Sunday Poster Session
Category: Small Intestine
P1958 - The Hidden Culprit: Duodenal Lipoma Presenting as Chronic Abdominal Pain in a Young Adult
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Neal K. Bhachawat, DO
Houston Methodist Hospital
Houston, TX
Presenting Author(s)
Neal K. Bhachawat, DO1, Scott N. Berger, MD1, Neha Mathur, MD2, Sunil Dacha, MD1
1Houston Methodist Hospital, Houston, TX; 2Houston Methodist Hospital, Division of Gastroenterology and Hepatology, Lynda K. and David M. Underwood Center for Digestive Health, Houston, TX
Introduction: Intestinal lipomas are uncommon benign tumors with an unknown etiology and an estimated incidence between 0.15% and 4.4%. Large lipomas can lead to complications such as intussusception or obstruction. We present a rare case of a young male with non-specific abdominal complaints found to have intestinal intussusception secondary to a duodenal lipoma.
Case Description/
Methods: A 34-year-old male with class 3 obesity presented with 7 months of worsening postprandial abdominal pain and fullness. He reported a 10-pound unintentional weight loss over 2 months and denied overt gastrointestinal bleeding. Exam revealed pale conjunctiva and a soft, non-tender abdomen. Laboratory workup was notable for microcytic anemia: hemoglobin 4.4 g/dL, MCV 68 fL, and ferritin 4 ng/mL. Complete metabolic panel including liver tests was unremarkable. He received four units of packed red blood cells with improvement in anemia. CT abdomen/pelvis showed a 10 cm lipomatous mass in the descending duodenum with upstream intussusception (Image1). Upper endoscopy revealed a duodenal mass originating in the bulb, causing intussusception (Image2). Superficial biopsies showed polypoid duodenal mucosa with foveolar metaplasia, ulceration/erosion, and granulation tissue. Tumor markers (CA 19-9, CEA, Chromogranin A) were normal. His hemoglobin remained stable and abdominal pain improved. Surgery team planned for outpatient lipoma resection, however he was lost to follow-up.
Discussion: Duodenal lipomas are rare and can present with vague and non-specific gastrointestinal symptoms, which can lead to delayed diagnosis until complications occur. A literature review of 59 reported cases noted that 39% of duodenal lipomas arose in the second portion of the duodenum, with peak incidence typically between the fifth and seventh decades of life. Diagnosis is often established via radiologic imaging, commonly detected incidentally during CT scans performed for non-specific abdominal complaints. Importantly, the mucosal surface of a lipoma may exhibit areas of ulceration or erosion that can cause anemia. Large symptomatic lipomas are treated with surgical or endoscopic resection, with endoscopic submucosal dissection. This case highlights the need to consider duodenal lipomas in small bowel intussusception and to recognize when surgical or endoscopic intervention is warranted to prevent future recurrences.
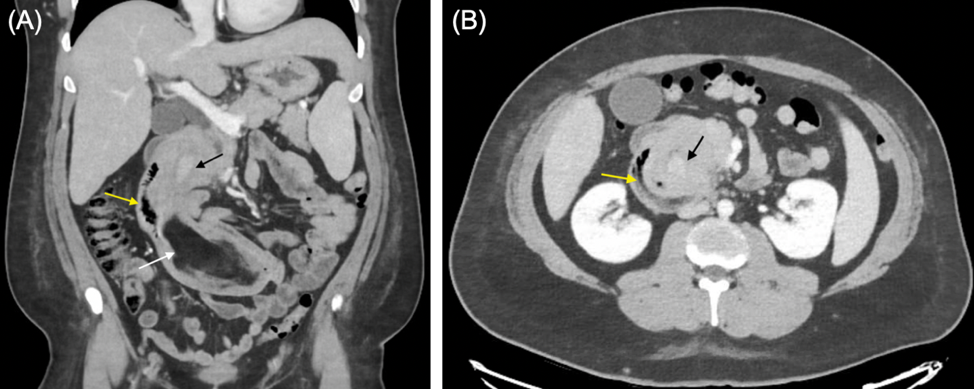
Figure: Compute Tomography (CT) scan with intravenous contrast: (A) coronal view shows intussusception of proximal bowel (black arrow) into the 2nd portion of duodenum (yellow arrow). A large duodenal lipoma is visualized in the area (white arrow). (B) axial view shows the intussusception of proximal bowel (black arrow) into the 2nd portion of duodenum (yellow arrow).
