscopic or surgical management depends on tumor size, location, and lymph node involvement. Few post-polypectomy bleeding for GPs, potentially from prominent feeding vessels, have been reported; however, no prior post-polypectomy cases that the authors could identify involved DAPT. This case highlights the need for careful planning and monitoring to minimize complications when approaching resection of atypical masses for patients on DAPT or anticoagulation.
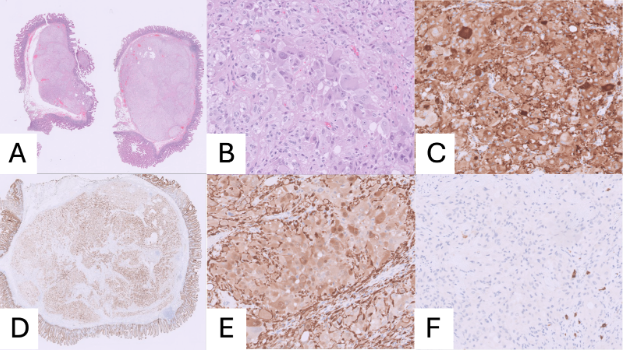
Figure: Figure 1. Endoscopic management of duodenal gangliocytic paraganglioma. (A) EGD showing pedunculated submucosal lesion. (B) EUS confirming 17.2 x 14.1 mm submucosal mass. (C) Endoscopic resection with hot snare resection. (D) Repeat EGD with active bleeding. (E) Post-treatment hemostasis. (F) Healed post-polypectomy site on surveillance EGD
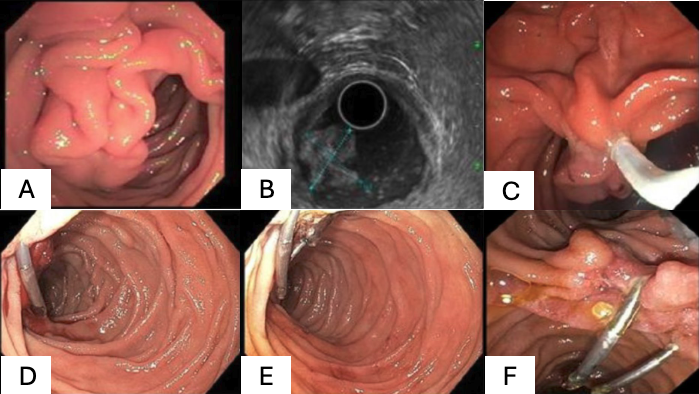
Figure: Figure 2: Microscopic histochemical evaluation for duodenal gangliocytic paraganglioma. (A) Low-power view of H&E stained section illustrating submucosal mass, (B) high-power view of H&E stain showing a nest of epithelioid cells admixed with ganglion cells and spindle cells, (C) ganglion and epithelioid cells show strong expression of S100 and synaptophysin by immunohistochemical staining, (D) low-power view of AE1/AE3 stained cells with heterogenous positivity in the epithelioid cells, (E) high-power view of S100 stained section highlights spindle and ganglion cells, and (F) all three cell types within the tumor tissue are negative for CD117 expression (GIST marker), while a small number of incidental mast cells are positive for this marker.
Disclosures:
Wesley Chow indicated no relevant financial relationships.
Evan Wilder indicated no relevant financial relationships.
Olivia Lanser indicated no relevant financial relationships.
Phataraporn Thorson indicated no relevant financial relationships.
Douglas Hunt indicated no relevant financial relationships.
Han Zhang indicated no relevant financial relationships.
Wesley Chow, MD1, Evan Wilder, MD2, Olivia Lanser, MD2, Phataraporn Thorson, MD3, Douglas Hunt, MD3, Han Zhang, MD2. P1967 - Endoscopic Resection of an Incidental Gangliocytic Paraganglioma Complicated by Delayed Bleeding: Lessons in Procedural Planning, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Scripps Mercy Hospital, San Diego, CA; 2Scripps Green Hospital, La Jolla, CA; 3Scripps Clinic, La Jolla, CA
Introduction: Gangliocytic paraganglioma (GP) is a rare neuroendocrine tumor typically located in the duodenum. While frequently asymptomatic, it may present with abdominal pain and gastrointestinal (GI) hemorrhage. Due to its resemblance to other GI malignancies, biopsy is required for diagnosis. Here, we present a case of an incidental gangliocytic paraganglioma removed endoscopically and complicated by delayed post-polypectomy bleeding.
Case Description/
Methods: A 60-year-old male with coronary artery disease (stents placed 2 years prior, on dual antiplatelet, aspirin and plavix, therapy (DAPT)), thyroid cancer with hemithyroidectomy and Parkinson's disease presented with dysphagia and abdominal pain for one year. His labs and CT abdomen/pelvis were normal.
