Sunday Poster Session
Category: Small Intestine
P1963 - Superior Mesenteric Artery Syndrome Masquerading as Cannabinoid Hyperemesis: A Case of Diagnostic Delay
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Aarohi Parikh, MD (she/her/hers)
HCA Houston Healthcare
Kingwood, TX
Presenting Author(s)
Aarohi Parikh, MD1, Supritha Chintamaneni, MBBS2, Hader Ismail, MD3
1HCA Houston Healthcare, Kingwood, TX; 2HCA Healthcare, Kingwood, TX; 3HCA Healthcare, Cypress, TX
Introduction: Superior mesenteric artery syndrome (SMAS) is a rare cause of upper gastrointestinal obstruction due to compression of the third portion of the duodenum between the aorta and the superior mesenteric artery. With an incidence of 0.1–0.3%, it often presents with nonspecific symptoms such as epigastric pain, nausea, and vomiting which closely mimic cannabinoid hyperemesis syndrome (CHS), particularly in patients with chronic cannabis use. These overlapping features frequently lead to misdiagnosis and delayed treatment. We present a case of a middle-aged woman repeatedly diagnosed with CHS who was ultimately found to have SMAS.
Case Description/
Methods: A 44-year-old female with a history of CHS presented with chronic diffuse abdominal pain, intractable nausea, and vomiting with a 20-pound weight loss over two months. She had six prior hospitalizations that included three abdominal CT scans and two EGDs, all unremarkable. Her symptoms were attributed to CHS, and she was discharged with symptomatic management every time. On this admission, vitals were unremarkable and she was cachectic with temporal wasting. Labs showed mild leukocytosis (12.9 ×10⁹/L) without anemia or lipase/amylase elevation. A repeat CT abdomen was again unrevealing. GI was consulted. EGD showed moderate gastric inflammation, bilious fluid, and duodenal erythema. A CT angiogram revealed an aortomesenteric angle of 8° and an aortomesenteric distance of 4 mm, confirming SMAS (Figure 1). She was transferred for a laparoscopic duodenojejunostomy which was completed without any acute complications. She is recovering post operatively and will follow up in clinic in 1-2 weeks.
Discussion: The symptom overlap between CHS and SMAS poses a diagnostic challenge as both may present with chronic nausea, vomiting, abdominal pain, and weight loss. In patients with cannabis use, providers may default to CHS, delaying the recognition of less common causes like SMAS. Diagnosis requires a high index of suspicion and vascular imaging, with an aortomesenteric angle < 25° and an aortomesenteric distance < 10 mm being diagnostic. Initial treatment is supportive, but definitive management requires a laparoscopic duodenojejunostomy. This case highlights the need to consider SMAS in patients with persistent symptoms and inconclusive workups. Early recognition is essential and maintaining a high degree of suspicion is critical to avoid delays in care.
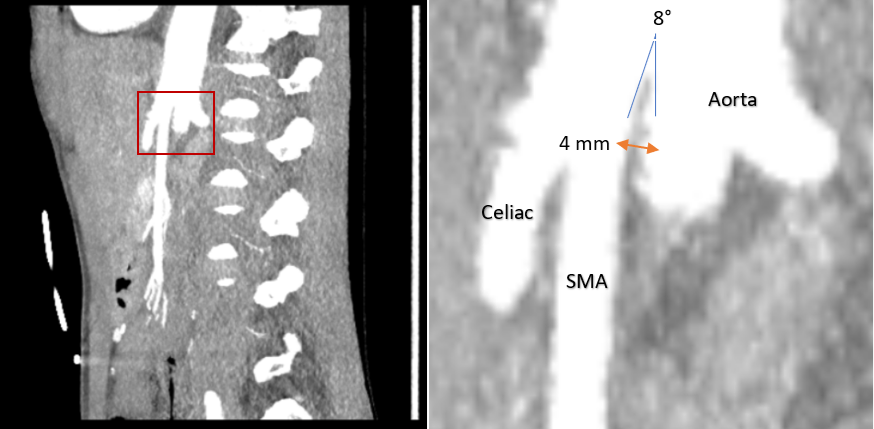
Figure: Figure 1. Image on the left represents a sagittal view of the aorta with the celiac artery and super mesenteric artery branches within the red box. The right image is a closer up image indicating an aortomesenteric angle of 8° and an aortomesenteric distance of 4 mm for superior mesenteric artery syndrome.
Disclosures:
Aarohi Parikh indicated no relevant financial relationships.
Supritha Chintamaneni indicated no relevant financial relationships.
Hader Ismail indicated no relevant financial relationships.
