Sunday Poster Session
Category: Liver
P1827 - Banding Ulcer Hemorrhage Controlled by Esophageal Stent Placement as a Bridge to Transplant
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Carter Edmunds, MD
University of Alabama at Birmingham
Birmingham, AL
Presenting Author(s)
Award: ACG Presidential Poster Award
Carter Edmunds, MD1, Joshua G.. Fricker, MD2, Mohamed Shoreibah, MD1, Shajan Peter, MD1, Dala Eloubeidi, MD3
1University of Alabama at Birmingham, Birmingham, AL; 2University of Alabama at Birmingham Medical Center, Birmingham, AL; 3University of Alabama at Birmingham Hospital, Birmingham, AL
Introduction: Banding ulcers are an uncommon but potentially life-threatening complication of variceal banding in patients with cirrhosis, with bleeding estimated to occur in approximately 3% of cases. The ulcers can erode into adjacent vasculature and cause hemorrhagic shock that is often refractory to conventional therapies due to the ulcer’s location and friability of the mucosa. Although esophageal self-expanding metal stents (SEMS) are often used more commonly as a salvage therapy for refractory bleeding, their role for managing hemorrhage from banding ulcers is not well defined currently. We present a case of severe bleeding from esophageal banding ulcers that was successfully managed by SEMS as a bridge to liver transplantation.
Case Description/
Methods: A 41-year-old man with recently diagnosed alcohol-associated decompensated cirrhosis was transferred to our institution for emergent liver transplant evaluation following an episode of esophageal variceal hemorrhage managed with band ligation at an outside hospital. On arrival, he developed melena and worsening anemia. Esophagogastroduodenoscopy (EGD) demonstrated grade II distal esophageal varices and two superficial ulcers (Fig. 1A). Due to the ulcer’s location, the decision was made against further banding. Over the following 24 hours, the patient continued to have signs of further bleeding with worsening hemodynamic instability requiring vasopressor support. Given his high MELD score and concern that a TIPS would worsen underlying liver dysfunction, the decision was made to place an esophageal stent across the distal esophagus for hemostasis (Fig. 1B-C). Bleeding resolved shortly after the stent placement, and vasopressors were discontinued within 12 hours. The patient underwent successful orthotopic liver transplantation within 72 hours of the initial stent placement. The SEMS was removed uneventfully one month later during follow-up EGD as an outpatient.
Discussion: This case demonstrates the potential role that esophageal self-expanding metal stents can provide for controlling bleeding from banding ulcers. Although banding ulcers are uncommon, they are a potential cause of massive hemorrhage in this patient population, who are commonly not appropriate candidates for TIPS due to the severity of their underlying liver dysfunction. In these cases, SEMS can potentially lead to successful hemostasis and serve as a bridge to definitive therapy, such as liver transplantation, for high-risk patients.
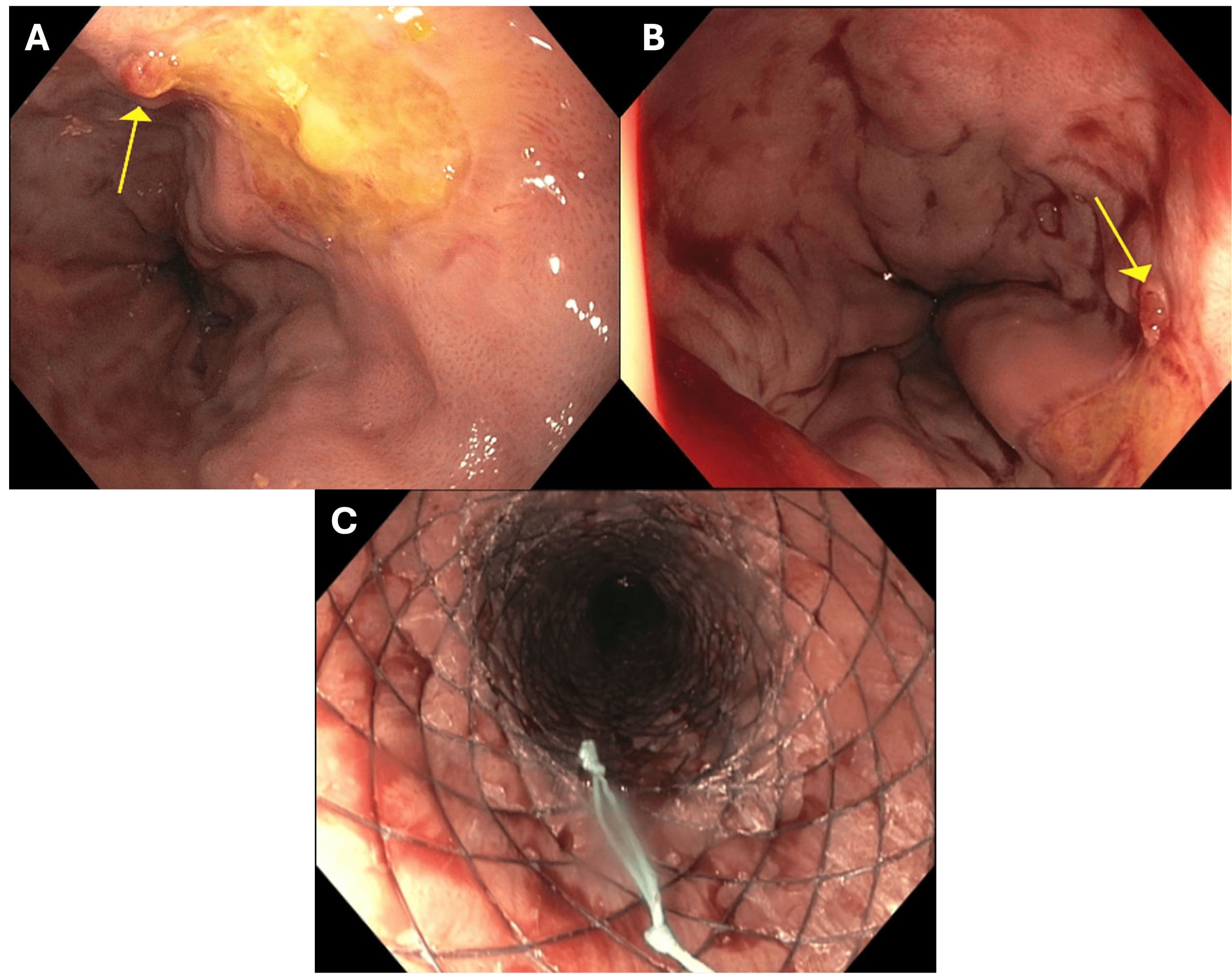
Figure: Figure 1. A) Upper endoscopy with esophageal varices and superficial banding ulcers, one with a nipple sign overlapping the edge. B) Subsequent upper endoscopy for stent placement with evidence of recent bleeding; however, no evidence of active bleeding. Banding ulcer noted by arrow. C) Successful self-expanding metal stent placement in the distal esophagus.