Esophagogastroduodenoscopy (EGD) found an atypical pedunculated submucosal mass in the second part of the duodenum with normal overlying mucosa. Endoscopic ultrasound (EUS) noted a 17.2 × 14.1 mm heterogenous, isoechoic mass with a hypoechoic nodularity at its apex and small feeding vessel on doppler. This mass was completely resected by hot snare polypectomy and two hemoclips were placed for hemostasis. Plavix was held for 7 days prior to the procedure. On pathology, immunohistochemical stain was positive for AE1/AE3, S100 protein, chromogranin, and synaptophysin and negative for CD117, confirming gangliocytic paraganglioma.
He presented five days post-polypectomy with melena and symptomatic anemia (Hgb 13.5 to 8.8 g/dL, baseline 15 g/dL) after resuming DAPT 1-day post-procedure. EGD noted bleeding at the polypectomy site that was controlled with epinephrine, bipolar cautery, and a hemoclip. DAPT was de-escalated to aspirin only. One year later, EGD and EUS found no residual tumor or evidence of lymphadenopathy.
Discussion: GPs are characterized by three histologic cell types: epithelioid (AE1/AE3), schwannian (S100), and ganglion (chromogranin or synaptophysin). Accurate diagnosis is essential to avoid misdiagnosis of more aggressive malignancies, such as GI stromal tumors or metastases. Endoscopic or surgical management depends on tumor size, location, and lymph node involvement. Few post-polypectomy bleeding for GPs, potentially from prominent feeding vessels, have been reported; however, no prior post-polypectomy cases that the authors could identify involved DAPT. This case highlights the need for careful planning and monitoring to minimize complications when approaching resection of atypical masses for patients on DAPT or anticoagulation.
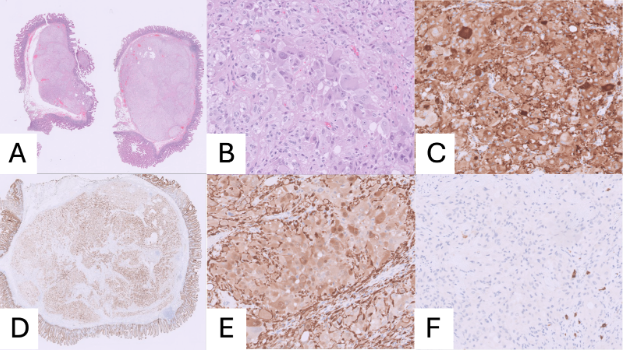
Figure: Figure 1. Endoscopic management of duodenal gangliocytic paraganglioma. (A) EGD showing pedunculated submucosal lesion. (B) EUS confirming 17.2 x 14.1 mm submucosal mass. (C) Endoscopic resection with hot snare resection. (D) Repeat EGD with active bleeding. (E) Post-treatment hemostasis. (F) Healed post-polypectomy site on surveillance EGD
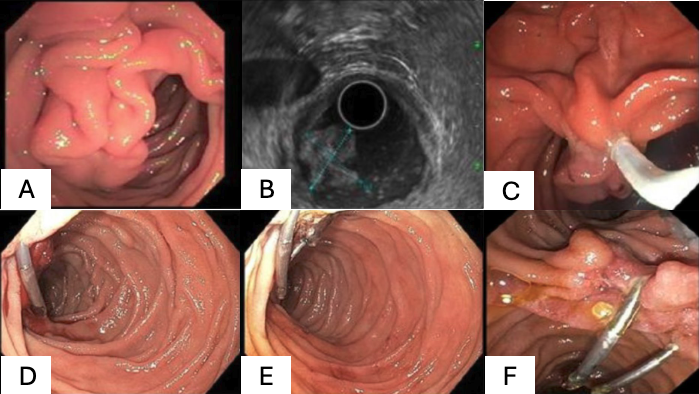
Figure: Figure 2: Microscopic histochemical evaluation for duodenal gangliocytic paraganglioma. (A) Low-power view of H&E stained section illustrating submucosal mass, (B) high-power view of H&E stain showing a nest of epithelioid cells admixed with ganglion cells and spindle cells, (C) ganglion and epithelioid cells show strong expression of S100 and synaptophysin by immunohistochemical staining, (D) low-power view of AE1/AE3 stained cells with heterogenous positivity in the epithelioid cells, (E) high-power view of S100 stained section highlights spindle and ganglion cells, and (F) all three cell types within the tumor tissue are negative for CD117 expression (GIST marker), while a small number of incidental mast cells are positive for this marker.
Disclosures:
Wesley Chow indicated no relevant financial relationships.
Evan Wilder indicated no relevant financial relationships.
Olivia Lanser indicated no relevant financial relationships.
Phataraporn Thorson indicated no relevant financial relationships.
Douglas Hunt indicated no relevant financial relationships.
Han Zhang indicated no relevant financial relationships.
Wesley Chow, MD1, Evan Wilder, MD2, Olivia Lanser, MD2, Phataraporn Thorson, MD3, Douglas Hunt, MD3, Han Zhang, MD2. P1967 - Endoscopic Resection of an Incidental Gangliocytic Paraganglioma Complicated by Delayed Bleeding: Lessons in Procedural Planning, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
