Sunday Poster Session
Category: Liver
P1874 - Perplexing Severe Cholestasis in the Post-Partum Period
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- SY
Sarah F. Yosief, MD (she/her/hers)
Duke University Hospital
Durham, NC
Presenting Author(s)
Sarah F. Yosief, MD1, Kara Wegermann, MD2
1Duke University Hospital, Durham, NC; 2Duke University School of Medicine, Durham, NC
Introduction: Primary sclerosing cholangitis (PSC) is a chronic cholestatic liver disease with progressive bile duct inflammation and fibrosis. This case highlights the challenge of diagnosing PSC during pregnancy and postpartum due to overlap with intrahepatic cholestasis of pregnancy (ICP), gallbladder disease, and drug-induced liver injury (DILI).
Case Description/
Methods: A 36-year-old G2P0010 woman with a history of H. pylori gastritis, ICP, and gallstone pancreatitis during her second trimester presented four days postpartum with RUQ pain, jaundice, nausea, and vomiting. Labs showed AST 184 U/L, ALT 96 U/L, bilirubin 8.6 mg/dL, and ALP 936 U/L. MRI revealed a decompressed gallbladder with sludge, no ductal dilation, and increased hepatic T1 signal. ANA was low-positive (1:160). Cephalexin-induced DILI was suspected.
Her liver tests worsened despite observation. EUS was unremarkable, and liver biopsy showed patchy canalicular cholestasis, lobular inflammation, and periportal fibrosis. She did not tolerate cholestyramine and her jaundice and pruritus worsened. Ursodiol improved transaminases and ALP, but not bilirubin; it was discontinued due to diarrhea.
Repeat MRI/MRCP showed peripheral ductal irregularities. A second liver biopsy showed severe lobular cholestasis, bile duct injury, and worsening fibrosis. ERCP confirmed multifocal intrahepatic strictures, consistent with PSC.
Discussion: This case shows how overlapping pregnancy-related conditions can complicate diagnosis of chronic liver disease. ICP was initially suspected, but the postpartum worsening was not consistent with the typical clinical course. Her recent antibiotic exposure suggested DILI. However, persistent lab abnormalities and progressive fibrosis off the offending agent made DILI unlikely. Hormonal changes in pregnancy may have masked or worsened PSC.
Retrospective review of the initial MRI revealed subtle hepatic T1 abnormalities suggestive of early cholestasis. Repeat imaging and biopsy later showed clear biliary injury, and ERCP ultimately confirmed PSC.
This case emphasizes the importance of serial assessment in evolving cholestatic disease, the diagnostic value of ERCP when noninvasive findings are inconclusive, and the need to consider both pregnancy-specific and unrelated liver diseases. In complex presentations, multidisciplinary collaboration is critical for timely and accurate diagnosis.
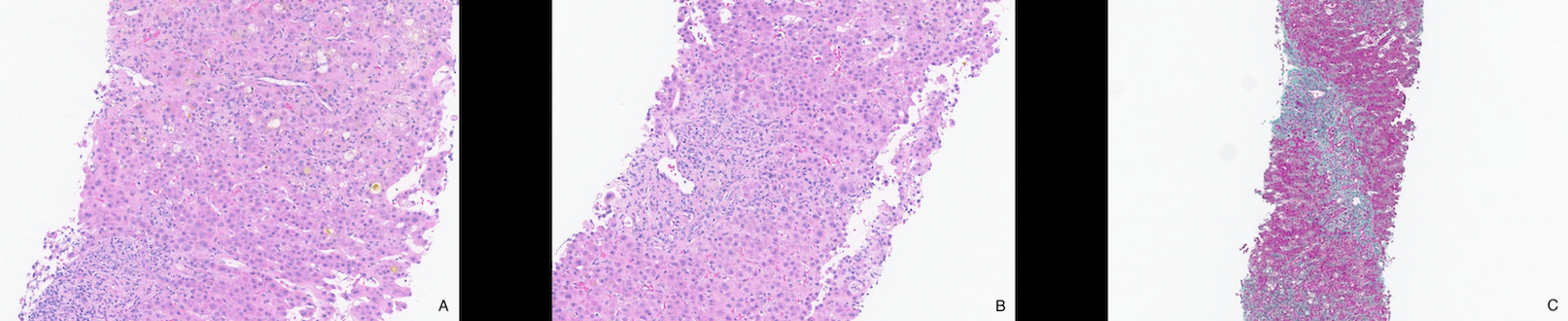
Figure: Figure 1: Liver Biopsy with Staining
A. Severe lobular cholestasis associated with marked lobular disarray, feathery degeneration, and focal hepatocyte dropout (HE 400x)
B. Mild portal inflammation associated with ductular reaction (HE 400x)
C. Periportal fibrosis with patchy perisinusoidal fibrosis on trichrome stain (trichrome 200x)
Disclosures:
Sarah Yosief indicated no relevant financial relationships.
Kara Wegermann: FocusMed CME – Speaker.
