Sunday Poster Session
Category: Liver
P1829 - Hepatic Candidiasis in a Patient With ANCA-Associated Vasculitis Following Immunosuppressant-Induced Neutropenia
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Rahul Kumar, MD (he/him/his)
North Central Bronx Hospital
Bronx, NY
Presenting Author(s)
Rahul Kumar, MD1, Joo Hee Park, MD1, Avinash Nankani, MBBS2, Sunny Kumar, MD3, Fnu Vikash, MD4, Miroslav Radulovic, MD1, Sunny Patel, MD5
1North Central Bronx Hospital, Bronx, NY; 2Dow University of Health Sciences, Karachi, Sindh, Pakistan; 3Wright Center for Graduate Medical Education, Scranton, PA; 4Cleveland Clinic Foundation, Bronx, NY; 5NYC Health + Hospitals/Jacobi, Bronx, NY
Introduction: Chronic disseminated candidiasis (CDC), or hepatosplenic candidiasis, is a rare but serious fungal infection that typically arises in patients with hematologic malignancies during recovery from prolonged neutropenia. It is often linked to translocation of Candida species through damaged gastrointestinal mucosa during neutropenia, with seeding of organs like the liver and spleen once immune recovery begins. Although most common in cancer patients, it may also occur in those with autoimmune diseases receiving immunosuppressive therapy.
Case Description/
Methods: An 82-year-old woman with ANCA-associated vasculitis presented with 5 days of right upper quadrant pain, nausea, and vomiting. Her history included ILD, pauci-immune glomerulonephritis, COVID-related ARDS, CMV pneumonitis, and hemorrhagic cholecystitis with prior cholecystostomy. Azathioprine had been discontinued 5 months earlier due to neutropenic fever; she remained on prednisone. Neutrophils had since recovered.
Labs: WBC 34.14 /nL, Cr 2.0 mg/dL, ALP 2296 U/L, AST 107, ALT 45, TBili 4.3. MRCP showed biliary dilation with an obstructive lesion. ERCP retrieved three stones and a clot; cholangiogram confirmed clearance. However, liver enzymes remained elevated.
CT revealed a 16.4 × 12.0 cm multiloculated subcapsular perihepatic collection. IR drained 360 cc of dark brown fluid. Blood cultures were negative, but aspirate grew Candida albicans. Oral fluconazole was started, with rapid clinical and biochemical improvement. Residual fluid was treated with intralesional Dornase and Alteplase. Follow-up imaging showed near-complete resolution, and the patient remained asymptomatic.
Discussion: Hepatic candidiasis in immunocompetent or autoimmune patients is rare and often presents with nonspecific symptoms and abnormal liver tests. It frequently occurs without candidemia, and blood cultures lack sensitivity. Diagnosis depends on clinical suspicion, imaging, and aspirate culture or histology. Targeted antifungal therapy is the cornerstone of treatment, and fluconazole is often effective in susceptible cases. In our patient, prompt oral fluconazole and adjunctive intralesional fibrinolytics led to full recovery. This case highlights the importance of early recognition, appropriate antifungal therapy, and multidisciplinary management for optimal outcomes.