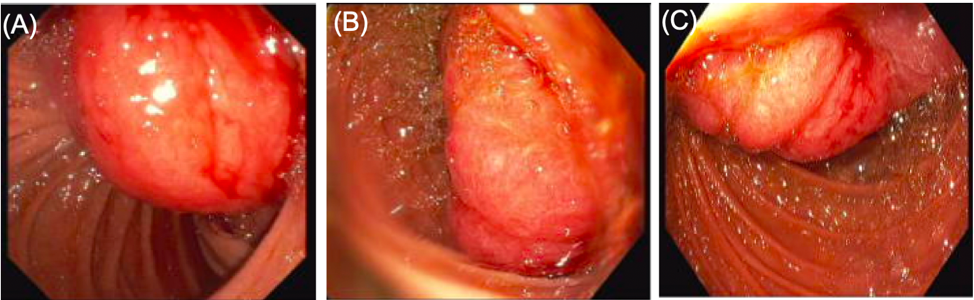
Figure: Endoscopy images showing a large mass originating at the duodenal bulb (A) and extends into the 2nd portion of the duodenum (B and C) causing intussusception.
Disclosures:
Neal Bhachawat indicated no relevant financial relationships.
Scott Berger indicated no relevant financial relationships.
Neha Mathur: Ardelyx – Speakers Bureau. Regeneron – Advisor or Review Panel Member, Speakers Bureau. Sanofi – Advisor or Review Panel Member, Speakers Bureau.
Sunil Dacha indicated no relevant financial relationships.
Neal K. Bhachawat, DO1, Scott N. Berger, MD1, Neha Mathur, MD2, Sunil Dacha, MD1. P1958 - The Hidden Culprit: Duodenal Lipoma Presenting as Chronic Abdominal Pain in a Young Adult, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Houston Methodist Hospital, Houston, TX; 2Houston Methodist Hospital, Division of Gastroenterology and Hepatology, Lynda K. and David M. Underwood Center for Digestive Health, Houston, TX
Introduction: Intestinal lipomas are uncommon benign tumors with an unknown etiology and an estimated incidence between 0.15% and 4.4%. Large lipomas can lead to complications such as intussusception or obstruction. We present a rare case of a young male with non-specific abdominal complaints found to have intestinal intussusception secondary to a duodenal lipoma.
Case Description/
Methods: A 34-year-old male with class 3 obesity presented with 7 months of worsening postprandial abdominal pain and fullness. He reported a 10-pound unintentional weight loss over 2 months and denied overt gastrointestinal bleeding. Exam revealed pale conjunctiva and a soft, non-tender abdomen. Laboratory workup was notable for microcytic anemia: hemoglobin 4.4 g/dL, MCV 68 fL, and ferritin 4 ng/mL. Complete metabolic panel including liver tests was unremarkable. He received four units of packed red blood cells with improvement in anemia. CT abdomen/pelvis showed a 10 cm lipomatous mass in the descending duodenum with upstream intussusception (Image1). Upper endoscopy revealed a duodenal mass originating in the bulb, causing intussusception (Image2). Superficial biopsies showed polypoid duodenal mucosa with foveolar metaplasia, ulceration/erosion, and granulation tissue. Tumor markers (CA 19-9, CEA, Chromogranin A) were normal. His hemoglobin remained stable and abdominal pain improved. Surgery team planned for outpatient lipoma resection, however he was lost to follow-up.
