Sunday Poster Session
Category: Practice Management
P1916 - Telehealth No-Shows in Digestive Health: The Role of Social Determinants of Health and Broadband Access
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Himesh Zaver, MD
University of Virginia Health
Charlottesville, VA
Presenting Author(s)
Himesh Zaver, MD1, Olivia Reszczynski, MD1, Aditya Singh, BS1, Tsola Efejuku, MD1, Robert Cutler, MD2, Alexander Podboy, MD1
1University of Virginia Health, Charlottesville, VA; 2Atrium Health Wake Forest Baptist, Winston-Salem, NC
Introduction: Telehealth is integral to modern healthcare delivery, yet barriers persist that impact equitable access and utilization. This study evaluated the relationship between patient demographics, broadband access, and social determinants of health (SDOH) in relation to telehealth appointment attendance among digestive health patients.
Methods: A total of 1,356 adults scheduled for digestive health telehealth visits at a tertiary-care center in central Virginia were categorized into either No-Show (n = 662) or Completed Visit (n = 694) cohorts. Patient-level data were extracted from the electronic health record (Table 1), while county-level data and broadband metrics, based on a patient’s home address, were obtained from the Federal Communications Commission’s “Mapping Broadband Health in America platform" (Table 2).
Results: No Show cohort patients were significantly younger (48.4 vs. 60.1 years; p < 0.001) and more often single (33.1% vs. 21.7%; p < 0.001). A higher proportion of No-Show encounters were scheduled in the IBD clinic (42.9% vs. 18.9%; p < 0.001), whereas appointments in General GI (11.6% vs. 20.1%; p < 0.001), Hepatology (14.4% vs. 32.3%; p < 0.001), and Liver Transplant clinics (8.6% vs. 17.4%; p < 0.001) were more likely to be completed. Completed visits were more likely among White/Caucasian patients (87.7% vs. 79.5%; p < 0.001), Medicare beneficiaries (53.2% vs. 30.5%; p < 0.001), and those who were married (52.8% vs. 44.1%; p = 0.002) or widowed (7.7% vs. 4.8%; p = 0.042). In contrast, the No Show cohort had higher proportions of Black (13.4% vs. 8.2%; p = 0.0027), Hispanic/Latino (4.1% vs. 1.9%; p = 0.026), single (33.1% vs. 21.7%; p < 0.001), and Medicaid-insured patients (26.4% vs. 18.4%; p < 0.001). Patients who were new to the tertiary care center (3.17% vs. 0.43%; p < 0.001) or attending an initial specialty visit in digestive health (7.55% vs. 2.44%; p < 0.001) were significantly more likely to miss their appointments. There were no significant differences in county-level broadband access, educational attainment, median household income, or unemployment rates between the two cohorts.
Discussion: Telehealth no-shows were associated with initial patient encounters, younger age, minority race/ethnicity, and Medicaid insurance. Future research is warranted to explore targeted interventions that address these disparities and optimize telehealth utilization across diverse patient populations.