Aarohi Parikh, MD1, Supritha Chintamaneni, MBBS2, Hader Ismail, MD3. P1963 - Superior Mesenteric Artery Syndrome Masquerading as Cannabinoid Hyperemesis: A Case of Diagnostic Delay, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1HCA Houston Healthcare, Kingwood, TX; 2HCA Healthcare, Kingwood, TX; 3HCA Healthcare, Cypress, TX
Introduction: Superior mesenteric artery syndrome (SMAS) is a rare cause of upper gastrointestinal obstruction due to compression of the third portion of the duodenum between the aorta and the superior mesenteric artery. With an incidence of 0.1–0.3%, it often presents with nonspecific symptoms such as epigastric pain, nausea, and vomiting which closely mimic cannabinoid hyperemesis syndrome (CHS), particularly in patients with chronic cannabis use. These overlapping features frequently lead to misdiagnosis and delayed treatment. We present a case of a middle-aged woman repeatedly diagnosed with CHS who was ultimately found to have SMAS.
Case Description/
Methods: A 44-year-old female with a history of CHS presented with chronic diffuse abdominal pain, intractable nausea, and vomiting with a 20-pound weight loss over two months. She had six prior hospitalizations that included three abdominal CT scans and two EGDs, all unremarkable. Her symptoms were attributed to CHS, and she was discharged with symptomatic management every time. On this admission, vitals were unremarkable and she was cachectic with temporal wasting. Labs showed mild leukocytosis (12.9 ×10⁹/L) without anemia or lipase/amylase elevation. A repeat CT abdomen was again unrevealing. GI was consulted. EGD showed moderate gastric inflammation, bilious fluid, and duodenal erythema. A CT angiogram revealed an aortomesenteric angle of 8° and an aortomesenteric distance of 4 mm, confirming SMAS (Figure 1). She was transferred for a laparoscopic duodenojejunostomy which was completed without any acute complications. She is recovering post operatively and will follow up in clinic in 1-2 weeks.
Discussion: The symptom overlap between CHS and SMAS poses a diagnostic challenge as both may present with chronic nausea, vomiting, abdominal pain, and weight loss. In patients with cannabis use, providers may default to CHS, delaying the recognition of less common causes like SMAS. Diagnosis requires a high index of suspicion and vascular imaging, with an aortomesenteric angle < 25° and an aortomesenteric distance < 10 mm being diagnostic. Initial treatment is supportive, but definitive management requires a laparoscopic duodenojejunostomy. This case highlights the need to consider SMAS in patients with persistent symptoms and inconclusive workups. Early recognition is essential and maintaining a high degree of suspicion is critical to avoid delays in care.
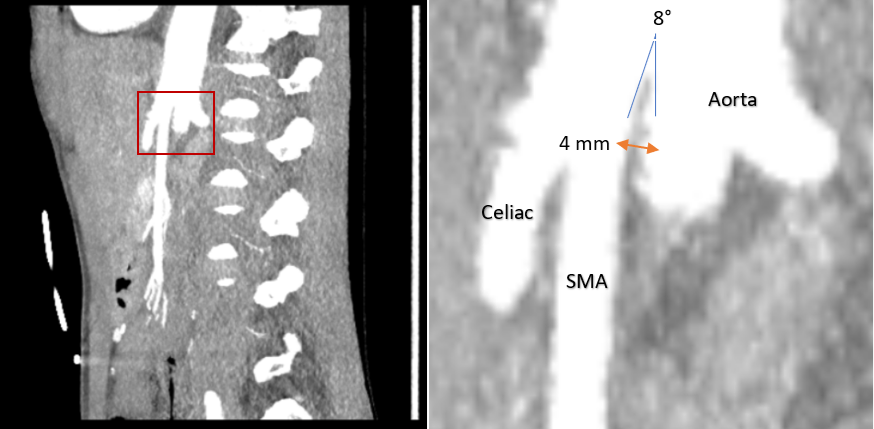
Figure: Figure 1. Image on the left represents a sagittal view of the aorta with the celiac artery and super mesenteric artery branches within the red box. The right image is a closer up image indicating an aortomesenteric angle of 8° and an aortomesenteric distance of 4 mm for superior mesenteric artery syndrome.
Disclosures:
Aarohi Parikh indicated no relevant financial relationships.
Supritha Chintamaneni indicated no relevant financial relationships.
Hader Ismail indicated no relevant financial relationships.
Aarohi Parikh, MD1, Supritha Chintamaneni, MBBS2, Hader Ismail, MD3. P1963 - Superior Mesenteric Artery Syndrome Masquerading as Cannabinoid Hyperemesis: A Case of Diagnostic Delay, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
