Sunday Poster Session
Category: Liver
P1763 - A Rare Case of Refractory Ascites Due to Fungal Peritonitis in a Patient With Decompensated Alcoholic Cirrhosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Ria Ghose Kundu, MD (she/her/hers)
HonorHealth
Scottsdale, AZ
Presenting Author(s)
Ria Ghose Kundu, MD1, Gavin Levinthal, MD2, Siva Talluri, MD2
1HonorHealth, Scottsdale, AZ; 2Honor Health Gastroenterology - SCOTTSDALE, AZ, Scottsdale, AZ
Introduction: Spontaneous bacterial peritonitis (SBP) is a well-established complication in patients with decompensated cirrhosis. However, spontaneous fungal peritonitis is rare, with Coccidioides spp. being an uncommon but significant pathogen in endemic regions such as the southwestern United States. Failure to recognize fungal peritonitis can lead to delays in appropriate therapy and worse outcomes.
Case Description/
Methods: A 45-year-old Native American male with a history of alcoholic cirrhosis presented on October 30, 2024, with worsening abdominal distension. Diagnostic paracentesis confirmed spontaneous bacterial peritonitis, and he was treated with intravenous ceftriaxone. He was discharged on November 5, 2024, on oral ciprofloxacin for prophylaxis, along with furosemide and spironolactone.
Despite adherence to therapy, the patient required repeat paracentesis on November 11, 2024, due to increasing abdominal girth and discomfort. Laboratory analysis of ascitic fluid showed a rising absolute neutrophil count (ANC). He was readmitted and started on intravenous ceftriaxone and piperacillin-tazobactam. Serial ascitic fluid analyses are summarized in Table 1.
Due to persistently elevated neutrophils despite broad-spectrum antibiotics, fungal peritonitis was suspected. Serologic testing for Coccidioides was positive for both IgM and IgG antibodies. Ascitic fluid β-D-glucan (Fungitell) level was elevated at 54 pg/mL on November 22, 2024.
The patient was started on an oral fluconazole loading dose of 800 mg, followed by 400 mg daily. He showed marked clinical improvement, with resolution of abdominal distension and no recurrence of ascites. He was discharged on oral fluconazole for continued outpatient therapy.
Discussion: Fungal peritonitis is an underrecognized cause of refractory ascites in cirrhotic patients, particularly in areas endemic for Coccidioides. Diagnosis is often delayed due to clinical overlap with bacterial peritonitis and the rarity of fungal causes. Serologic testing and β-D-glucan measurement are valuable diagnostic adjuncts.
This case emphasizes the need to consider fungal etiologies in patients who fail to respond to standard antibiotics, particularly among high-risk populations, including Native American and Hispanic individuals residing in endemic regions. Early initiation of antifungal therapy can lead to significant clinical improvement and may reduce morbidity.
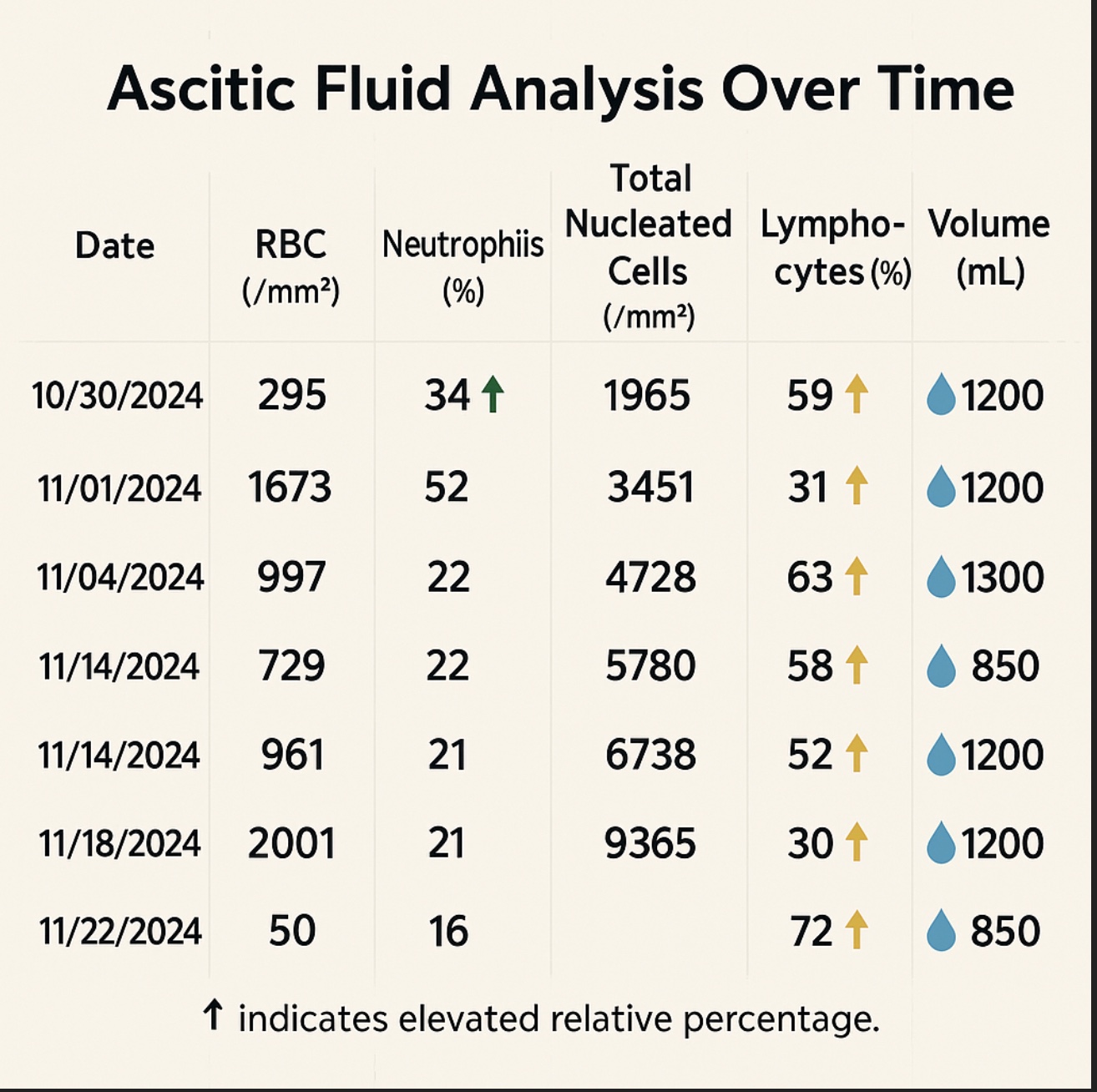
Figure: Table 1. Ascitic Fluid Analysis Over Time
Disclosures:
Ria Ghose Kundu indicated no relevant financial relationships.
Gavin Levinthal indicated no relevant financial relationships.
Siva Talluri indicated no relevant financial relationships.
Ria Ghose Kundu, MD1, Gavin Levinthal, MD2, Siva Talluri, MD2. P1763 - A Rare Case of Refractory Ascites Due to Fungal Peritonitis in a Patient With Decompensated Alcoholic Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1HonorHealth, Scottsdale, AZ; 2Honor Health Gastroenterology - SCOTTSDALE, AZ, Scottsdale, AZ
Introduction: Spontaneous bacterial peritonitis (SBP) is a well-established complication in patients with decompensated cirrhosis. However, spontaneous fungal peritonitis is rare, with Coccidioides spp. being an uncommon but significant pathogen in endemic regions such as the southwestern United States. Failure to recognize fungal peritonitis can lead to delays in appropriate therapy and worse outcomes.
Case Description/
Methods: A 45-year-old Native American male with a history of alcoholic cirrhosis presented on October 30, 2024, with worsening abdominal distension. Diagnostic paracentesis confirmed spontaneous bacterial peritonitis, and he was treated with intravenous ceftriaxone. He was discharged on November 5, 2024, on oral ciprofloxacin for prophylaxis, along with furosemide and spironolactone.
Despite adherence to therapy, the patient required repeat paracentesis on November 11, 2024, due to increasing abdominal girth and discomfort. Laboratory analysis of ascitic fluid showed a rising absolute neutrophil count (ANC). He was readmitted and started on intravenous ceftriaxone and piperacillin-tazobactam. Serial ascitic fluid analyses are summarized in Table 1.
Due to persistently elevated neutrophils despite broad-spectrum antibiotics, fungal peritonitis was suspected. Serologic testing for Coccidioides was positive for both IgM and IgG antibodies. Ascitic fluid β-D-glucan (Fungitell) level was elevated at 54 pg/mL on November 22, 2024.
The patient was started on an oral fluconazole loading dose of 800 mg, followed by 400 mg daily. He showed marked clinical improvement, with resolution of abdominal distension and no recurrence of ascites. He was discharged on oral fluconazole for continued outpatient therapy.
Discussion: Fungal peritonitis is an underrecognized cause of refractory ascites in cirrhotic patients, particularly in areas endemic for Coccidioides. Diagnosis is often delayed due to clinical overlap with bacterial peritonitis and the rarity of fungal causes. Serologic testing and β-D-glucan measurement are valuable diagnostic adjuncts.
This case emphasizes the need to consider fungal etiologies in patients who fail to respond to standard antibiotics, particularly among high-risk populations, including Native American and Hispanic individuals residing in endemic regions. Early initiation of antifungal therapy can lead to significant clinical improvement and may reduce morbidity.
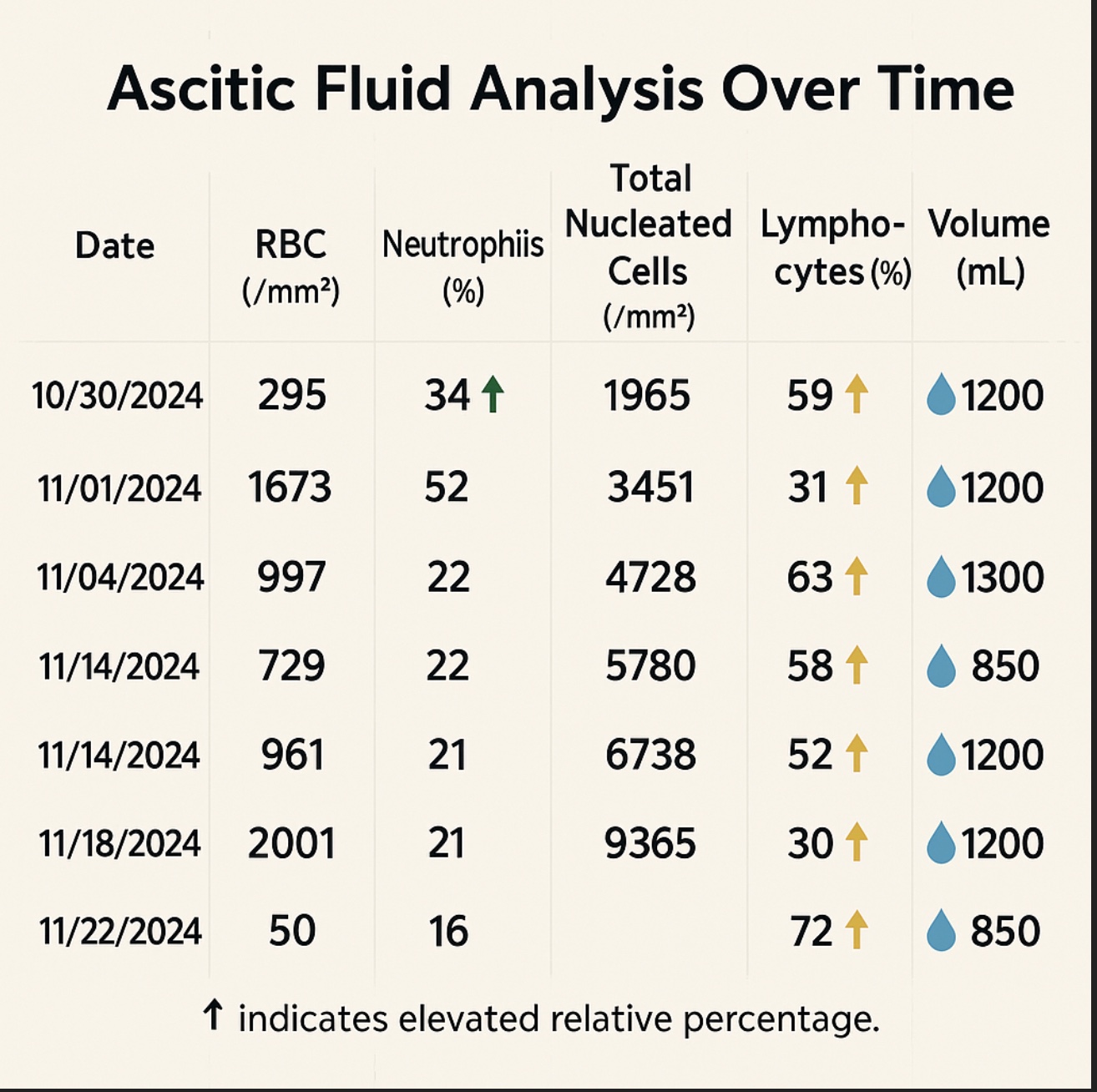
Figure: Table 1. Ascitic Fluid Analysis Over Time
Disclosures:
Ria Ghose Kundu indicated no relevant financial relationships.
Gavin Levinthal indicated no relevant financial relationships.
Siva Talluri indicated no relevant financial relationships.
Ria Ghose Kundu, MD1, Gavin Levinthal, MD2, Siva Talluri, MD2. P1763 - A Rare Case of Refractory Ascites Due to Fungal Peritonitis in a Patient With Decompensated Alcoholic Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