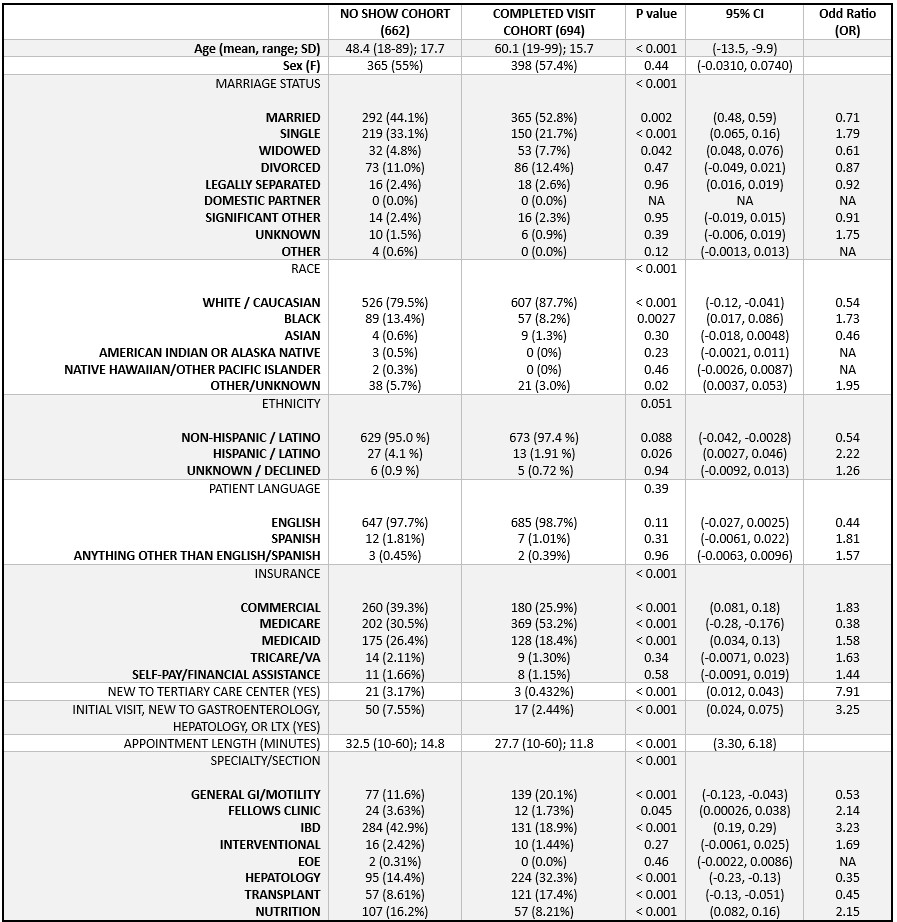
Figure: Table 1. Patient level subject demographics
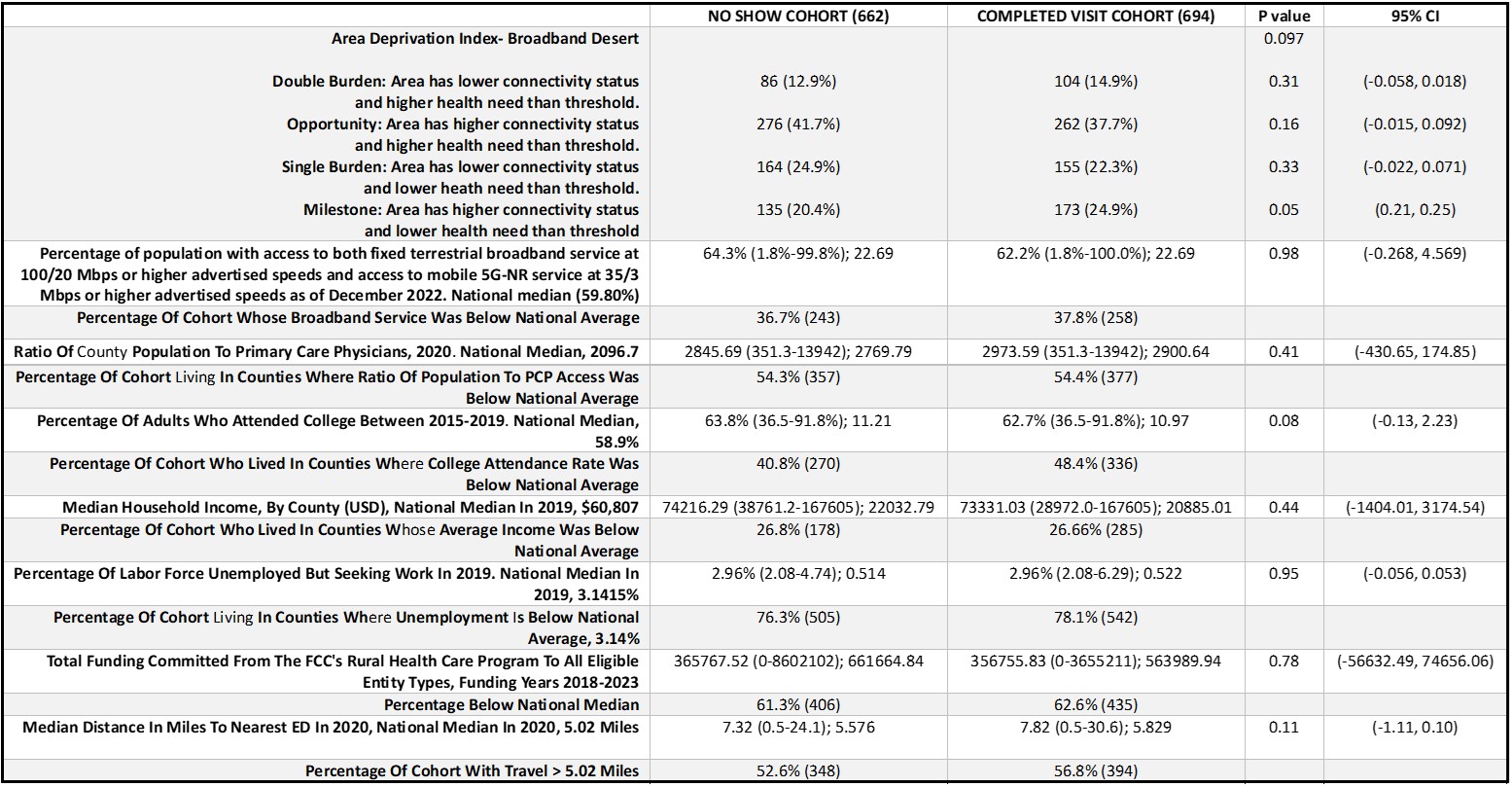
Figure: Table 2. County-level demographics derived from the Federal Communications Commission’s "Mapping Broadband Health in America" platform, a visual database integrating broadband and health-related data.
Disclosures:
Himesh Zaver indicated no relevant financial relationships.
Olivia Reszczynski indicated no relevant financial relationships.
Aditya Singh indicated no relevant financial relationships.
Tsola Efejuku indicated no relevant financial relationships.
Robert Cutler indicated no relevant financial relationships.
Alexander Podboy indicated no relevant financial relationships.
Himesh Zaver, MD1, Olivia Reszczynski, MD1, Aditya Singh, BS1, Tsola Efejuku, MD1, Robert Cutler, MD2, Alexander Podboy, MD1. P1916 - Telehealth No-Shows in Digestive Health: The Role of Social Determinants of Health and Broadband Access, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Virginia Health, Charlottesville, VA; 2Atrium Health Wake Forest Baptist, Winston-Salem, NC
Introduction: Telehealth is integral to modern healthcare delivery, yet barriers persist that impact equitable access and utilization. This study evaluated the relationship between patient demographics, broadband access, and social determinants of health (SDOH) in relation to telehealth appointment attendance among digestive health patients.
