Sunday Poster Session
Category: Liver
P1872 - An Unusual Case of Non-Cirrhotic Hyperammonemic Encephalopathy in an Adult Patient: Case Report and Literature Review
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Vishal Chandel, MD
Brigham and Women's Hospital, Harvard Medical School
Boston, MA
Presenting Author(s)
Vishal Chandel, MD
Brigham and Women's Hospital, Harvard Medical School, Boston, MA
Introduction: Hyperammonemia is the underlying metabolic derangement in decompensated liver disease. A less common presentation is hyperammonemia in the absence of liver disease. Infections by urease producing organisms and Urea cycle disorders (UCD) should be considered for unexplained hyperammonemia. We present a case of non-cirrhotic hyperammonemia (NCH) complicated by cerebral edema that failed conventional therapy.
Case Description/
Methods: A 45-year-old female with multiple sclerosis (on monoclonal antibody) presented with acute abdominal pain. Imaging revealed pneumoperitoneum from gastric perforation secondary to chronic steroid use. The course was further complicated by intraabdominal sepsis due to gastric leak. During treatment, patient developed progressively elevated ammonia levels of unclear etiology as the patient had no history of liver disease. The peak ammonia was 676 μmol/L (normal range 11–60). Labs and imaging did not demonstrate cirrhosis or acute liver failure. Ammonia remained elevated despite lactulose and continuous renal replacement therapy. Encephalopathy ensued with neurologic deterioration requiring intubation. The patient required parenteral nutrition (PN) due to gastric leak and recent wedge resection. Amino acids were removed from PN when the ammonia level was 326 μmol/L. The patient was found to have positive rare Ureaplasma species. Azithromycin, doxycycline and levofloxacin were started but patient continued to decline with progressive worsening of mental status eventually leading to cerebral edema, herniation and death.
