Sunday Poster Session
Category: Pediatrics
P1901 - Unrelenting Bleeding in a Teen: An Atypical Debut of Crohn’s Disease
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Sean O. MacBride, MBA, BS
University of Nebraska Medical Center
Omaha, NE
Presenting Author(s)
Sean O. MacBride, MBA, BS, Alvaro Flores, MD
University of Nebraska Medical Center, Omaha, NE
Introduction: Crohn’s disease is a chronic, immune-mediated inflammatory condition that can affect the gastrointestinal tract from mouth to anus. While abdominal pain, weight loss, and diarrhea are hallmark features, significant gastrointestinal hemorrhage is rare. We present an unusual case of Crohn’s disease in an adolescent with severe, recurrent hematochezia with poorly localizable bleeding.
Case Description/
Methods: A previously healthy 17-year-old male presented with sudden-onset, painless hematochezia without accompanying symptoms. Initial evaluation revealed fecal calprotectin at 731.20 µg/g, normal coagulation studies, and a negative gastrointestinal pathogen panel; Meckel’s scan was unremarkable.
Within 24 hours of admission, he had over 15 grossly bloody bowel movements. Hemoglobin fell precipitously from 13.5 g/dL to 9.3 g/dL. CT revealed bowel wall thickening of the terminal ileum. Despite signs of active hemorrhage, panendoscopy revealed no bleeding source, however, colonoscopy showed mucosal thickening and cobble stoning consistent with Crohn’s ileitis (Fig A).
Intravenous steroids resulted in interval improvements in stool frequency and hematochezia. MRE showed terminal ileitis with a localized stricture. Despite clinical improvement, hemoglobin fell to 6.6 g/dL, requiring two blood transfusions. CTA failed to identify active bleeding. Repeat colonoscopy identified areas of oozing in the terminal ileum (Fig B). Given the lack of localized lesions amenable for conventional bleeding control interventions, we treated with Polysaccharide Hemostatic System and Hemostatic gel (Fig C). Bleeding resolved and hemoglobin stabilized.
Discussion: Although gastrointestinal bleeding occurs in Crohn’s disease, it is typically accompanied by hallmark symptoms such as abdominal pain, diarrhea, or weight loss; severe bleeding is a rare initial presentation. In this case, the absence of typical symptoms and the severity of bleeding posed a diagnostic and therapeutic challenge. Despite multiple imaging studies and endoscopic evaluations, localizing the bleeding source was initially unsuccessful. Once the source was finally identified, therapeutic endoscopic interventions were limited due to lack of localized bleeding amenable to standard bleeding control methods leading salvage therapy with second line hemostatic agents. This highlights the difficulty of managing atypical presentations of Crohn’s disease and the importance of maintaining a broad differential in evaluating acute hematochezia in adolescents.
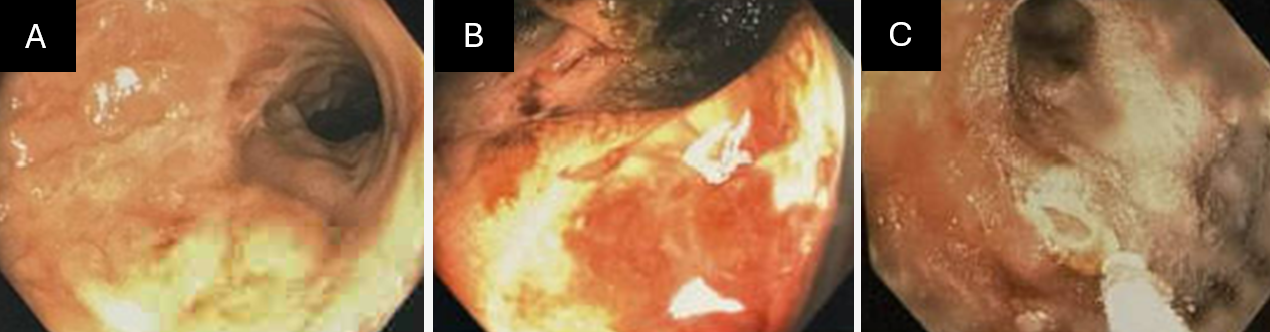
Figure: Fig A. Terminal ileum with inflamed mucosa but no stigmata of recent bleeding on initial colonoscopy. Fig B. Terminal ileum with inflamed mucosa and active oozing on repeat colonoscopy. Fig C. Terminal ileum following application of hemostatic gel.
Disclosures:
Sean MacBride indicated no relevant financial relationships.
Alvaro Flores indicated no relevant financial relationships.
