Sunday Poster Session
Category: Liver
P1767 - Respiratory Syncytial Virus-Associated Hepatitis in a Liver Transplant Recipient
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- AA
Adaobi Ahanotu, MD (she/her/hers)
University of Maryland Medical Center
Hyattsville, MD
Presenting Author(s)
Adaobi Ahanotu, MD1, David Lee, MD, MS2, William Twaddell, MD2, Nathalie Urrunaga, MD, MS3
1University of Maryland Medical Center, Hyattsville, MD; 2University of Maryland Medical Center, Baltimore, MD; 3University of Maryland, Baltimore, MD
Introduction: RSV is a respiratory virus. Rarely, RSV can cause extra-pulmonary manifestations in the immunocompromised. However, hepatic involvement of RSV and its implications among patients who underwent liver transplant (LT) is seldom documented. By describing the clinical course and prognosis of a post-LT patient who experienced RSV-hepatitis, we can educate clinicians about this entity in LT-patients.
Case Description/
Methods: A 51-year-old female with of nonalcoholic steatohepatitis cirrhosis status post orthotopic LT (on mycophenolate and tacrolimus), presented with dyspnea. The patient had previously normal graft function. Associated symptoms included jaundice and anorexia. She had positive sick contact with RSV. On arrival, she was tachypneic with SpO2 of 43% that improved to 98% on 6L NC. Labs were notable for elevated aminotransferase in a hepatocellular pattern with a R-factor of 8.7 (AST 909, ALT 369, Alk Phos 157, T. bilirubin 1.4). In addition, respiratory viral panel was positive for RSV.
Hepatology was consulted and ordered liver ultrasound with dopplers to evaluate hepatic vasculature, acute viral hepatitis panel, autoimmune serologies, infectious panel, and held mycophenolate. All other labs were negative, and ultrasound showed patent hepatic vasculature. Her liver enzymes continued to worsen (AST 1505, ALT 1003) so liver biopsy was pursued due to concern for rejection. Her biopsy was consistent with portal and periportal inflammation (Figure 1), which corresponds to elevations in AST and ALT. Patient denied taking any new medications. Given the patient’s clinical history, most likely etiology was RSV.
Discussion: RSV leads to 60,000 hospitalizations in adults per year. Among the immunocompromised, in rare cases, RSV can affect the liver and produce hepatic inflammation and damage, as evidenced by the rise in transaminases. Throughout the admission, the patient was provided supportive care and was discharged without complications. It is presumed that early management with supportive care played an integral role in preventing liver failure.
This case is a learning point for clinicians involved with treating LT patients. LT patients are at a higher risk of hepatic infection and damage by various viruses due to the vulnerability of the graft and underlying immunosuppression. Elevation in liver enzymes should immediately prompt clinicians to consider infectious etiologies including viral infections in addition to graft rejection.
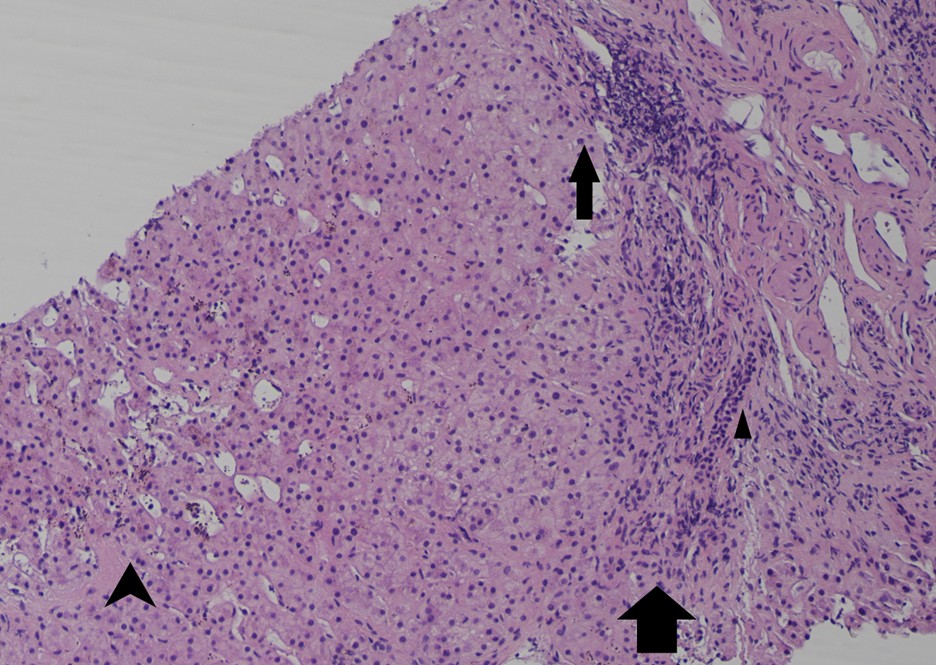
Figure: Figure 1. Standard H&E Stain of Liver Sample from patient. Sections show T-cells causing predominantly portal and periportal inflammation (solid arrows). This is not a specific finding but corresponds to elevations in AST/ALT. Typical features of rejection including bile duct damage were not present (triangle arrowhead points at preserved bile duct). There is also mild sinusoidal dilatation and iron overload (depicted by wing-like arrowhead).
Disclosures:
Adaobi Ahanotu indicated no relevant financial relationships.
David Lee indicated no relevant financial relationships.
William Twaddell indicated no relevant financial relationships.
Nathalie Urrunaga indicated no relevant financial relationships.