Disclosures:
Carter Edmunds indicated no relevant financial relationships.
Joshua Fricker indicated no relevant financial relationships.
Mohamed Shoreibah indicated no relevant financial relationships.
Shajan Peter: Castle biosciences – Advisory Committee/Board Member. Olympus corporation – Advisory Committee/Board Member.
Dala Eloubeidi indicated no relevant financial relationships.
Carter Edmunds, MD1, Joshua G.. Fricker, MD2, Mohamed Shoreibah, MD1, Shajan Peter, MD1, Dala Eloubeidi, MD3. P1827 - Banding Ulcer Hemorrhage Controlled by Esophageal Stent Placement as a Bridge to Transplant, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Carter Edmunds, MD1, Joshua G.. Fricker, MD2, Mohamed Shoreibah, MD1, Shajan Peter, MD1, Dala Eloubeidi, MD3
1University of Alabama at Birmingham, Birmingham, AL; 2University of Alabama at Birmingham Medical Center, Birmingham, AL; 3University of Alabama at Birmingham Hospital, Birmingham, AL
Introduction: Banding ulcers are an uncommon but potentially life-threatening complication of variceal banding in patients with cirrhosis, with bleeding estimated to occur in approximately 3% of cases. The ulcers can erode into adjacent vasculature and cause hemorrhagic shock that is often refractory to conventional therapies due to the ulcer’s location and friability of the mucosa. Although esophageal self-expanding metal stents (SEMS) are often used more commonly as a salvage therapy for refractory bleeding, their role for managing hemorrhage from banding ulcers is not well defined currently. We present a case of severe bleeding from esophageal banding ulcers that was successfully managed by SEMS as a bridge to liver transplantation.
Case Description/
Methods: A 41-year-old man with recently diagnosed alcohol-associated decompensated cirrhosis was transferred to our institution for emergent liver transplant evaluation following an episode of esophageal variceal hemorrhage managed with band ligation at an outside hospital. On arrival, he developed melena and worsening anemia. Esophagogastroduodenoscopy (EGD) demonstrated grade II distal esophageal varices and two superficial ulcers (Fig. 1A). Due to the ulcer’s location, the decision was made against further banding. Over the following 24 hours, the patient continued to have signs of further bleeding with worsening hemodynamic instability requiring vasopressor support. Given his high MELD score and concern that a TIPS would worsen underlying liver dysfunction, the decision was made to place an esophageal stent across the distal esophagus for hemostasis (Fig. 1B-C). Bleeding resolved shortly after the stent placement, and vasopressors were discontinued within 12 hours. The patient underwent successful orthotopic liver transplantation within 72 hours of the initial stent placement. The SEMS was removed uneventfully one month later during follow-up EGD as an outpatient.
Discussion: This case demonstrates the potential role that esophageal self-expanding metal stents can provide for controlling bleeding from banding ulcers. Although banding ulcers are uncommon, they are a potential cause of massive hemorrhage in this patient population, who are commonly not appropriate candidates for TIPS due to the severity of their underlying liver dysfunction. In these cases, SEMS can potentially lead to successful hemostasis and serve as a bridge to definitive therapy, such as liver transplantation, for high-risk patients.
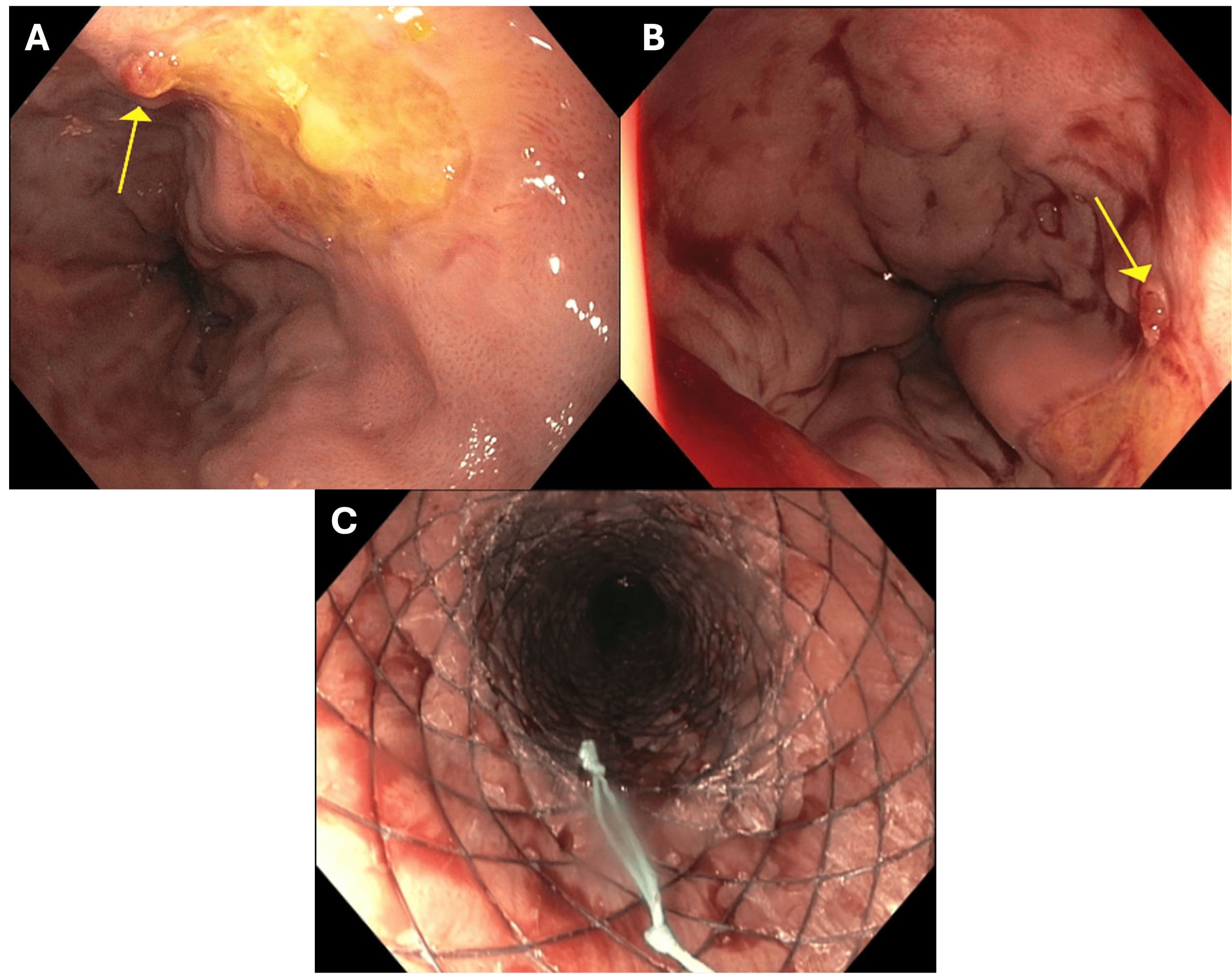
Figure: Figure 1. A) Upper endoscopy with esophageal varices and superficial banding ulcers, one with a nipple sign overlapping the edge. B) Subsequent upper endoscopy for stent placement with evidence of recent bleeding; however, no evidence of active bleeding. Banding ulcer noted by arrow. C) Successful self-expanding metal stent placement in the distal esophagus.
Disclosures:
Carter Edmunds indicated no relevant financial relationships.
Joshua Fricker indicated no relevant financial relationships.
Mohamed Shoreibah indicated no relevant financial relationships.
Shajan Peter: Castle biosciences – Advisory Committee/Board Member. Olympus corporation – Advisory Committee/Board Member.
Dala Eloubeidi indicated no relevant financial relationships.
Carter Edmunds, MD1, Joshua G.. Fricker, MD2, Mohamed Shoreibah, MD1, Shajan Peter, MD1, Dala Eloubeidi, MD3. P1827 - Banding Ulcer Hemorrhage Controlled by Esophageal Stent Placement as a Bridge to Transplant, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