Sean O. MacBride, MBA, BS, Alvaro Flores, MD. P1901 - Unrelenting Bleeding in a Teen: An Atypical Debut of Crohn’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Nebraska Medical Center, Omaha, NE
Introduction: Crohn’s disease is a chronic, immune-mediated inflammatory condition that can affect the gastrointestinal tract from mouth to anus. While abdominal pain, weight loss, and diarrhea are hallmark features, significant gastrointestinal hemorrhage is rare. We present an unusual case of Crohn’s disease in an adolescent with severe, recurrent hematochezia with poorly localizable bleeding.
Case Description/
Methods: A previously healthy 17-year-old male presented with sudden-onset, painless hematochezia without accompanying symptoms. Initial evaluation revealed fecal calprotectin at 731.20 µg/g, normal coagulation studies, and a negative gastrointestinal pathogen panel; Meckel’s scan was unremarkable.
Within 24 hours of admission, he had over 15 grossly bloody bowel movements. Hemoglobin fell precipitously from 13.5 g/dL to 9.3 g/dL. CT revealed bowel wall thickening of the terminal ileum. Despite signs of active hemorrhage, panendoscopy revealed no bleeding source, however, colonoscopy showed mucosal thickening and cobble stoning consistent with Crohn’s ileitis (Fig A).
Intravenous steroids resulted in interval improvements in stool frequency and hematochezia. MRE showed terminal ileitis with a localized stricture. Despite clinical improvement, hemoglobin fell to 6.6 g/dL, requiring two blood transfusions. CTA failed to identify active bleeding. Repeat colonoscopy identified areas of oozing in the terminal ileum (Fig B). Given the lack of localized lesions amenable for conventional bleeding control interventions, we treated with Polysaccharide Hemostatic System and Hemostatic gel (Fig C). Bleeding resolved and hemoglobin stabilized.
Discussion: Although gastrointestinal bleeding occurs in Crohn’s disease, it is typically accompanied by hallmark symptoms such as abdominal pain, diarrhea, or weight loss; severe bleeding is a rare initial presentation. In this case, the absence of typical symptoms and the severity of bleeding posed a diagnostic and therapeutic challenge. Despite multiple imaging studies and endoscopic evaluations, localizing the bleeding source was initially unsuccessful. Once the source was finally identified, therapeutic endoscopic interventions were limited due to lack of localized bleeding amenable to standard bleeding control methods leading salvage therapy with second line hemostatic agents. This highlights the difficulty of managing atypical presentations of Crohn’s disease and the importance of maintaining a broad differential in evaluating acute hematochezia in adolescents.
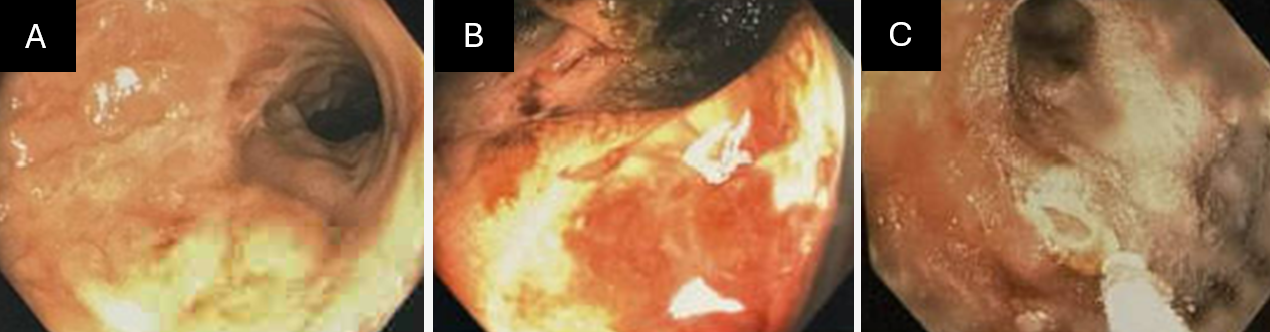
Figure: Fig A. Terminal ileum with inflamed mucosa but no stigmata of recent bleeding on initial colonoscopy. Fig B. Terminal ileum with inflamed mucosa and active oozing on repeat colonoscopy. Fig C. Terminal ileum following application of hemostatic gel.
Disclosures:
Sean MacBride indicated no relevant financial relationships.
Alvaro Flores indicated no relevant financial relationships.
Sean O. MacBride, MBA, BS, Alvaro Flores, MD. P1901 - Unrelenting Bleeding in a Teen: An Atypical Debut of Crohn’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