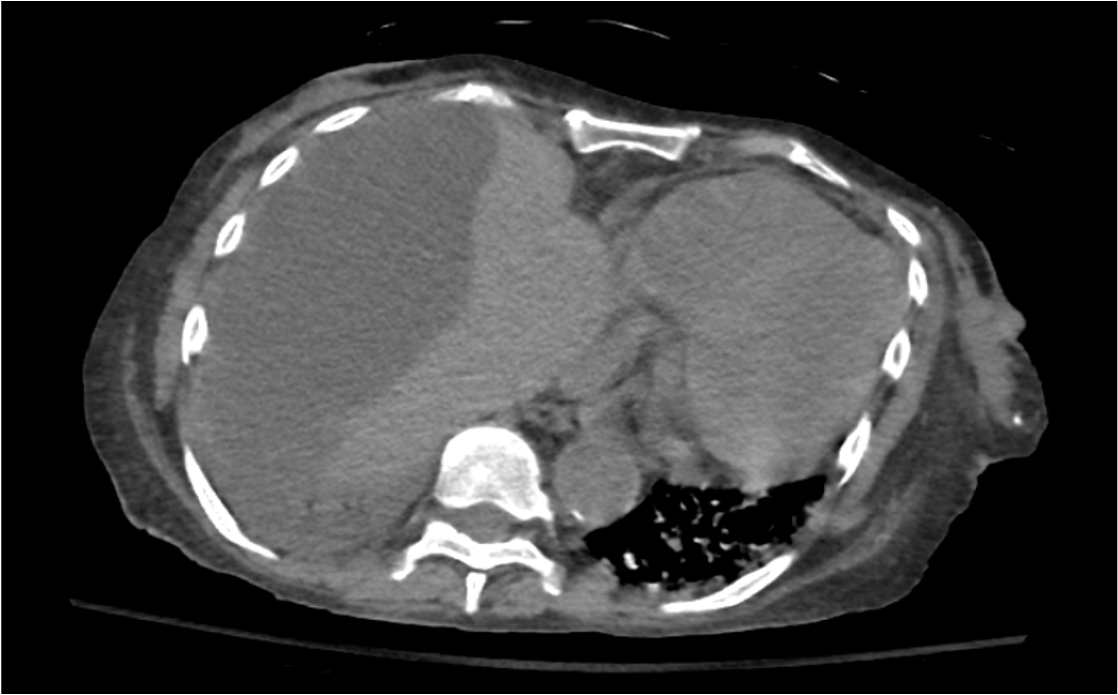
Figure: Figure 1. Axial CT showing subcapsular perihepatic fluid collection (~164 × 120 mm) consistent with hepatic abscess.
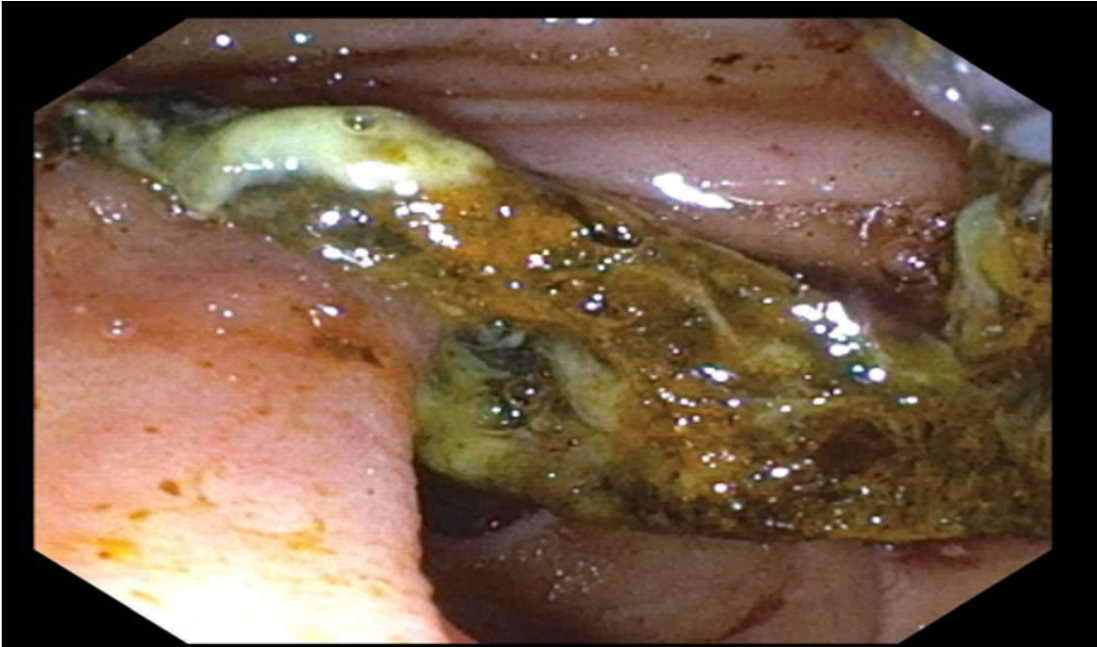
Figure: Figure 2: Endoscopic view during ERCP showing extraction of a large clot, sludge, and stone fragments from the biliary duct.
Disclosures:
Rahul Kumar indicated no relevant financial relationships.
Joo Hee Park indicated no relevant financial relationships.
Avinash Nankani indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Fnu Vikash indicated no relevant financial relationships.
Miroslav Radulovic indicated no relevant financial relationships.
Sunny Patel indicated no relevant financial relationships.