Discussion: In our case, patient had NCH non-responsive to treatment. The mechanism is likely related to either having an undiagnosed inborn error of metabolism (IEM) or an infection with urea producing organism in the setting of severe immunocompromised status and post-surgical complications. In this patient, chronic steroid and immunomodulator use either unmasked IEMs or gave a flourishing medium for urease-producing organisms. Although IEMs often have early age of onset, UCDs can present at later age. Ornithine transcarbamylase deficiency is the most common UCD and can present with reduced plasma citrulline in both children and adults. Treating a potential IEM begins prior to confirmation of an etiology. Treatment should start early if UCD is suspected. Timely intervention is essential to prevent mortality. Early treatment includes holding proteins, providing ammonia scavengers along with renal replacement to reduce ammonia levels.
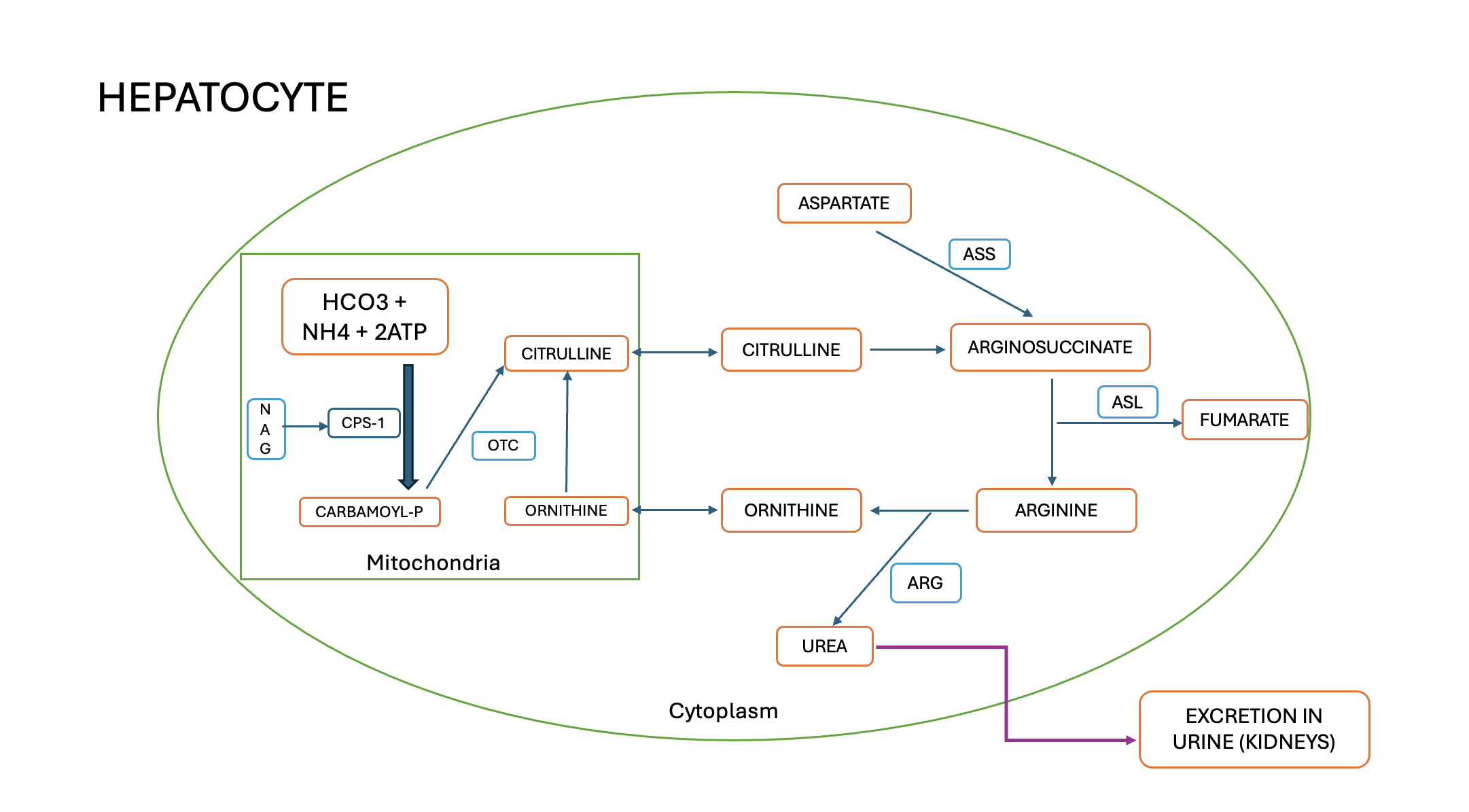
Figure: Urea Cycle
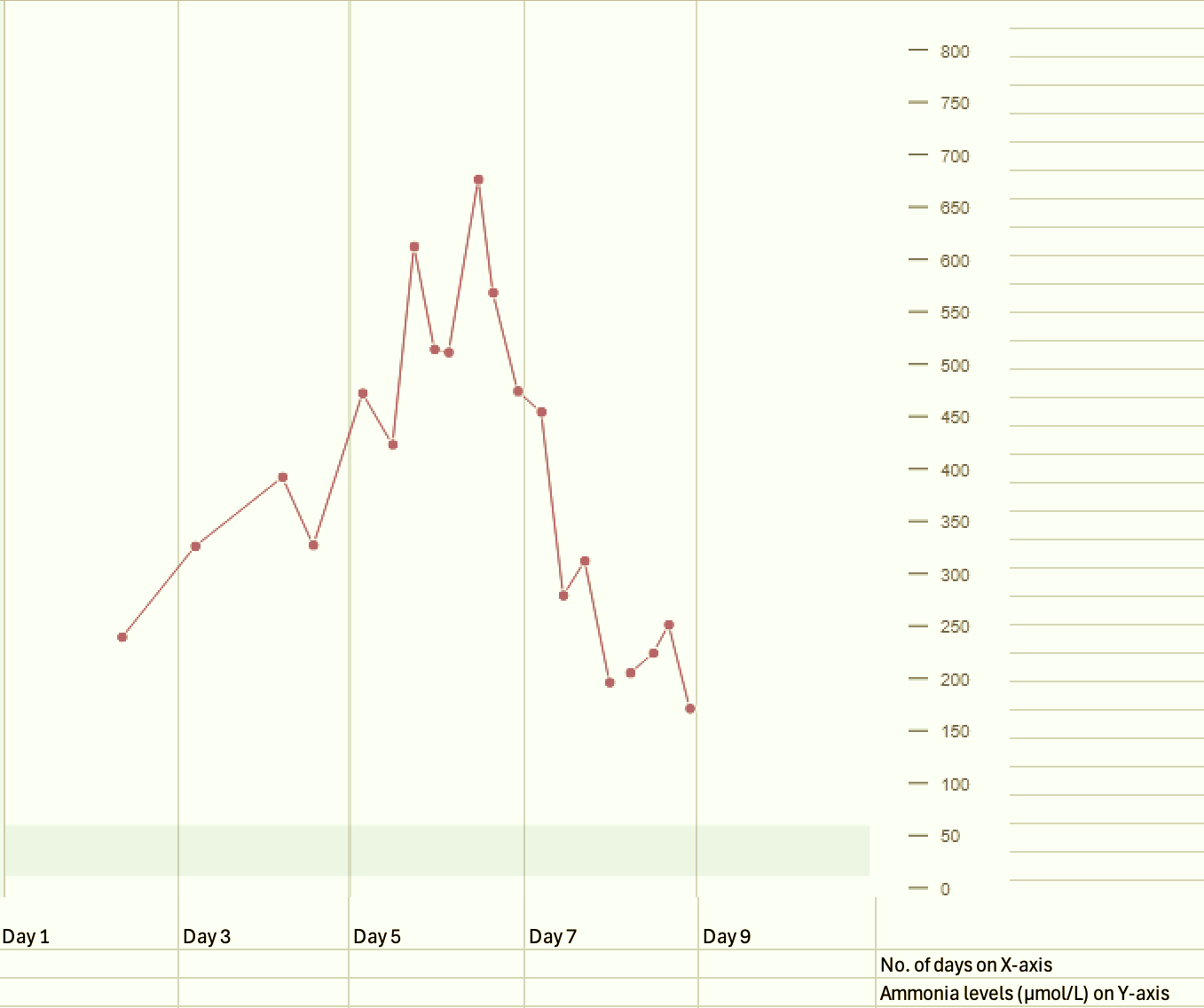
Figure: Charting of ammonia levels in our patient
Disclosures:
Vishal Chandel indicated no relevant financial relationships.
Vishal Chandel, MD. P1872 - An Unusual Case of Non-Cirrhotic Hyperammonemic Encephalopathy in an Adult Patient: Case Report and Literature Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Brigham and Women's Hospital, Harvard Medical School, Boston, MA
Introduction: Hyperammonemia is the underlying metabolic derangement in decompensated liver disease. A less common presentation is hyperammonemia in the absence of liver disease. Infections by urease producing organisms and Urea cycle disorders (UCD) should be considered for unexplained hyperammonemia. We present a case of non-cirrhotic hyperammonemia (NCH) complicated by cerebral edema that failed conventional therapy.
Case Description/
