Sunday Poster Session
Category: Practice Management
P1926 - Evaluating the Use of Sex in Gastroenterology Algorithms: A FAIRS Framework Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Oriana Pando, MD, MPH
Beth Israel Deaconess Medical Center
Boston, MA
Presenting Author(s)
Jordan Anders-Rumsey, MD1, Oriana Pando, MD, MPH2, Cass D. Condray, BSc3, Loren Rabinowitz, MD2, Kira Newman, MD, PhD1
1University of Michigan, Ann Arbor, MI; 2Beth Israel Deaconess Medical Center, Boston, MA; 3University of Oklahoma, Norman, OK
Introduction: Clinical algorithms are widely used in gastroenterology to guide decision-making and patient care. To ensure equitable and accurate outcomes, these tools must be evaluated for bias. A recent article in the New England Journal of Medicine introduced the FAIRS framework—Fairness Assessment In Representing Sex—for evaluating the inclusion of sex in clinical algorithms. It poses three key questions: (1) Is sex prognostically necessary? (2) Why is sex prognostically informative? (3) Would the algorithm’s anticipated use penalize the disadvantaged sex? We applied this framework to adult gastroenterology algorithms that explicitly incorporate sex as a variable.
Methods: A total of 184 algorithms were reviewed from sources including the ACG, AGA, AASLD, Rome Foundation, MDCalc, and UpToDate. Seven pediatric algorithms were excluded, leaving 177 adult-focused algorithms. Of these, 45 used sex-influenced variables (i.e. Hgb, Cr, BUN, AST, ALT, etc.), and 12 explicitly included sex as a variable and were included in analyses. Each algorithm was evaluated using the FAIRS framework by two independent reviewers.
Results: Among the 12 algorithms analyzed, 11 demonstrated appropriate use of sex, defined as an underlying sex based biologic difference affecting outcomes and no penalty (i.e. increased morbidity, mortality, complication, etc.) to the sex included in the algorithm. In these cases, sex was considered justifiably included. One algorithm (Obesity Surgery Mortality Risk Score) raised concerns, as sex appeared to influence outcomes without a clear biologic rationale and may disadvantage one sex—suggesting sex should be excluded or accompanied by a cautionary statement. Notably, two algorithms, the Model for End Stage Liver Disease score (MELD) 3.0 and Gender-Equity Model for liver Allocation (GEMA-Na), were found to reduce sex-based bias by adjusting scores for females, mitigating the negative impact of creatinine-based calculations in liver transplant allocation.
Discussion: The incorporation of sex in clinical algorithms within gastroenterology is complex and context dependent. While sex-based variables can enhance accuracy, they also carry the risk of perpetuating bias. The FAIRS framework provides a valuable tool for assessing the fairness of these algorithms. Further investigation is warranted into algorithms that use sex-correlated variables (e.g., Cr, Hgb), as these may introduce implicit bias even when sex is not explicitly included.
