Sunday Poster Session
Category: Liver
P1744 - Light Chain Deposition Disease Manifesting as Acute Liver Failure
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Feruza Abraamyan, MD (she/her/hers)
Sutter Health
Carmichael, CA
Presenting Author(s)
Feruza Abraamyan, MD1, Albert Do, MD2
1Sutter Health, Roseville, CA; 2University of California Davis Health, Sacramento, CA
Introduction: Light chain deposition disease (LCDD) is rare and characterized by the deposition of non-amyloid monoclonal light chains, primarily with renal, cardiac, and/or neural involvement. Hepatic involvement with fulminant presentation would not be commonly expected, as was encountered in this case.
Case Description/
Methods: A 58-year-old healthy man was admitted with ascites, weight loss, and elevated liver tests for 3 months, without history of injurious herbal drug culprits, prescription medications, alcohol use, nor family history of liver disease. His examination did not show cutaneous findings of cirrhosis nor hepatic encephalopathy. Laboratory findings were significant for cholestasis (ALP 1071 U/L and total bilirubin 7.5 mg/dL). Viral, autoimmune etiologies, Willson’s disease, and Hemochromatosis were ruled out. Diagnostic paracentesis found SAAG 3.1, ascites total protein < 2.0, and negative cytology. CT showed moderate ascites, patent hepatic veins, and hepatomegaly with minimal surface nodularity.
Transjugular liver biopsy revealed portal hypertension with HVPG 24 mmHg without Budd-Chiari syndrome. Histology revealed hyaline within sinusoids and venous walls, sinusoidal dilatation and hepatocellular congestion and dropout, centrilobular hemorrhagic necrosis, and marked hepatocanalicular