Methods: A total of 1,356 adults scheduled for digestive health telehealth visits at a tertiary-care center in central Virginia were categorized into either No-Show (n = 662) or Completed Visit (n = 694) cohorts. Patient-level data were extracted from the electronic health record (Table 1), while county-level data and broadband metrics, based on a patient’s home address, were obtained from the Federal Communications Commission’s “Mapping Broadband Health in America platform" (Table 2).
Results: No Show cohort patients were significantly younger (48.4 vs. 60.1 years; p < 0.001) and more often single (33.1% vs. 21.7%; p < 0.001). A higher proportion of No-Show encounters were scheduled in the IBD clinic (42.9% vs. 18.9%; p < 0.001), whereas appointments in General GI (11.6% vs. 20.1%; p < 0.001), Hepatology (14.4% vs. 32.3%; p < 0.001), and Liver Transplant clinics (8.6% vs. 17.4%; p < 0.001) were more likely to be completed. Completed visits were more likely among White/Caucasian patients (87.7% vs. 79.5%; p < 0.001), Medicare beneficiaries (53.2% vs. 30.5%; p < 0.001), and those who were married (52.8% vs. 44.1%; p = 0.002) or widowed (7.7% vs. 4.8%; p = 0.042). In contrast, the No Show cohort had higher proportions of Black (13.4% vs. 8.2%; p = 0.0027), Hispanic/Latino (4.1% vs. 1.9%; p = 0.026), single (33.1% vs. 21.7%; p < 0.001), and Medicaid-insured patients (26.4% vs. 18.4%; p < 0.001). Patients who were new to the tertiary care center (3.17% vs. 0.43%; p < 0.001) or attending an initial specialty visit in digestive health (7.55% vs. 2.44%; p < 0.001) were significantly more likely to miss their appointments. There were no significant differences in county-level broadband access, educational attainment, median household income, or unemployment rates between the two cohorts.
Discussion: Telehealth no-shows were associated with initial patient encounters, younger age, minority race/ethnicity, and Medicaid insurance. Future research is warranted to explore targeted interventions that address these disparities and optimize telehealth utilization across diverse patient populations.
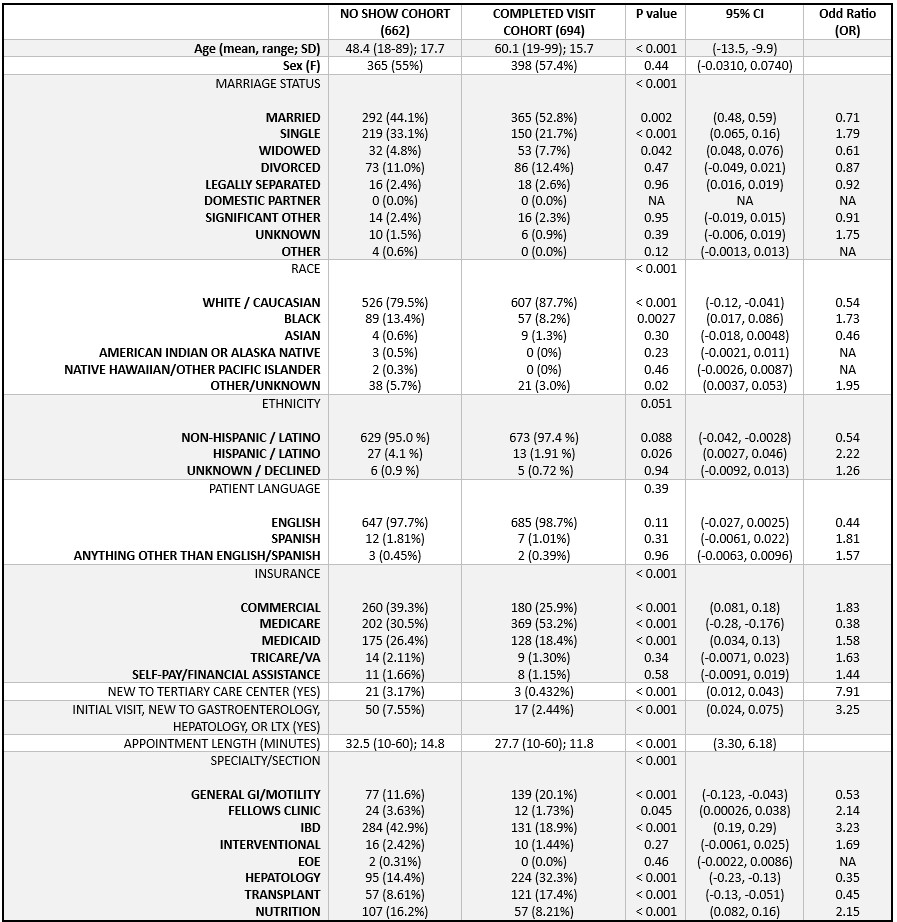
Figure: Table 1. Patient level subject demographics
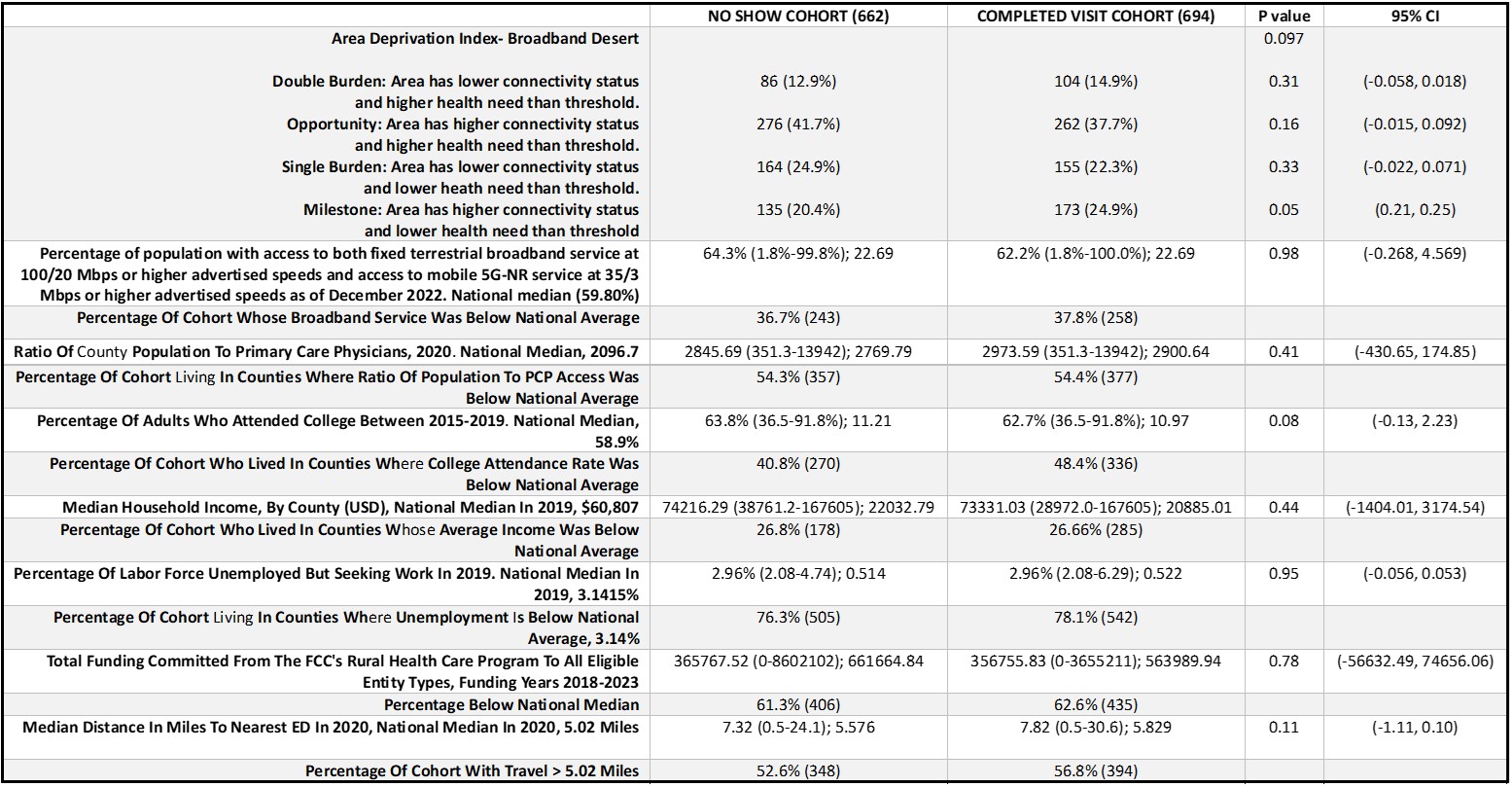
Figure: Table 2. County-level demographics derived from the Federal Communications Commission’s "Mapping Broadband Health in America" platform, a visual database integrating broadband and health-related data.
Disclosures:
Himesh Zaver indicated no relevant financial relationships.
Olivia Reszczynski indicated no relevant financial relationships.
Aditya Singh indicated no relevant financial relationships.
Tsola Efejuku indicated no relevant financial relationships.
Robert Cutler indicated no relevant financial relationships.
Alexander Podboy indicated no relevant financial relationships.
Himesh Zaver, MD1, Olivia Reszczynski, MD1, Aditya Singh, BS1, Tsola Efejuku, MD1, Robert Cutler, MD2, Alexander Podboy, MD1. P1916 - Telehealth No-Shows in Digestive Health: The Role of Social Determinants of Health and Broadband Access, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