Methods: A 45-year-old female with multiple sclerosis (on monoclonal antibody) presented with acute abdominal pain. Imaging revealed pneumoperitoneum from gastric perforation secondary to chronic steroid use. The course was further complicated by intraabdominal sepsis due to gastric leak. During treatment, patient developed progressively elevated ammonia levels of unclear etiology as the patient had no history of liver disease. The peak ammonia was 676 μmol/L (normal range 11–60). Labs and imaging did not demonstrate cirrhosis or acute liver failure. Ammonia remained elevated despite lactulose and continuous renal replacement therapy. Encephalopathy ensued with neurologic deterioration requiring intubation. The patient required parenteral nutrition (PN) due to gastric leak and recent wedge resection. Amino acids were removed from PN when the ammonia level was 326 μmol/L. The patient was found to have positive rare Ureaplasma species. Azithromycin, doxycycline and levofloxacin were started but patient continued to decline with progressive worsening of mental status eventually leading to cerebral edema, herniation and death.
Discussion: In our case, patient had NCH non-responsive to treatment. The mechanism is likely related to either having an undiagnosed inborn error of metabolism (IEM) or an infection with urea producing organism in the setting of severe immunocompromised status and post-surgical complications. In this patient, chronic steroid and immunomodulator use either unmasked IEMs or gave a flourishing medium for urease-producing organisms. Although IEMs often have early age of onset, UCDs can present at later age. Ornithine transcarbamylase deficiency is the most common UCD and can present with reduced plasma citrulline in both children and adults. Treating a potential IEM begins prior to confirmation of an etiology. Treatment should start early if UCD is suspected. Timely intervention is essential to prevent mortality. Early treatment includes holding proteins, providing ammonia scavengers along with renal replacement to reduce ammonia levels.
