Sunday Poster Session
Category: Liver
P1805 - Atypical Parkinsonism in a Cirrhotic Patient: A Case of Acquired Hepatocerebral Degeneration
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- MH
Maryam Haider, MD
University of Chicago Northshore
Lincolnshire, IL
Presenting Author(s)
Maryam Haider, MD1, Raza Muhammad, DO2, Dhiren Shah, MD3
1University of Chicago Northshore, Lincolnshire, IL; 2University of Chicago/Northshore, Evanston, IL; 3University of Chicago Northshore, Glenview, IL
Introduction: Acquired Hepatocerebral Degeneration (AHD) is a rare neurological disorder that occurs in patients with chronic liver disease, characterized by progressive neurological impairments due to hepatobiliary dysfunction and portosystemic shunting. We present a case of AHD in a patient with hepatic sarcoidosis-related cirrhosis.
Case Description/
Methods: A 72-year-old male with cirrhosis secondary to hepatic sarcoidosis complicated by esophageal varices status post-TIPS, presented with altered mental status and bilateral lower extremity swelling. Vitals were stable. On exam, the patient was alert and oriented to person only (A&Ox1), spontaneous movement, no significant abdominal distension, arm contractures, and 3+ pitting edema in lower limbs. After treatment with the lactulose enema, mentation improved but he was unable to stand without assistance, though he had walked independently a week prior, neurological exam now showed hypomimia, dysarthria, and generalized bradykinesia with rigidity . Initial Labs showed elevated LFT’s(T. bilirubin 2.3, Alk Phos 365, AST/ALT 137/60), WBC 12.8, Hb 11.4, platelets 327, and ammonia 109. Initial infectious work-up was negative. CT head revealed minimal chronic small vessel disease. Brain MRI showed T1 hyperintense signals in globus pallidus and midbrain, and T2 FLAIR signals in cerebellar peduncles, findings suggestive of AHD. Neurology noted that the rapid progression and early gait instability are atypical for idiopathic Parkinson’s disease, suggesting an atypical parkinsonism, possibly secondary to hepatocerebral degeneration.
Discussion: AHD can occur in advanced hepatobiliary diseases, often with cirrhosis, especially with portosystemic shunting. The pathogenesis remains unclear; a theory suggests that accumulation of neurotoxins such as manganese and ammonia bypass hepatic clearance and cross the blood-brain barrier which leads to central nervous system dysfunction. Hyperammonemia impairs astrocyte function, causing brain edema and nitrosative stress, potentially contributing to AHD. This case highlights the interconnection between chronic liver disease and AHD. Early recognition and understanding of the pathophysiology are vital for managing and potentially alleviating cerebral impacts. Though there is no definitive treatment, symptomatic management, including medications and possibly early liver transplantation, might offer relief. Vigilant monitoring and comprehensive assessments are crucial in managing AHD complexities.
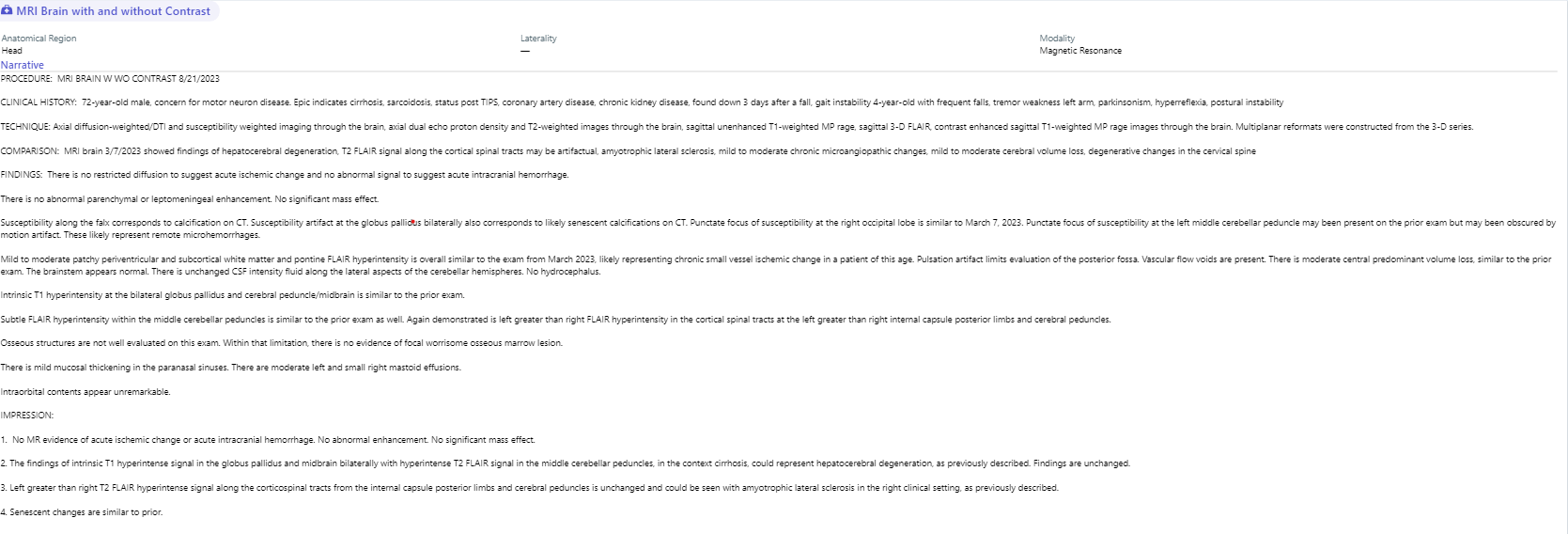
Figure: Fig1. MRI BRAIN WITH AND WITHOUT CONTRAST

Figure: Fig2. CT Head showing minimal chronic small vessel disease and age-appropriate mild to moderate volume loss.