Rahul Kumar, MD1, Joo Hee Park, MD1, Avinash Nankani, MBBS2, Sunny Kumar, MD3, Fnu Vikash, MD4, Miroslav Radulovic, MD1, Sunny Patel, MD5. P1829 - Hepatic Candidiasis in a Patient With ANCA-Associated Vasculitis Following Immunosuppressant-Induced Neutropenia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1North Central Bronx Hospital, Bronx, NY; 2Dow University of Health Sciences, Karachi, Sindh, Pakistan; 3Wright Center for Graduate Medical Education, Scranton, PA; 4Cleveland Clinic Foundation, Bronx, NY; 5NYC Health + Hospitals/Jacobi, Bronx, NY
Introduction: Chronic disseminated candidiasis (CDC), or hepatosplenic candidiasis, is a rare but serious fungal infection that typically arises in patients with hematologic malignancies during recovery from prolonged neutropenia. It is often linked to translocation of Candida species through damaged gastrointestinal mucosa during neutropenia, with seeding of organs like the liver and spleen once immune recovery begins. Although most common in cancer patients, it may also occur in those with autoimmune diseases receiving immunosuppressive therapy.
Case Description/
Methods: An 82-year-old woman with ANCA-associated vasculitis presented with 5 days of right upper quadrant pain, nausea, and vomiting. Her history included ILD, pauci-immune glomerulonephritis, COVID-related ARDS, CMV pneumonitis, and hemorrhagic cholecystitis with prior cholecystostomy. Azathioprine had been discontinued 5 months earlier due to neutropenic fever; she remained on prednisone. Neutrophils had since recovered.
Labs: WBC 34.14 /nL, Cr 2.0 mg/dL, ALP 2296 U/L, AST 107, ALT 45, TBili 4.3. MRCP showed biliary dilation with an obstructive lesion. ERCP retrieved three stones and a clot; cholangiogram confirmed clearance. However, liver enzymes remained elevated.
CT revealed a 16.4 × 12.0 cm multiloculated subcapsular perihepatic collection. IR drained 360 cc of dark brown fluid. Blood cultures were negative, but aspirate grew Candida albicans. Oral fluconazole was started, with rapid clinical and biochemical improvement. Residual fluid was treated with intralesional Dornase and Alteplase. Follow-up imaging showed near-complete resolution, and the patient remained asymptomatic.
Discussion: Hepatic candidiasis in immunocompetent or autoimmune patients is rare and often presents with nonspecific symptoms and abnormal liver tests. It frequently occurs without candidemia, and blood cultures lack sensitivity. Diagnosis depends on clinical suspicion, imaging, and aspirate culture or histology. Targeted antifungal therapy is the cornerstone of treatment, and fluconazole is often effective in susceptible cases. In our patient, prompt oral fluconazole and adjunctive intralesional fibrinolytics led to full recovery. This case highlights the importance of early recognition, appropriate antifungal therapy, and multidisciplinary management for optimal outcomes.
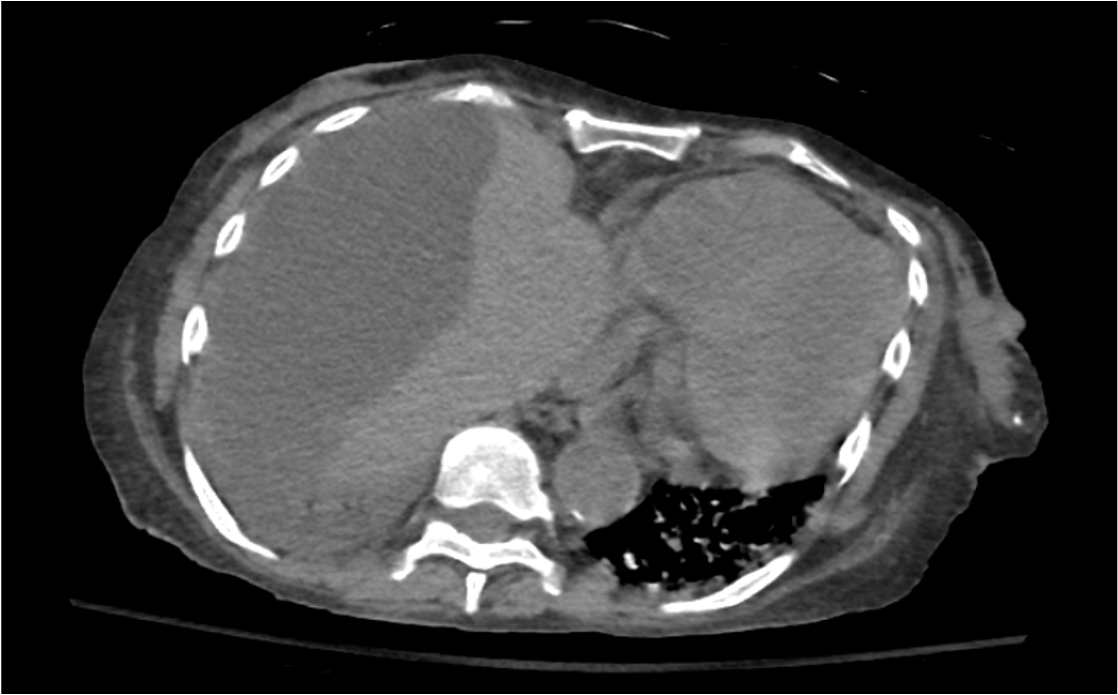
Figure: Figure 1. Axial CT showing subcapsular perihepatic fluid collection (~164 × 120 mm) consistent with hepatic abscess.