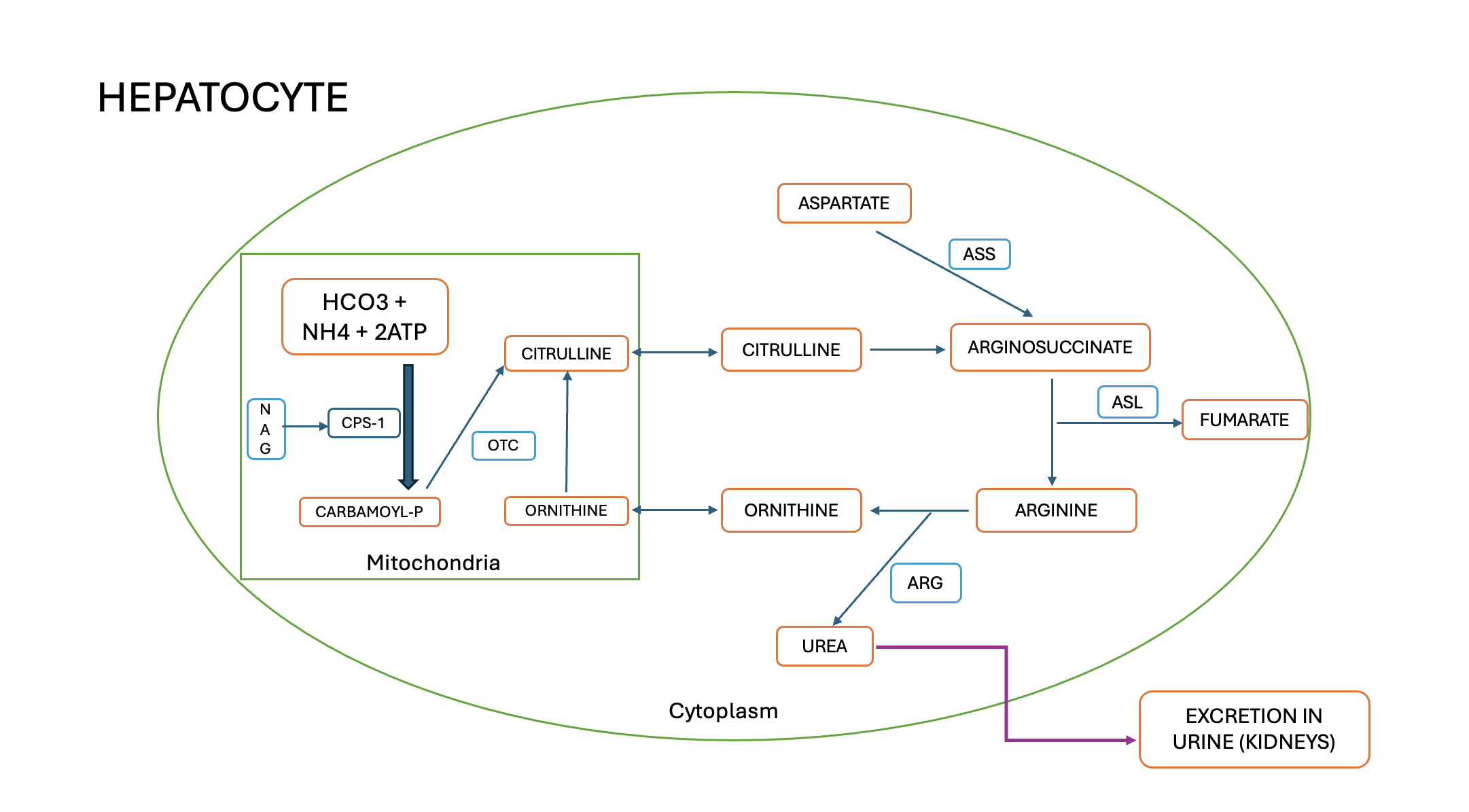
Figure: Urea Cycle
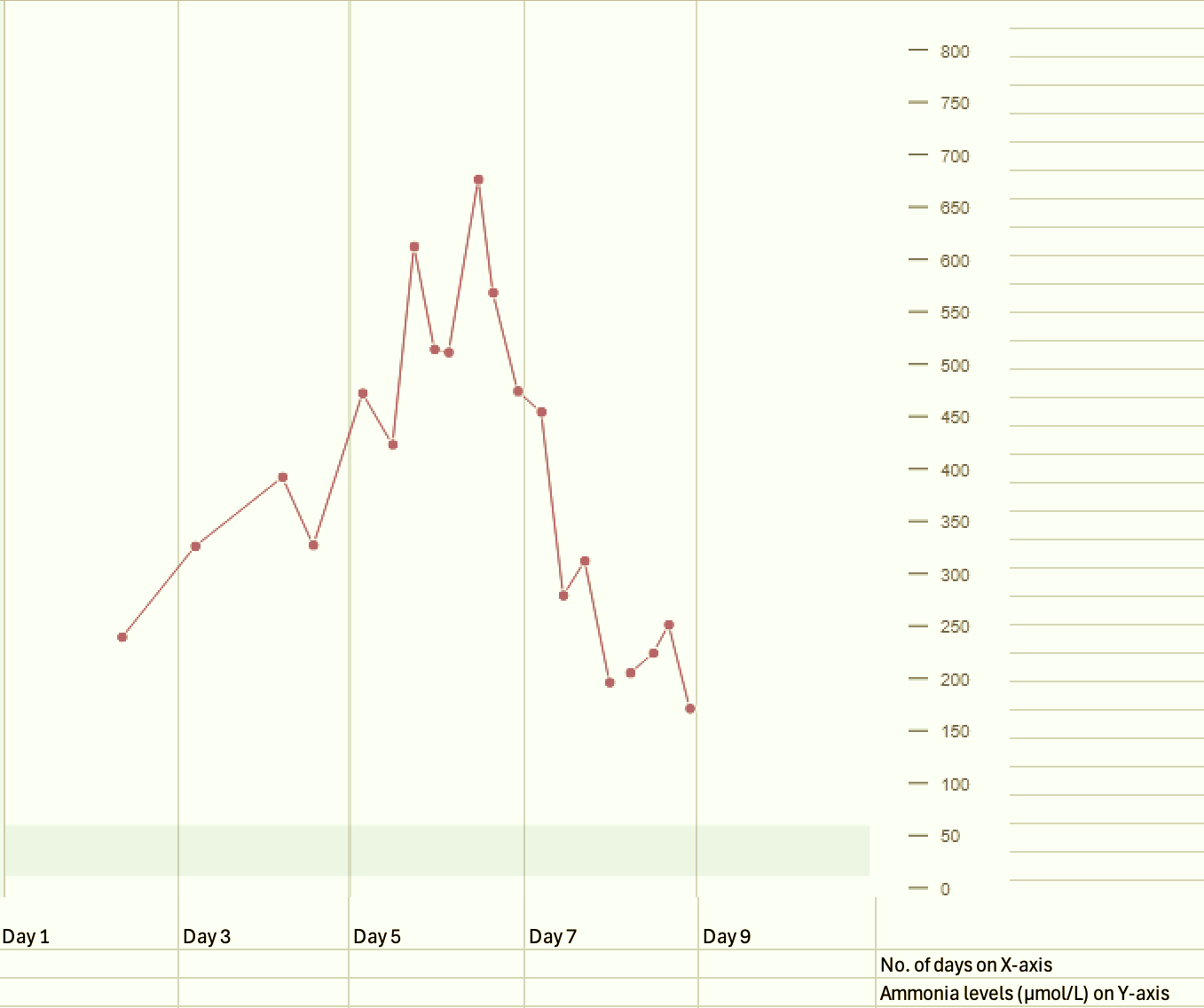
Figure: Charting of ammonia levels in our patient
Disclosures:
Vishal Chandel indicated no relevant financial relationships.
Vishal Chandel, MD. P1872 - An Unusual Case of Non-Cirrhotic Hyperammonemic Encephalopathy in an Adult Patient: Case Report and Literature Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