cholestasis, without fibrosis, no amyloid deposition (A). Further staining revealing lambda light chain deposition and mild kappa light chain deposition (B), consistent with LCDD, further supported by IgA monoclonal protein spike on immunoelectrophoresis and bone marrow biopsy finding a clonal lambda-restricted plasma cell population.
With worsening renal and liver injury, he urgently started daratumumab, bortezomib, and dexamethasone, and hemodialysis. However, he developed progressive multisystem organ failure with refractory ascites, hepatic encephalopathy, and distributive shock. He was transitioned to comfort care and soon expired.
Discussion: Infiltrative liver diseases are known to cause cholestatic liver disease but uncommonly cause liver failure, most observed from overwhelming infiltrative metastatic solid malignancy. LCDD is uncommon and is not expected to affect the liver fulminantly, as was observed in this patient. Recognition of uncommon etiologies of liver infiltrative diseases, such as malignancy, hemophagocytic lymphohistiocytosis, disseminated infections, and amyloidosis, can lead to timely recognition and treatment initiation, where early treatment may affect patient survival.
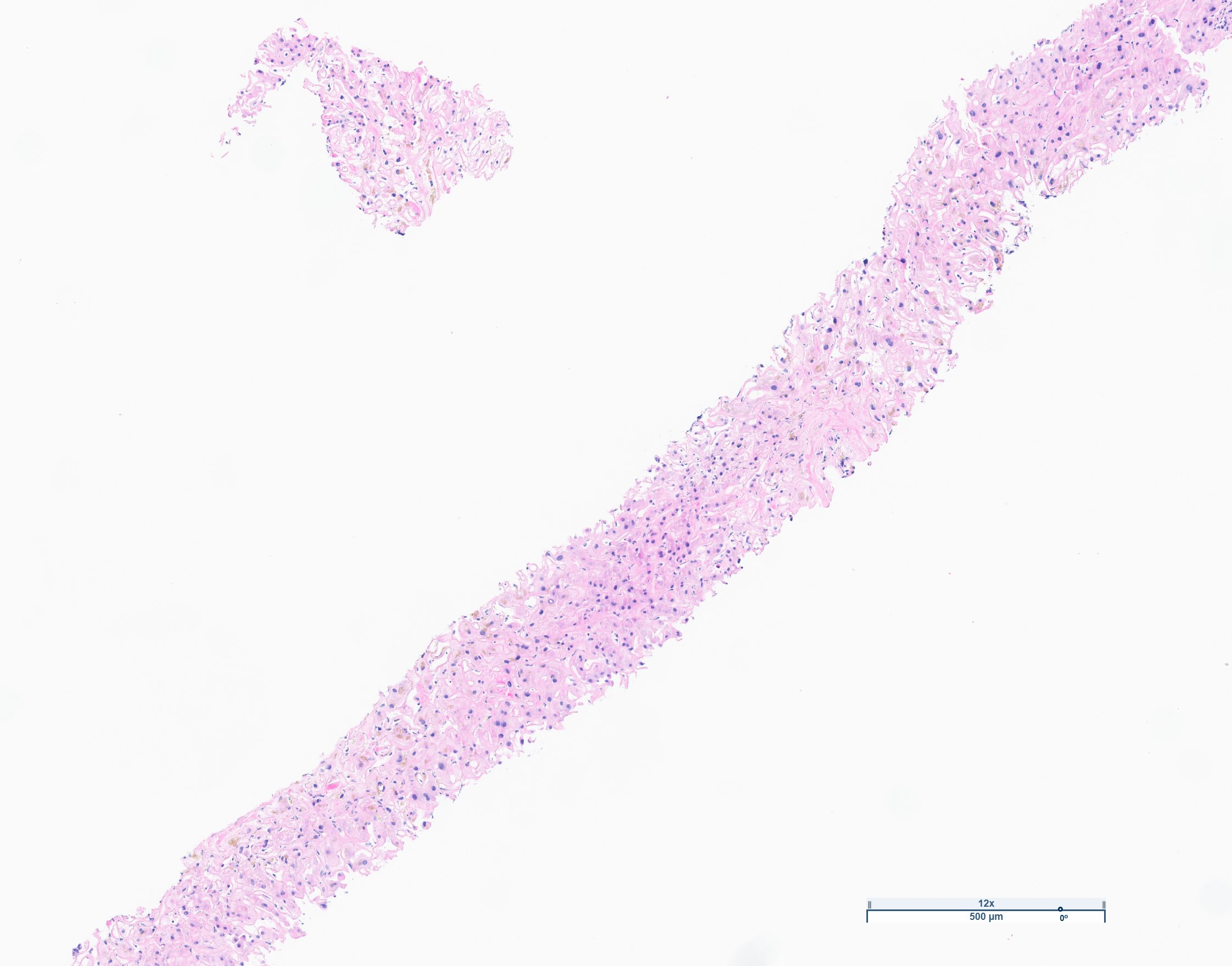
Figure: A) H&E: Diffuse and prominent perisinusoidal fibrosis, which also involves the pericentral liver parenchyma. No hepatocyte dropout, atrophy or nodularity was identified.
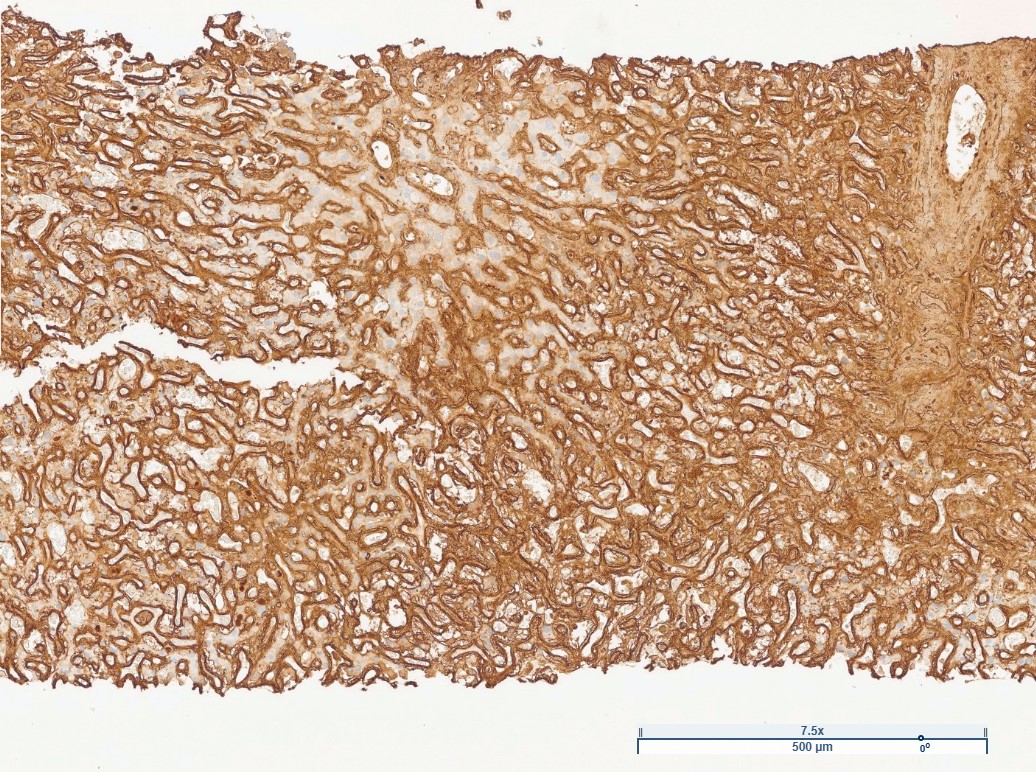
Figure: B) Lambda light chain, strong staining of sinusoidal and perivenular acellular material.
Disclosures:
Feruza Abraamyan indicated no relevant financial relationships.
Albert Do indicated no relevant financial relationships.