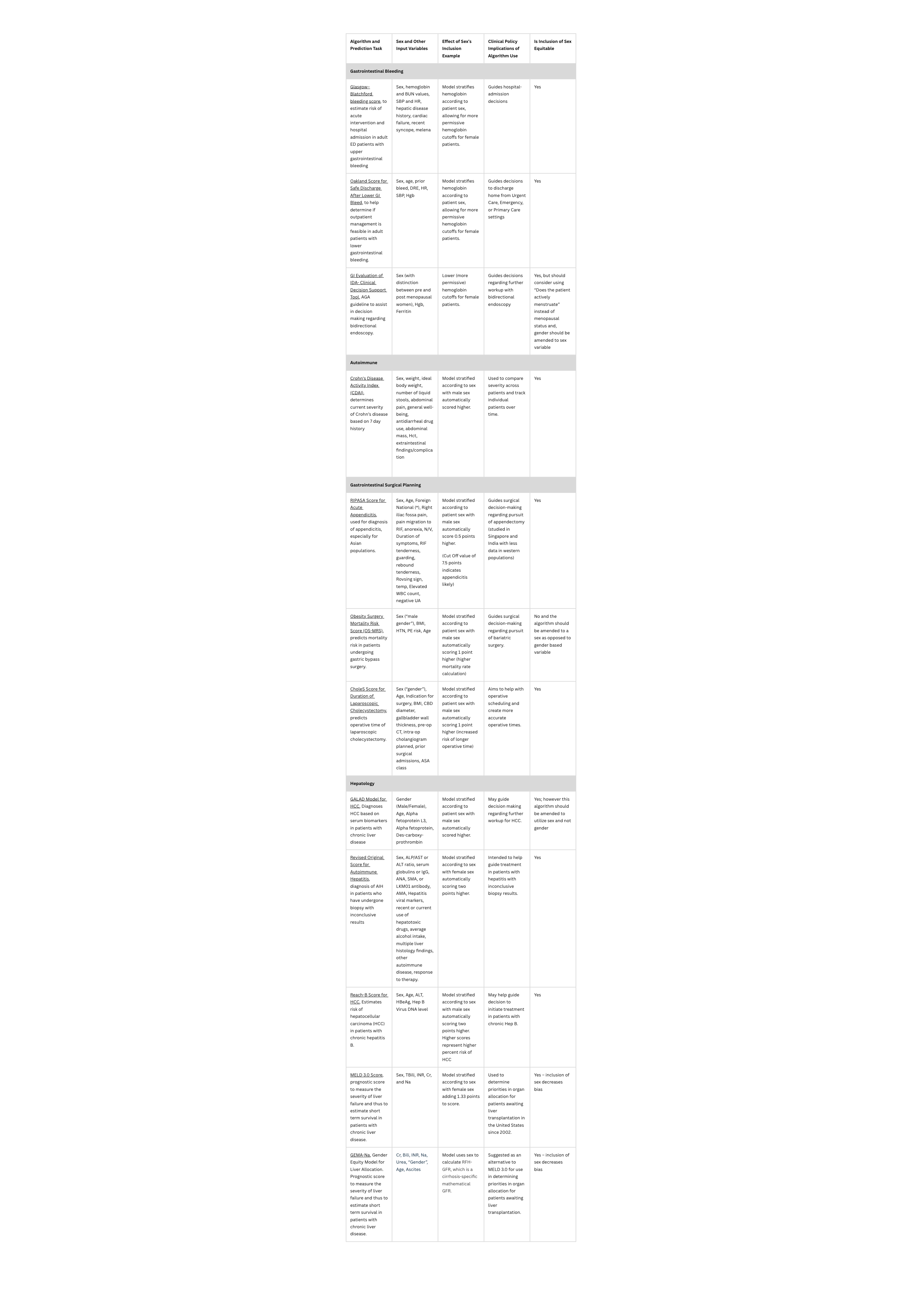
Figure: Figure 1: Twelve algorithms analyzed using FAIRS framework.
Disclosures:
Jordan Anders-Rumsey indicated no relevant financial relationships.
Oriana Pando indicated no relevant financial relationships.
Cass Condray indicated no relevant financial relationships.
Loren Rabinowitz indicated no relevant financial relationships.
Kira Newman indicated no relevant financial relationships.
Jordan Anders-Rumsey, MD1, Oriana Pando, MD, MPH2, Cass D. Condray, BSc3, Loren Rabinowitz, MD2, Kira Newman, MD, PhD1. P1926 - Evaluating the Use of Sex in Gastroenterology Algorithms: A FAIRS Framework Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Michigan, Ann Arbor, MI; 2Beth Israel Deaconess Medical Center, Boston, MA; 3University of Oklahoma, Norman, OK
Introduction: Clinical algorithms are widely used in gastroenterology to guide decision-making and patient care. To ensure equitable and accurate outcomes, these tools must be evaluated for bias. A recent article in the New England Journal of Medicine introduced the FAIRS framework—Fairness Assessment In Representing Sex—for evaluating the inclusion of sex in clinical algorithms. It poses three key questions: (1) Is sex prognostically necessary? (2) Why is sex prognostically informative? (3) Would the algorithm’s anticipated use penalize the disadvantaged sex? We applied this framework to adult gastroenterology algorithms that explicitly incorporate sex as a variable.
Methods: A total of 184 algorithms were reviewed from sources including the ACG, AGA, AASLD, Rome Foundation, MDCalc, and UpToDate. Seven pediatric algorithms were excluded, leaving 177 adult-focused algorithms. Of these, 45 used sex-influenced variables (i.e. Hgb, Cr, BUN, AST, ALT, etc.), and 12 explicitly included sex as a variable and were included in analyses. Each algorithm was evaluated using the FAIRS framework by two independent reviewers.
Results: Among the 12 algorithms analyzed, 11 demonstrated appropriate use of sex, defined as an underlying sex based biologic difference affecting outcomes and no penalty (i.e. increased morbidity, mortality, complication, etc.) to the sex included in the algorithm. In these cases, sex was considered justifiably included. One algorithm (Obesity Surgery Mortality Risk Score) raised concerns, as sex appeared to influence outcomes without a clear biologic rationale and may disadvantage one sex—suggesting sex should be excluded or accompanied by a cautionary statement. Notably, two algorithms, the Model for End Stage Liver Disease score (MELD) 3.0 and Gender-Equity Model for liver Allocation (GEMA-Na), were found to reduce sex-based bias by adjusting scores for females, mitigating the negative impact of creatinine-based calculations in liver transplant allocation.