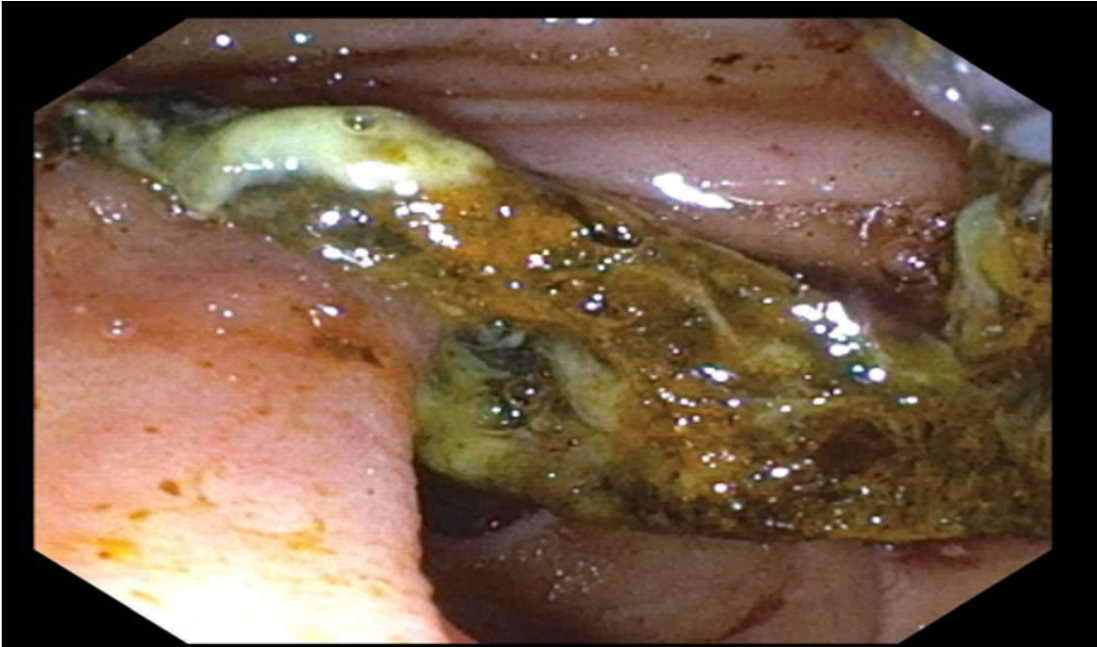
Figure: Figure 2: Endoscopic view during ERCP showing extraction of a large clot, sludge, and stone fragments from the biliary duct.
Disclosures:
Rahul Kumar indicated no relevant financial relationships.
Joo Hee Park indicated no relevant financial relationships.
Avinash Nankani indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Fnu Vikash indicated no relevant financial relationships.
Miroslav Radulovic indicated no relevant financial relationships.
Sunny Patel indicated no relevant financial relationships.
Rahul Kumar, MD1, Joo Hee Park, MD1, Avinash Nankani, MBBS2, Sunny Kumar, MD3, Fnu Vikash, MD4, Miroslav Radulovic, MD1, Sunny Patel, MD5. P1829 - Hepatic Candidiasis in a Patient With ANCA-Associated Vasculitis Following Immunosuppressant-Induced Neutropenia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