Feruza Abraamyan, MD1, Albert Do, MD2. P1744 - Light Chain Deposition Disease Manifesting as Acute Liver Failure, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Sutter Health, Roseville, CA; 2University of California Davis Health, Sacramento, CA
Introduction: Light chain deposition disease (LCDD) is rare and characterized by the deposition of non-amyloid monoclonal light chains, primarily with renal, cardiac, and/or neural involvement. Hepatic involvement with fulminant presentation would not be commonly expected, as was encountered in this case.
Case Description/
Methods: A 58-year-old healthy man was admitted with ascites, weight loss, and elevated liver tests for 3 months, without history of injurious herbal drug culprits, prescription medications, alcohol use, nor family history of liver disease. His examination did not show cutaneous findings of cirrhosis nor hepatic encephalopathy. Laboratory findings were significant for cholestasis (ALP 1071 U/L and total bilirubin 7.5 mg/dL). Viral, autoimmune etiologies, Willson’s disease, and Hemochromatosis were ruled out. Diagnostic paracentesis found SAAG 3.1, ascites total protein < 2.0, and negative cytology. CT showed moderate ascites, patent hepatic veins, and hepatomegaly with minimal surface nodularity.
Transjugular liver biopsy revealed portal hypertension with HVPG 24 mmHg without Budd-Chiari syndrome. Histology revealed hyaline within sinusoids and venous walls, sinusoidal dilatation and hepatocellular congestion and dropout, centrilobular hemorrhagic necrosis, and marked hepatocanalicular cholestasis, without fibrosis, no amyloid deposition (A). Further staining revealing lambda light chain deposition and mild kappa light chain deposition (B), consistent with LCDD, further supported by IgA monoclonal protein spike on immunoelectrophoresis and bone marrow biopsy finding a clonal lambda-restricted plasma cell population.