Discussion: Duodenal lipomas are rare and can present with vague and non-specific gastrointestinal symptoms, which can lead to delayed diagnosis until complications occur. A literature review of 59 reported cases noted that 39% of duodenal lipomas arose in the second portion of the duodenum, with peak incidence typically between the fifth and seventh decades of life. Diagnosis is often established via radiologic imaging, commonly detected incidentally during CT scans performed for non-specific abdominal complaints. Importantly, the mucosal surface of a lipoma may exhibit areas of ulceration or erosion that can cause anemia. Large symptomatic lipomas are treated with surgical or endoscopic resection, with endoscopic submucosal dissection. This case highlights the need to consider duodenal lipomas in small bowel intussusception and to recognize when surgical or endoscopic intervention is warranted to prevent future recurrences.
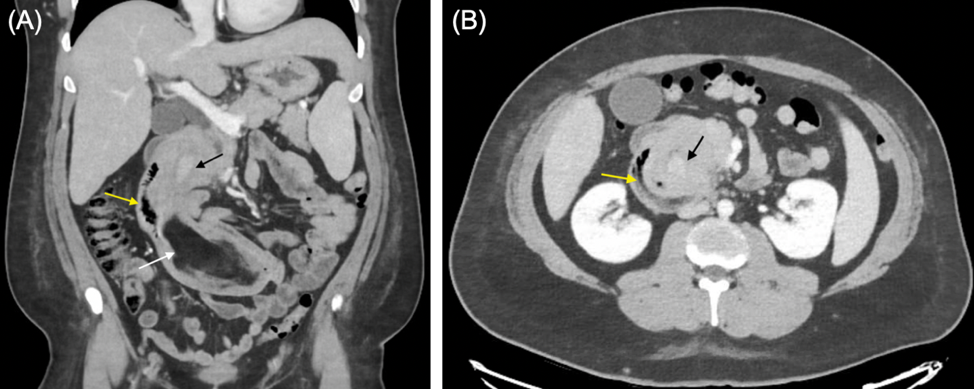
Figure: Compute Tomography (CT) scan with intravenous contrast: (A) coronal view shows intussusception of proximal bowel (black arrow) into the 2nd portion of duodenum (yellow arrow). A large duodenal lipoma is visualized in the area (white arrow). (B) axial view shows the intussusception of proximal bowel (black arrow) into the 2nd portion of duodenum (yellow arrow).
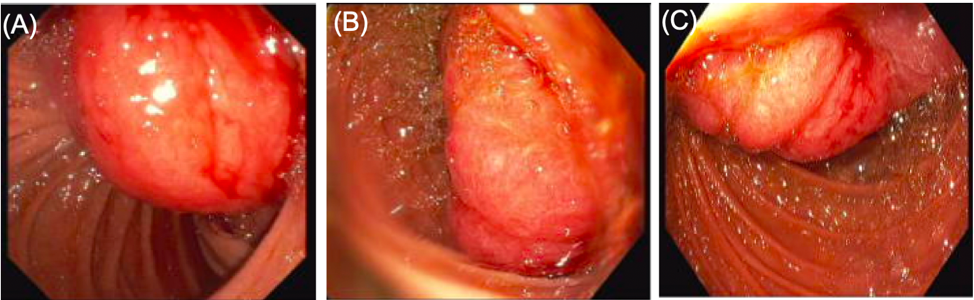
Figure: Endoscopy images showing a large mass originating at the duodenal bulb (A) and extends into the 2nd portion of the duodenum (B and C) causing intussusception.
Disclosures:
Neal Bhachawat indicated no relevant financial relationships.
Scott Berger indicated no relevant financial relationships.
Neha Mathur: Ardelyx – Speakers Bureau. Regeneron – Advisor or Review Panel Member, Speakers Bureau. Sanofi – Advisor or Review Panel Member, Speakers Bureau.
Sunil Dacha indicated no relevant financial relationships.
Neal K. Bhachawat, DO1, Scott N. Berger, MD1, Neha Mathur, MD2, Sunil Dacha, MD1. P1958 - The Hidden Culprit: Duodenal Lipoma Presenting as Chronic Abdominal Pain in a Young Adult, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