Discussion: The incorporation of sex in clinical algorithms within gastroenterology is complex and context dependent. While sex-based variables can enhance accuracy, they also carry the risk of perpetuating bias. The FAIRS framework provides a valuable tool for assessing the fairness of these algorithms. Further investigation is warranted into algorithms that use sex-correlated variables (e.g., Cr, Hgb), as these may introduce implicit bias even when sex is not explicitly included.
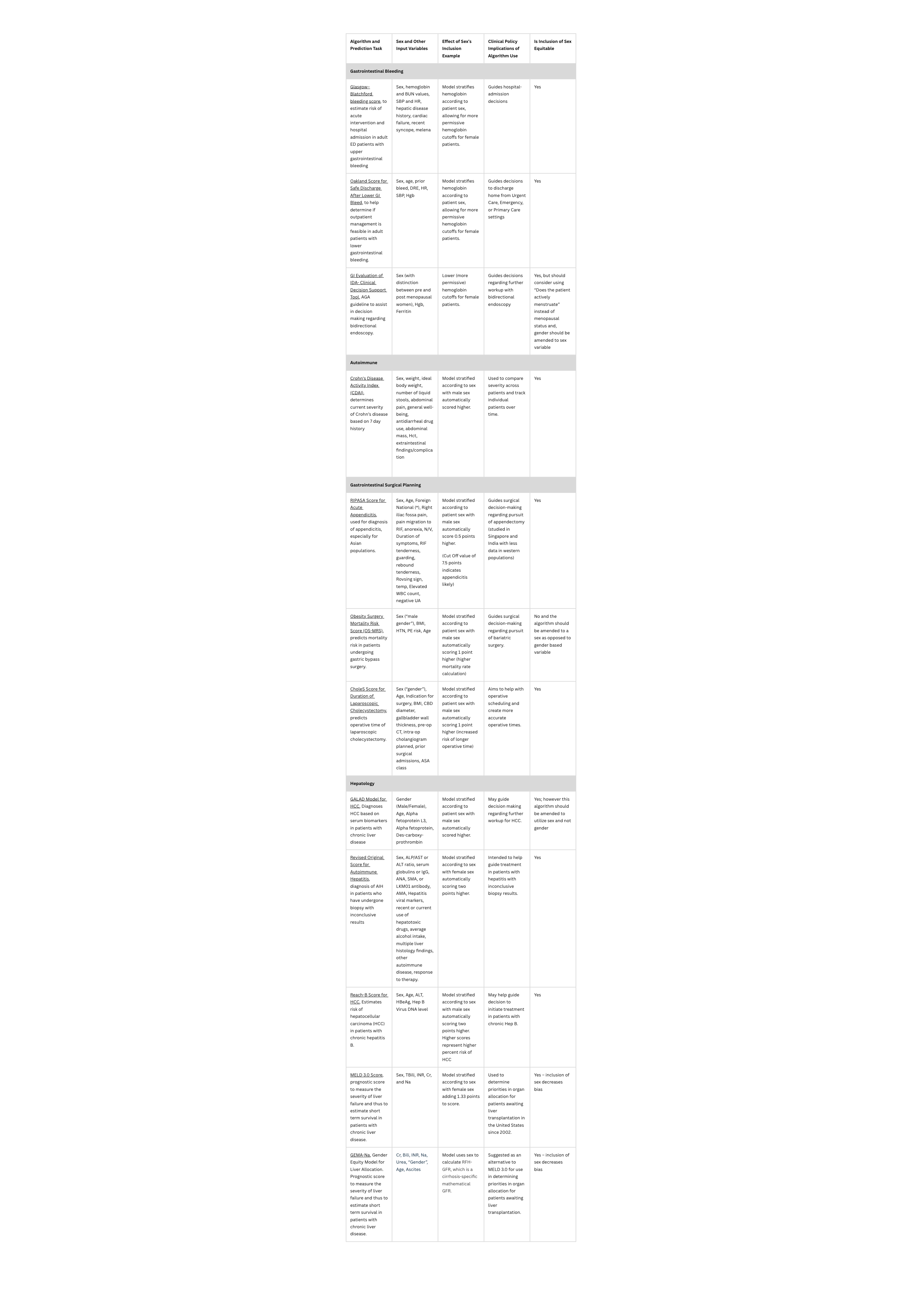
Figure: Figure 1: Twelve algorithms analyzed using FAIRS framework.
Disclosures:
Jordan Anders-Rumsey indicated no relevant financial relationships.
Oriana Pando indicated no relevant financial relationships.
Cass Condray indicated no relevant financial relationships.
Loren Rabinowitz indicated no relevant financial relationships.
Kira Newman indicated no relevant financial relationships.
Jordan Anders-Rumsey, MD1, Oriana Pando, MD, MPH2, Cass D. Condray, BSc3, Loren Rabinowitz, MD2, Kira Newman, MD, PhD1. P1926 - Evaluating the Use of Sex in Gastroenterology Algorithms: A FAIRS Framework Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