Sarah F. Yosief, MD1, Kara Wegermann, MD2. P1874 - Perplexing Severe Cholestasis in the Post-Partum Period, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Duke University Hospital, Durham, NC; 2Duke University School of Medicine, Durham, NC
Introduction: Primary sclerosing cholangitis (PSC) is a chronic cholestatic liver disease with progressive bile duct inflammation and fibrosis. This case highlights the challenge of diagnosing PSC during pregnancy and postpartum due to overlap with intrahepatic cholestasis of pregnancy (ICP), gallbladder disease, and drug-induced liver injury (DILI).
Case Description/
Methods: A 36-year-old G2P0010 woman with a history of H. pylori gastritis, ICP, and gallstone pancreatitis during her second trimester presented four days postpartum with RUQ pain, jaundice, nausea, and vomiting. Labs showed AST 184 U/L, ALT 96 U/L, bilirubin 8.6 mg/dL, and ALP 936 U/L. MRI revealed a decompressed gallbladder with sludge, no ductal dilation, and increased hepatic T1 signal. ANA was low-positive (1:160). Cephalexin-induced DILI was suspected.
Her liver tests worsened despite observation. EUS was unremarkable, and liver biopsy showed patchy canalicular cholestasis, lobular inflammation, and periportal fibrosis. She did not tolerate cholestyramine and her jaundice and pruritus worsened. Ursodiol improved transaminases and ALP, but not bilirubin; it was discontinued due to diarrhea.
Repeat MRI/MRCP showed peripheral ductal irregularities. A second liver biopsy showed severe lobular cholestasis, bile duct injury, and worsening fibrosis. ERCP confirmed multifocal intrahepatic strictures, consistent with PSC.
Discussion: This case shows how overlapping pregnancy-related conditions can complicate diagnosis of chronic liver disease. ICP was initially suspected, but the postpartum worsening was not consistent with the typical clinical course. Her recent antibiotic exposure suggested DILI. However, persistent lab abnormalities and progressive fibrosis off the offending agent made DILI unlikely. Hormonal changes in pregnancy may have masked or worsened PSC.
Retrospective review of the initial MRI revealed subtle hepatic T1 abnormalities suggestive of early cholestasis. Repeat imaging and biopsy later showed clear biliary injury, and ERCP ultimately confirmed PSC.
This case emphasizes the importance of serial assessment in evolving cholestatic disease, the diagnostic value of ERCP when noninvasive findings are inconclusive, and the need to consider both pregnancy-specific and unrelated liver diseases. In complex presentations, multidisciplinary collaboration is critical for timely and accurate diagnosis.
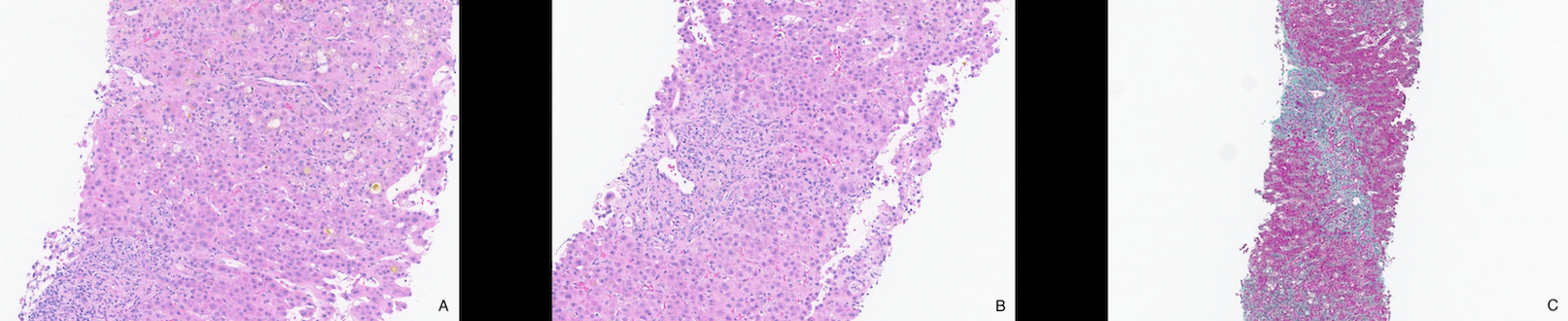
Figure: Figure 1: Liver Biopsy with Staining
A. Severe lobular cholestasis associated with marked lobular disarray, feathery degeneration, and focal hepatocyte dropout (HE 400x)
B. Mild portal inflammation associated with ductular reaction (HE 400x)
C. Periportal fibrosis with patchy perisinusoidal fibrosis on trichrome stain (trichrome 200x)
Disclosures:
Sarah Yosief indicated no relevant financial relationships.
Kara Wegermann: FocusMed CME – Speaker.
Sarah F. Yosief, MD1, Kara Wegermann, MD2. P1874 - Perplexing Severe Cholestasis in the Post-Partum Period, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