With worsening renal and liver injury, he urgently started daratumumab, bortezomib, and dexamethasone, and hemodialysis. However, he developed progressive multisystem organ failure with refractory ascites, hepatic encephalopathy, and distributive shock. He was transitioned to comfort care and soon expired.
Discussion: Infiltrative liver diseases are known to cause cholestatic liver disease but uncommonly cause liver failure, most observed from overwhelming infiltrative metastatic solid malignancy. LCDD is uncommon and is not expected to affect the liver fulminantly, as was observed in this patient. Recognition of uncommon etiologies of liver infiltrative diseases, such as malignancy, hemophagocytic lymphohistiocytosis, disseminated infections, and amyloidosis, can lead to timely recognition and treatment initiation, where early treatment may affect patient survival.
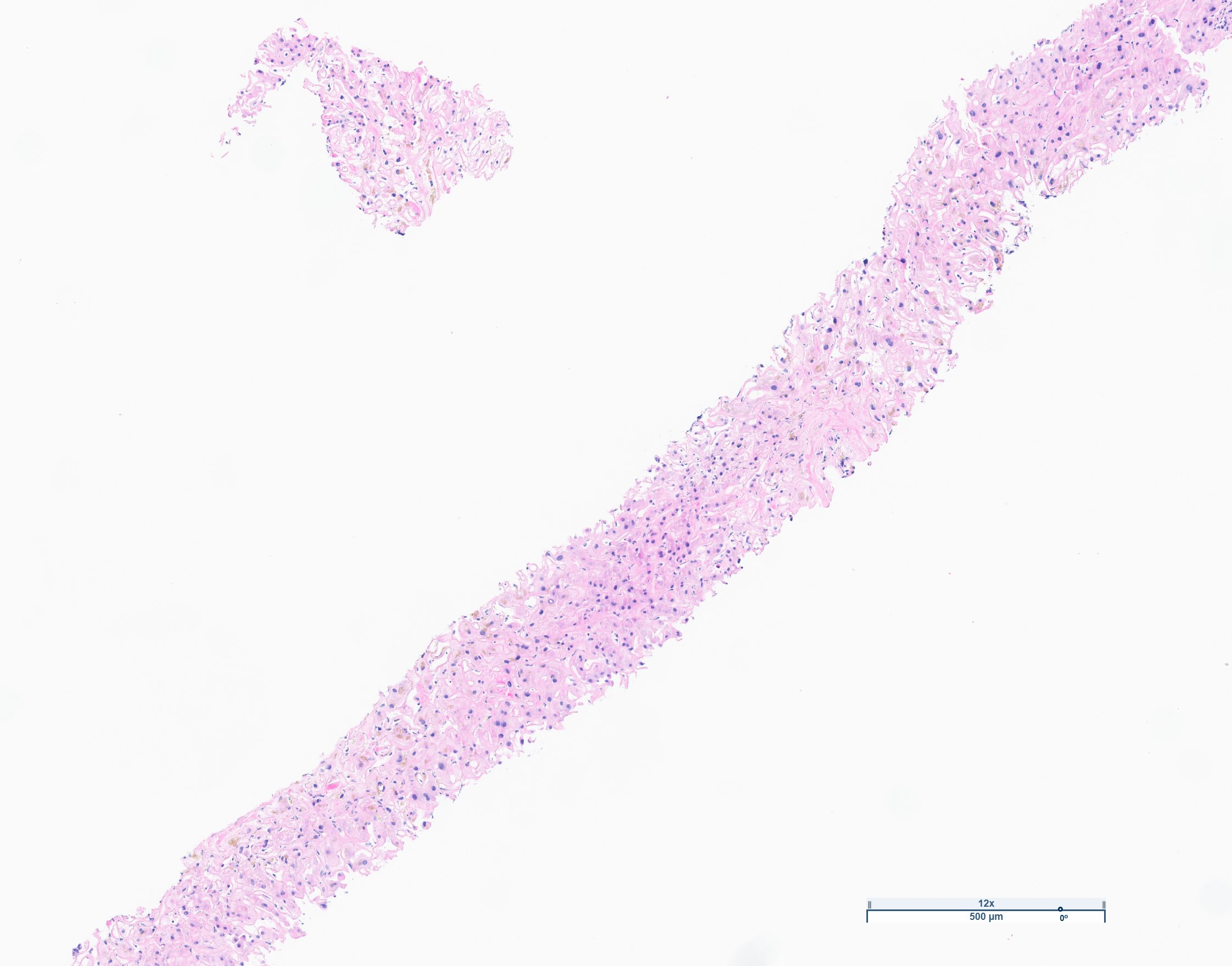
Figure: A) H&E: Diffuse and prominent perisinusoidal fibrosis, which also involves the pericentral liver parenchyma. No hepatocyte dropout, atrophy or nodularity was identified.
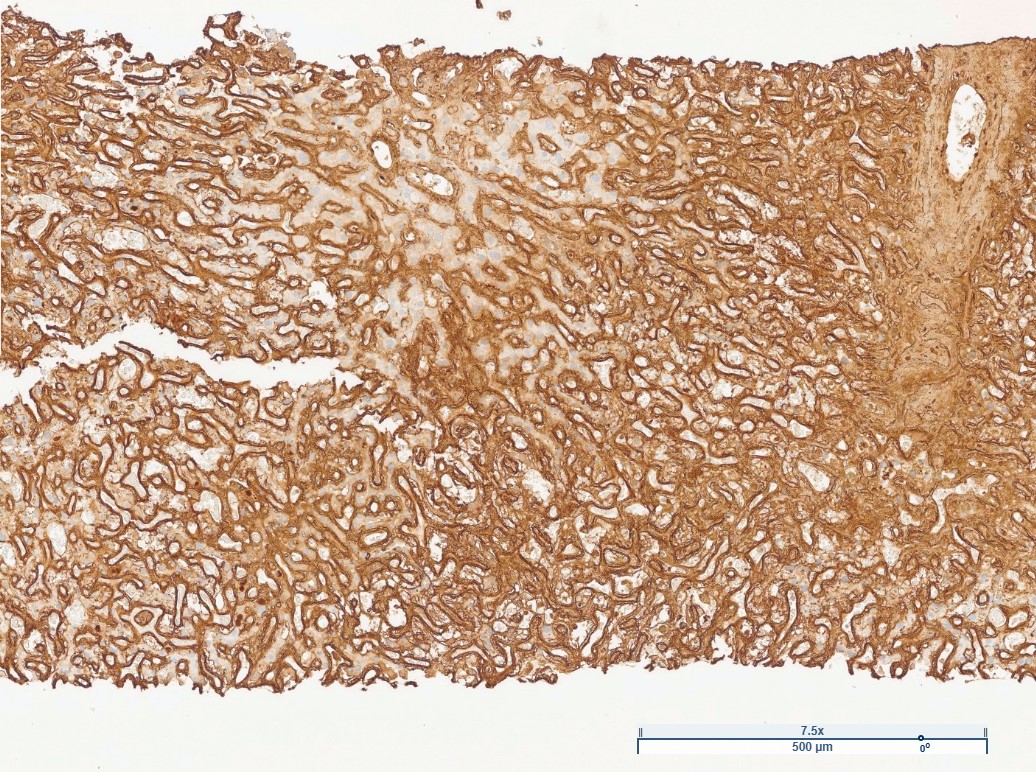
Figure: B) Lambda light chain, strong staining of sinusoidal and perivenular acellular material.
Disclosures:
Feruza Abraamyan indicated no relevant financial relationships.
Albert Do indicated no relevant financial relationships.
Feruza Abraamyan, MD1, Albert Do, MD2. P1744 - Light Chain Deposition Disease Manifesting as Acute Liver Failure, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