Adaobi Ahanotu, MD1, David Lee, MD, MS2, William Twaddell, MD2, Nathalie Urrunaga, MD, MS3. P1767 - Respiratory Syncytial Virus-Associated Hepatitis in a Liver Transplant Recipient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Maryland Medical Center, Hyattsville, MD; 2University of Maryland Medical Center, Baltimore, MD; 3University of Maryland, Baltimore, MD
Introduction: RSV is a respiratory virus. Rarely, RSV can cause extra-pulmonary manifestations in the immunocompromised. However, hepatic involvement of RSV and its implications among patients who underwent liver transplant (LT) is seldom documented. By describing the clinical course and prognosis of a post-LT patient who experienced RSV-hepatitis, we can educate clinicians about this entity in LT-patients.
Case Description/
Methods: A 51-year-old female with of nonalcoholic steatohepatitis cirrhosis status post orthotopic LT (on mycophenolate and tacrolimus), presented with dyspnea. The patient had previously normal graft function. Associated symptoms included jaundice and anorexia. She had positive sick contact with RSV. On arrival, she was tachypneic with SpO2 of 43% that improved to 98% on 6L NC. Labs were notable for elevated aminotransferase in a hepatocellular pattern with a R-factor of 8.7 (AST 909, ALT 369, Alk Phos 157, T. bilirubin 1.4). In addition, respiratory viral panel was positive for RSV.
Hepatology was consulted and ordered liver ultrasound with dopplers to evaluate hepatic vasculature, acute viral hepatitis panel, autoimmune serologies, infectious panel, and held mycophenolate. All other labs were negative, and ultrasound showed patent hepatic vasculature. Her liver enzymes continued to worsen (AST 1505, ALT 1003) so liver biopsy was pursued due to concern for rejection. Her biopsy was consistent with portal and periportal inflammation (Figure 1), which corresponds to elevations in AST and ALT. Patient denied taking any new medications. Given the patient’s clinical history, most likely etiology was RSV.
Discussion: RSV leads to 60,000 hospitalizations in adults per year. Among the immunocompromised, in rare cases, RSV can affect the liver and produce hepatic inflammation and damage, as evidenced by the rise in transaminases. Throughout the admission, the patient was provided supportive care and was discharged without complications. It is presumed that early management with supportive care played an integral role in preventing liver failure.
This case is a learning point for clinicians involved with treating LT patients. LT patients are at a higher risk of hepatic infection and damage by various viruses due to the vulnerability of the graft and underlying immunosuppression. Elevation in liver enzymes should immediately prompt clinicians to consider infectious etiologies including viral infections in addition to graft rejection.
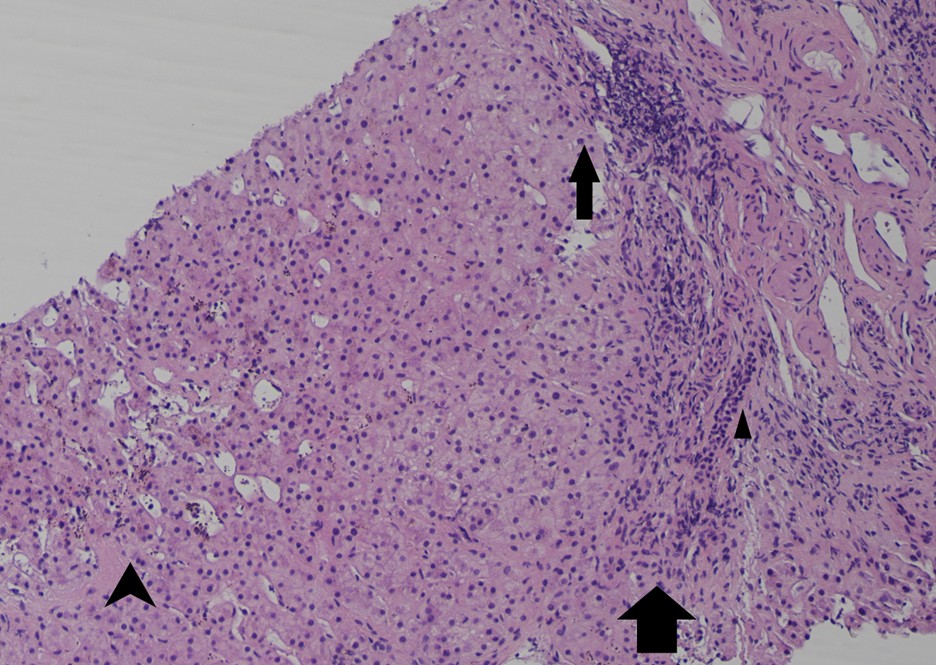
Figure: Figure 1. Standard H&E Stain of Liver Sample from patient. Sections show T-cells causing predominantly portal and periportal inflammation (solid arrows). This is not a specific finding but corresponds to elevations in AST/ALT. Typical features of rejection including bile duct damage were not present (triangle arrowhead points at preserved bile duct). There is also mild sinusoidal dilatation and iron overload (depicted by wing-like arrowhead).
Disclosures:
Adaobi Ahanotu indicated no relevant financial relationships.
David Lee indicated no relevant financial relationships.
William Twaddell indicated no relevant financial relationships.
Nathalie Urrunaga indicated no relevant financial relationships.
Adaobi Ahanotu, MD1, David Lee, MD, MS2, William Twaddell, MD2, Nathalie Urrunaga, MD, MS3. P1767 - Respiratory Syncytial Virus-Associated Hepatitis in a Liver Transplant Recipient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