Disclosures:
Maryam Haider indicated no relevant financial relationships.
Raza Muhammad indicated no relevant financial relationships.
Dhiren Shah indicated no relevant financial relationships.
Maryam Haider, MD1, Raza Muhammad, DO2, Dhiren Shah, MD3. P1805 - Atypical Parkinsonism in a Cirrhotic Patient: A Case of Acquired Hepatocerebral Degeneration, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Chicago Northshore, Lincolnshire, IL; 2University of Chicago/Northshore, Evanston, IL; 3University of Chicago Northshore, Glenview, IL
Introduction: Acquired Hepatocerebral Degeneration (AHD) is a rare neurological disorder that occurs in patients with chronic liver disease, characterized by progressive neurological impairments due to hepatobiliary dysfunction and portosystemic shunting. We present a case of AHD in a patient with hepatic sarcoidosis-related cirrhosis.
Case Description/
Methods: A 72-year-old male with cirrhosis secondary to hepatic sarcoidosis complicated by esophageal varices status post-TIPS, presented with altered mental status and bilateral lower extremity swelling. Vitals were stable. On exam, the patient was alert and oriented to person only (A&Ox1), spontaneous movement, no significant abdominal distension, arm contractures, and 3+ pitting edema in lower limbs. After treatment with the lactulose enema, mentation improved but he was unable to stand without assistance, though he had walked independently a week prior, neurological exam now showed hypomimia, dysarthria, and generalized bradykinesia with rigidity . Initial Labs showed elevated LFT’s(T. bilirubin 2.3, Alk Phos 365, AST/ALT 137/60), WBC 12.8, Hb 11.4, platelets 327, and ammonia 109. Initial infectious work-up was negative. CT head revealed minimal chronic small vessel disease. Brain MRI showed T1 hyperintense signals in globus pallidus and midbrain, and T2 FLAIR signals in cerebellar peduncles, findings suggestive of AHD. Neurology noted that the rapid progression and early gait instability are atypical for idiopathic Parkinson’s disease, suggesting an atypical parkinsonism, possibly secondary to hepatocerebral degeneration.
Discussion: AHD can occur in advanced hepatobiliary diseases, often with cirrhosis, especially with portosystemic shunting. The pathogenesis remains unclear; a theory suggests that accumulation of neurotoxins such as manganese and ammonia bypass hepatic clearance and cross the blood-brain barrier which leads to central nervous system dysfunction. Hyperammonemia impairs astrocyte function, causing brain edema and nitrosative stress, potentially contributing to AHD. This case highlights the interconnection between chronic liver disease and AHD. Early recognition and understanding of the pathophysiology are vital for managing and potentially alleviating cerebral impacts. Though there is no definitive treatment, symptomatic management, including medications and possibly early liver transplantation, might offer relief. Vigilant monitoring and comprehensive assessments are crucial in managing AHD complexities.
Figure: Fig1. MRI BRAIN WITH AND WITHOUT CONTRAST

Figure: Fig2. CT Head showing minimal chronic small vessel disease and age-appropriate mild to moderate volume loss.
Disclosures:
Maryam Haider indicated no relevant financial relationships.
Raza Muhammad indicated no relevant financial relationships.
Dhiren Shah indicated no relevant financial relationships.
Maryam Haider, MD1, Raza Muhammad, DO2, Dhiren Shah, MD3. P1805 - Atypical Parkinsonism in a Cirrhotic Patient: A Case of Acquired Hepatocerebral Degeneration, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
