Sunday Poster Session
Category: Liver
P1746 - When Lactulose Fails: A Complex Case of Hepatic Encephalopathy With Status Epilepticus and Ileus
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Amanda Sinderovsky, MD
Jefferson Torresdale Hospital
Philadelphia, PA
Presenting Author(s)
Amanda Sinderovsky, MD1, Kristin Lee, DO1, Kashif Tufail, MD2
1Jefferson Torresdale Hospital, Philadelphia, PA; 2Northeast Gastroenterology Associates, Philadelphia, PA
Introduction: Hepatic encephalopathy (HE) is a serious complication of advanced liver disease, driven by the accumulation of neurotoxins—primarily ammonia—that the liver cannot adequately clear. First-line treatments such as lactulose and rifaximin aim to reduce this toxic burden, but their effectiveness is compromised when GI motility is impaired.
Case Description/
Methods: A 62-year-old man with cirrhosis (complicated by variceal bleeding treated with banding and TIPS) and portal vein thrombosis presented with three days of worsening confusion. Labs showed elevated liver enzymes and a high-normal ammonia level (Table 1). Blood cultures grew Enterococcus faecium. CT imaging revealed a cirrhotic liver. He was admitted and started on lactulose, rifaximin, and linezolid. A 6L paracentesis was performed, though fluid studies were not obtained.
He then became obtunded, requiring intubation and transfer to the ICU. Lactulose was escalated to every two hours via orogastric tube.
The patient then developed status epilepticus. Ammonia levels peaked at 1090 µmol/L. During seizure activity, 3.2L of undigested lactulose was suctioned from the stomach. Seizures persisted on EEG despite multiple antiepileptic agents.
Stat imaging revealed new ileus and cerebral edema. Hypertonic saline and emergent dialysis were initiated. Despite maximal intervention, he remained comatose. Following goals-of-care discussions, comfort measures were instituted. He died three days later.
Discussion: Status epilepticus is a rare but deadly complication of severe HE, driven by uncontrolled hyperammonemia. In this case, ileus rendered oral lactulose ineffective, allowing ammonia levels to surge.
Prompt reduction of serum ammonia is critical to prevent cerebral edema and seizures. This case highlights the importance of assessing GI function in HE patients. When motility is impaired, rectal administration of lactulose or early dialysis should be considered.
Effective HE management requires not just timely initiation of therapy but confirmation that treatments are reaching their target. High-dose regimens without assessing GI function may be futile—or fatal.
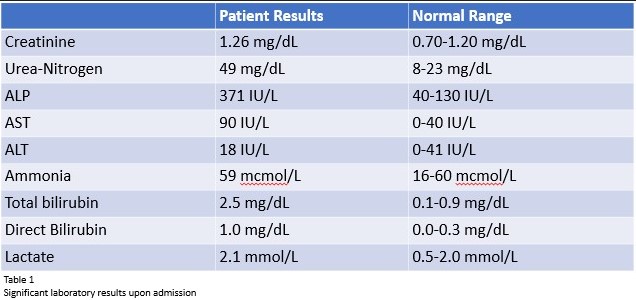
Figure: Laboratory results upon admission
Disclosures:
Amanda Sinderovsky indicated no relevant financial relationships.
Kristin Lee indicated no relevant financial relationships.
Kashif Tufail indicated no relevant financial relationships.
Amanda Sinderovsky, MD1, Kristin Lee, DO1, Kashif Tufail, MD2. P1746 - When Lactulose Fails: A Complex Case of Hepatic Encephalopathy With Status Epilepticus and Ileus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Jefferson Torresdale Hospital, Philadelphia, PA; 2Northeast Gastroenterology Associates, Philadelphia, PA
Introduction: Hepatic encephalopathy (HE) is a serious complication of advanced liver disease, driven by the accumulation of neurotoxins—primarily ammonia—that the liver cannot adequately clear. First-line treatments such as lactulose and rifaximin aim to reduce this toxic burden, but their effectiveness is compromised when GI motility is impaired.
Case Description/
Methods: A 62-year-old man with cirrhosis (complicated by variceal bleeding treated with banding and TIPS) and portal vein thrombosis presented with three days of worsening confusion. Labs showed elevated liver enzymes and a high-normal ammonia level (Table 1). Blood cultures grew Enterococcus faecium. CT imaging revealed a cirrhotic liver. He was admitted and started on lactulose, rifaximin, and linezolid. A 6L paracentesis was performed, though fluid studies were not obtained.
He then became obtunded, requiring intubation and transfer to the ICU. Lactulose was escalated to every two hours via orogastric tube.
The patient then developed status epilepticus. Ammonia levels peaked at 1090 µmol/L. During seizure activity, 3.2L of undigested lactulose was suctioned from the stomach. Seizures persisted on EEG despite multiple antiepileptic agents.
Stat imaging revealed new ileus and cerebral edema. Hypertonic saline and emergent dialysis were initiated. Despite maximal intervention, he remained comatose. Following goals-of-care discussions, comfort measures were instituted. He died three days later.
Discussion: Status epilepticus is a rare but deadly complication of severe HE, driven by uncontrolled hyperammonemia. In this case, ileus rendered oral lactulose ineffective, allowing ammonia levels to surge.
Prompt reduction of serum ammonia is critical to prevent cerebral edema and seizures. This case highlights the importance of assessing GI function in HE patients. When motility is impaired, rectal administration of lactulose or early dialysis should be considered.
Effective HE management requires not just timely initiation of therapy but confirmation that treatments are reaching their target. High-dose regimens without assessing GI function may be futile—or fatal.
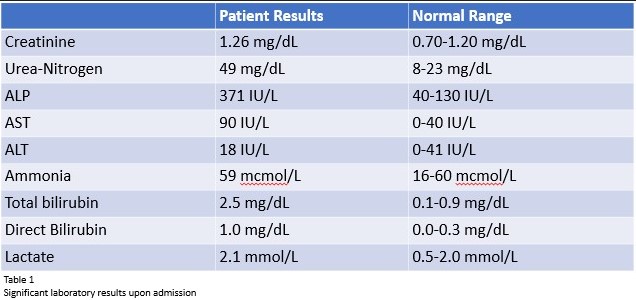
Figure: Laboratory results upon admission
Disclosures:
Amanda Sinderovsky indicated no relevant financial relationships.
Kristin Lee indicated no relevant financial relationships.
Kashif Tufail indicated no relevant financial relationships.
Amanda Sinderovsky, MD1, Kristin Lee, DO1, Kashif Tufail, MD2. P1746 - When Lactulose Fails: A Complex Case of Hepatic Encephalopathy With Status Epilepticus and Ileus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
