Sunday Poster Session
Category: Pediatrics
P1902 - Sulfasalazine-Induced Esophagitis Dissecans Superficialis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- KP
Kalyan Ray Parashette, MD, MPH
Loma Linda University Children's Hospital
Redlands, CA
Presenting Author(s)
Award: ACG Presidential Poster Award
Kalyan Ray Parashette, MD, MPH
Loma Linda University Children's Hospital, Redlands, CA
Introduction: Esophagitis dissecans superficialis (EDS) is a rare, begin, and self-limited condition. We present a case of sulfasalazine induced EDS, which resolved following the discontinuation of sulfasalazine.
Case Description/
Methods: A 13-year-old boy was diagnosed with pan-ulcerative colitis at 9 years of age. He had been maintained on sulfasalazine for the past 4 years. Clinically, his ulcerative colitis remained in remission. Blood work, including inflammatory markers were normal. Stool hemoccult was negative. However, fecal calprotectin was elevated at 109 µg/g (normal < 50 µg/g). Colonoscopy findings were normal. However, upper endoscopy revealed sloughing of the esophageal mucosa. Biopsies demonstrated viable squamous mucosa with mild chronic (lymphocyte-predominant) esophagitis and admixed detached, degenerated squamous epithelium, without significant associated inflammation. These findings were consistent with EDS. No fungal organisms were identified on PAS stain. EDS was suspected to be related to sulfasalazine therapy. Sulfasalazine was discontinued and replaced with mesalamine. Six weeks later, a follow-up transnasal endoscopy revealed a normal esophagus, indicating resolution of EDS following the change in therapy.
Discussion: Esophagitis dissecans superficialis (EDS), also known as sloughing esophagitis, is a rare condition characterized by sloughing of the esophageal epithelium. It is most commonly associated with desquamative dermatologic disorders, autoimmune disease, and medications. The exact etiology remains unclear, but proposed mechanisms include immune-mediated, physical, chemical, and thermal injury. EDS is often diagnosed incidentally, as in our case. When symptomatic, patients may present with dysphagia, odynophagia, vomiting, or heartburn. Endoscopic findings typically include whitish strips of easily detachable mucosa, most often involving the mid to distal esophagus. Biopsies usually reveal detached superficial squamous epithelium with mild inflammation. Treatment primarily involves identifying and removing the underlying trigger. In our case, the condition resolved completely following a change in therapy from sulfasalazine to mesalamine. Additional therapies may include proton pump inhibitors and, in autoimmune-related cases, systemic corticosteroids. The prognosis is generally excellent, with minimal long-term complications.
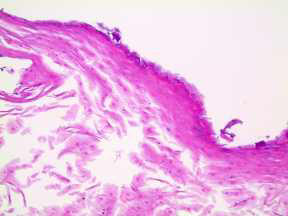
Figure: Upper endoscopy shows sloughing of the esophageal mucosa
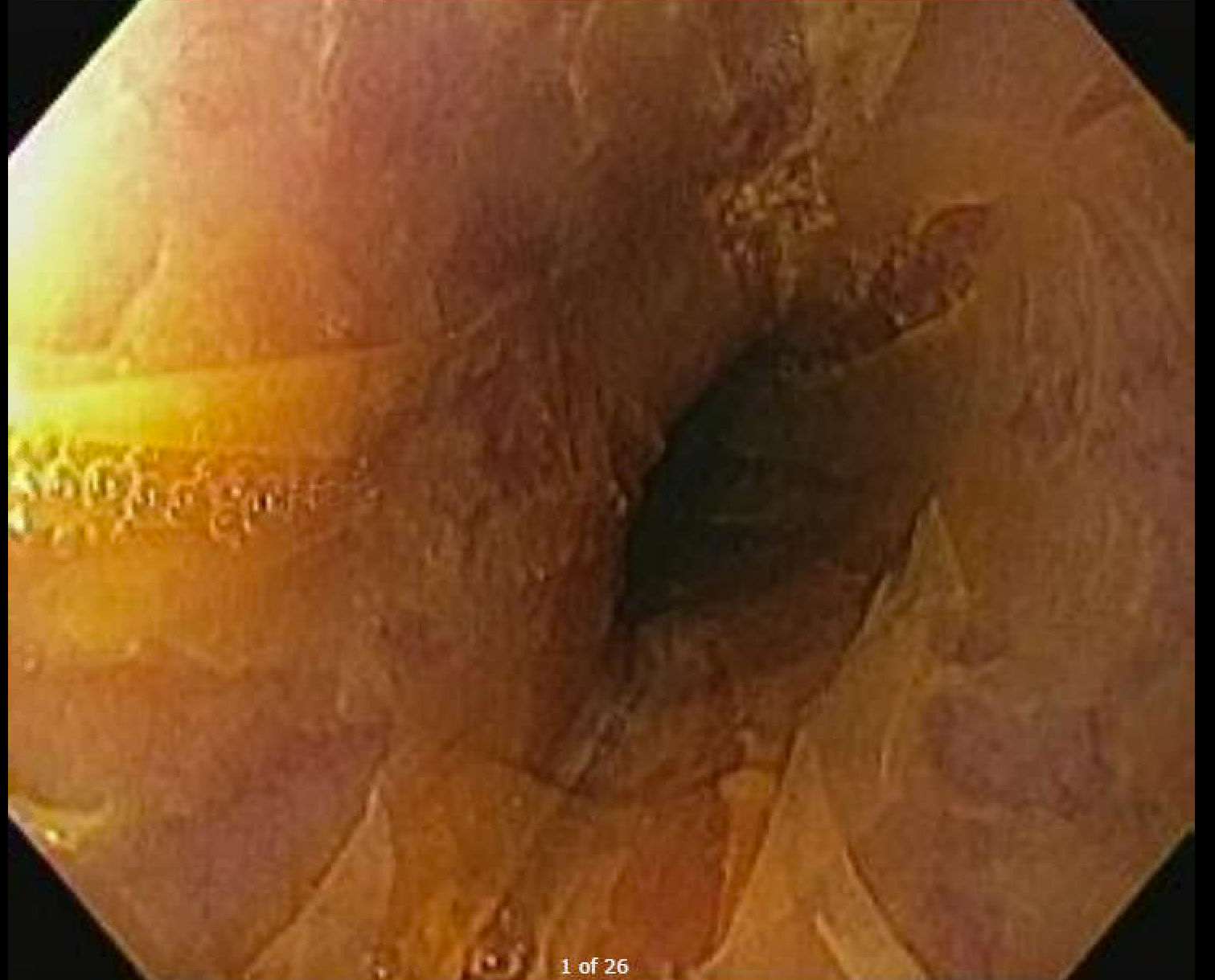
Figure: Biopsies shows viable squamous mucosa with mild chronic (lymphocytic-predominant) esophagitis and admixed detached degenerated squamous epithelium, without significant associated inflammation.
Disclosures:
Kalyan Ray Parashette indicated no relevant financial relationships.
Kalyan Ray Parashette, MD, MPH. P1902 - Sulfasalazine-Induced Esophagitis Dissecans Superficialis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Kalyan Ray Parashette, MD, MPH
Loma Linda University Children's Hospital, Redlands, CA
Introduction: Esophagitis dissecans superficialis (EDS) is a rare, begin, and self-limited condition. We present a case of sulfasalazine induced EDS, which resolved following the discontinuation of sulfasalazine.
Case Description/
Methods: A 13-year-old boy was diagnosed with pan-ulcerative colitis at 9 years of age. He had been maintained on sulfasalazine for the past 4 years. Clinically, his ulcerative colitis remained in remission. Blood work, including inflammatory markers were normal. Stool hemoccult was negative. However, fecal calprotectin was elevated at 109 µg/g (normal < 50 µg/g). Colonoscopy findings were normal. However, upper endoscopy revealed sloughing of the esophageal mucosa. Biopsies demonstrated viable squamous mucosa with mild chronic (lymphocyte-predominant) esophagitis and admixed detached, degenerated squamous epithelium, without significant associated inflammation. These findings were consistent with EDS. No fungal organisms were identified on PAS stain. EDS was suspected to be related to sulfasalazine therapy. Sulfasalazine was discontinued and replaced with mesalamine. Six weeks later, a follow-up transnasal endoscopy revealed a normal esophagus, indicating resolution of EDS following the change in therapy.
Discussion: Esophagitis dissecans superficialis (EDS), also known as sloughing esophagitis, is a rare condition characterized by sloughing of the esophageal epithelium. It is most commonly associated with desquamative dermatologic disorders, autoimmune disease, and medications. The exact etiology remains unclear, but proposed mechanisms include immune-mediated, physical, chemical, and thermal injury. EDS is often diagnosed incidentally, as in our case. When symptomatic, patients may present with dysphagia, odynophagia, vomiting, or heartburn. Endoscopic findings typically include whitish strips of easily detachable mucosa, most often involving the mid to distal esophagus. Biopsies usually reveal detached superficial squamous epithelium with mild inflammation. Treatment primarily involves identifying and removing the underlying trigger. In our case, the condition resolved completely following a change in therapy from sulfasalazine to mesalamine. Additional therapies may include proton pump inhibitors and, in autoimmune-related cases, systemic corticosteroids. The prognosis is generally excellent, with minimal long-term complications.
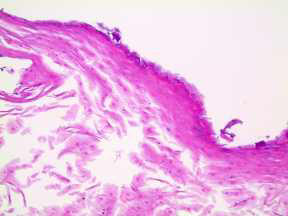
Figure: Upper endoscopy shows sloughing of the esophageal mucosa
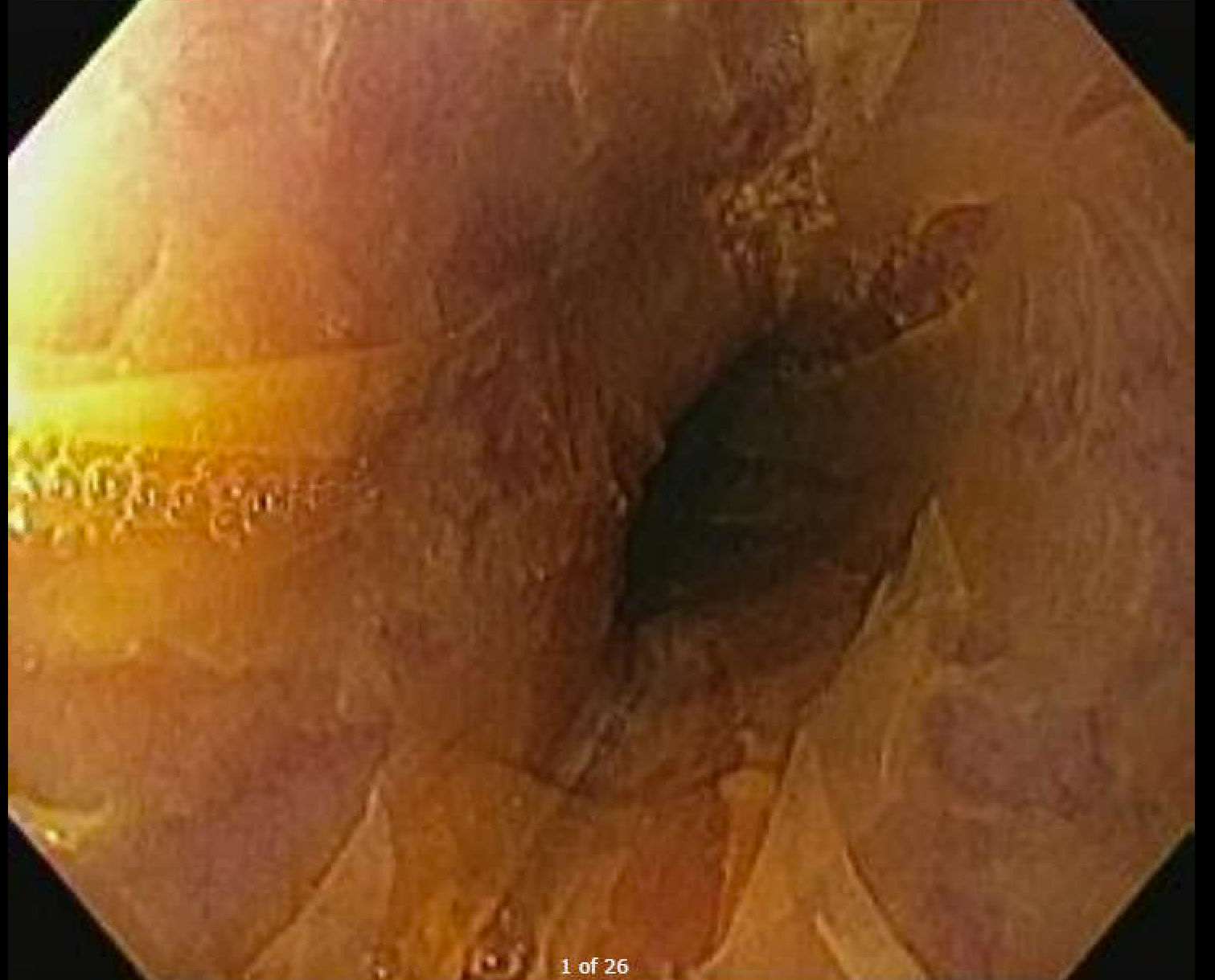
Figure: Biopsies shows viable squamous mucosa with mild chronic (lymphocytic-predominant) esophagitis and admixed detached degenerated squamous epithelium, without significant associated inflammation.
Disclosures:
Kalyan Ray Parashette indicated no relevant financial relationships.
Kalyan Ray Parashette, MD, MPH. P1902 - Sulfasalazine-Induced Esophagitis Dissecans Superficialis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

