Sunday Poster Session
Category: Liver
P1743 - A Diagnosis in Disguise: Asymptomatic Pseudomyxoma Peritonei Mimicking Cirrhosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Priscila Olague, MD
Univeristy of Texas Health Sciences Center in Houston
Houston, TX
Presenting Author(s)
Sean Ngo, BS1, Priscila Olague, MD2, Clay Smithhart, MD3, Tugrul Purnak, MD4
1McGovern Medical School at UTHealth, Houston, TX; 2Univeristy of Texas Health Sciences Center in Houston, Houston, TX; 3University of Texas Health, McGovern Medical School, Houston, TX; 4University of Texas at Houston, Houston, TX
Introduction: Pseudomyxoma peritonei (PMP) is a rare intra-abdominal malignancy characterized by mucinous ascites. Patients frequently present with non-specific abdominal symptoms, but in this case, the patient was asymptomatic and initially referred to the hepatology clinic for suspected cirrhosis. The patient’s concurrent cardiac comorbidities required a multidisciplinary approach to balance his overall health with his oncologic treatment.
Case Description/
Methods: A 54-year-old man with severe mitral regurgitation presented to the cardiovascular surgery clinic for mitral valve repair evaluation. A preoperative abdominal CT incidentally revealed a shrunken, irregular liver with ascites (Figure 1), raising concerns for cirrhosis and prompting a hepatology referral. However, a subsequent liver ultrasound revealed a complex perihepatic fluid collection, warranting further investigation.
The patient, who was asymptomatic with normal liver function tests, underwent MRI, which revealed liver scalloping and a heterogeneous, septated peritoneal fluid collection suggestive of PMP (Figure 2). Paracentesis confirmed the presence of intra-abdominal gelatinous fluid, and elevated tumor markers (CEA of 31 ng/mL, CA19-9 of 1,318 U/mL) supported the diagnosis of malignancy. Biopsy of a newly detected abdominal wall mass confirmed a well-differentiated mucinous adenocarcinoma, leading to a diagnosis of Stage IV PMP.
Due to the severity of the patient’s mitral regurgitation, the care team proceeded with mitral valve repair before pursuing oncologic intervention. Only after successful cardiac surgery and rehabilitation did the patient undergo PMP treatment with cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) nine months post-diagnosis. Follow-up imaging at six months and one year showed stable disease.
Discussion: Overall, PMP is rare and requires a high degree of suspicion in patients presenting with complex ascites. In this case, pseudocirrhosis due to peritoneal disease mimicked true cirrhosis, but liver scalloping and preserved liver function were key distinguishing features. Furthermore, while CRS/HIPEC is typically performed within three months of PMP diagnosis, this patient’s treatment was delayed for cardiac surgery, demonstrating that, in select cases, deferring CRS/HIPEC can be a viable strategy to optimize patient outcomes while managing coexisting medical conditions.
Disclosure: AI software was used to assist with grammar and spelling during the preparation of this abstract.
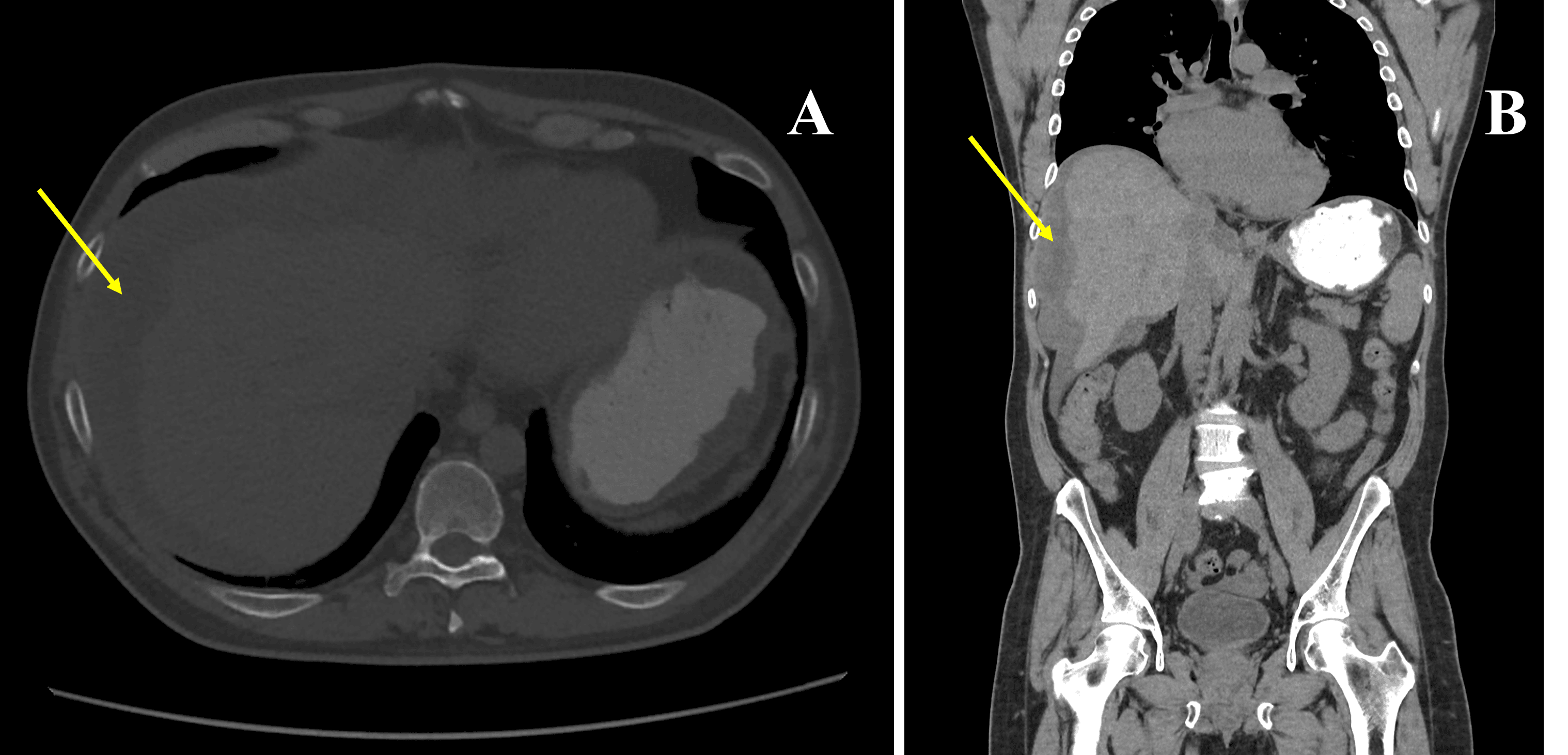
Figure: CT Abdomen and Pelvis without contrast. Initial axial (A) and coronal (B) views with incidental findings of a small, shrunken and irregular liver with surrounding fluid (denoted by yellow arrows) misattributed to liver cirrhosis and simple ascites.
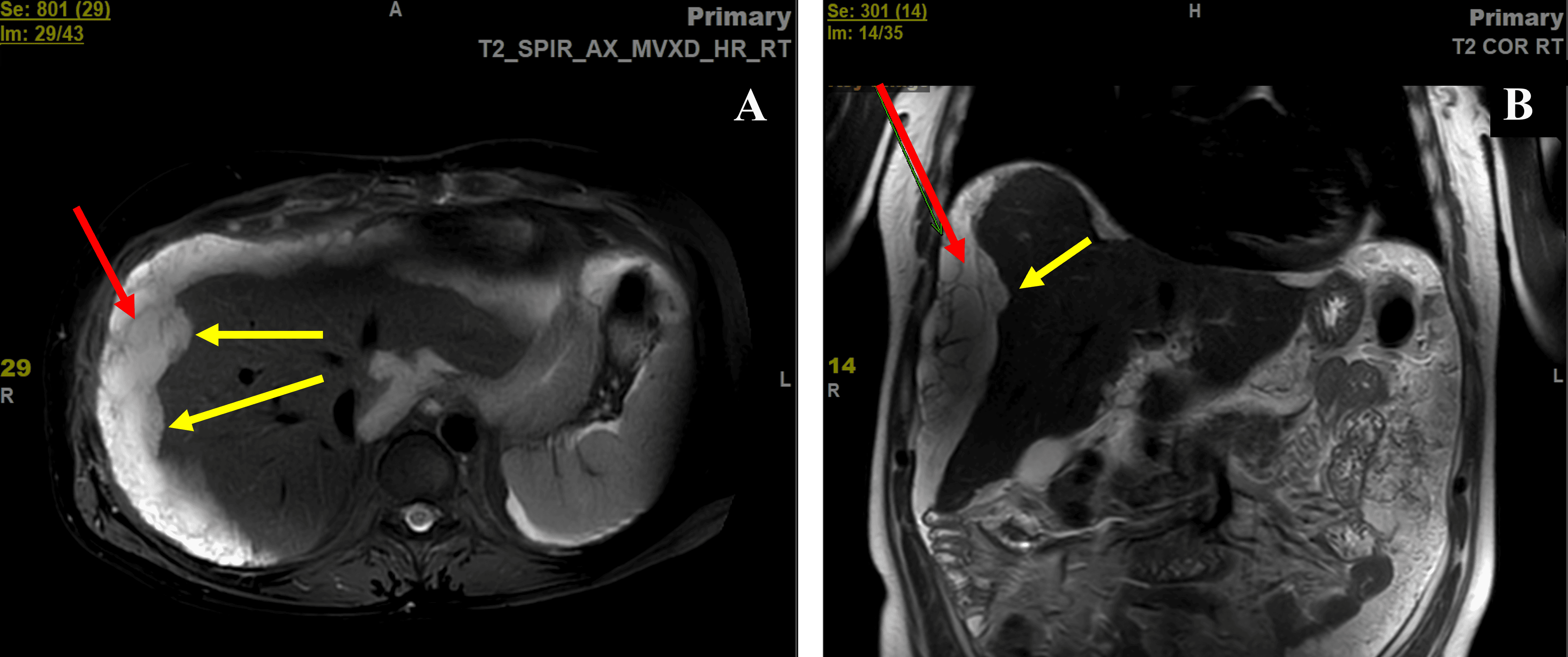
Figure: MRI of the abdomen with contrast. Axial (A) and coronal (B) views of the liver revealing scalloping of the liver (denoted by yellow arrows) and a complex septated perihepatic fluid collection causing a pseudocirrhotic liver morphology (denoted by red arrows).
Disclosures:
Sean Ngo indicated no relevant financial relationships.
Priscila Olague indicated no relevant financial relationships.
Clay Smithhart indicated no relevant financial relationships.
Tugrul Purnak indicated no relevant financial relationships.
Sean Ngo, BS1, Priscila Olague, MD2, Clay Smithhart, MD3, Tugrul Purnak, MD4. P1743 - A Diagnosis in Disguise: Asymptomatic Pseudomyxoma Peritonei Mimicking Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1McGovern Medical School at UTHealth, Houston, TX; 2Univeristy of Texas Health Sciences Center in Houston, Houston, TX; 3University of Texas Health, McGovern Medical School, Houston, TX; 4University of Texas at Houston, Houston, TX
Introduction: Pseudomyxoma peritonei (PMP) is a rare intra-abdominal malignancy characterized by mucinous ascites. Patients frequently present with non-specific abdominal symptoms, but in this case, the patient was asymptomatic and initially referred to the hepatology clinic for suspected cirrhosis. The patient’s concurrent cardiac comorbidities required a multidisciplinary approach to balance his overall health with his oncologic treatment.
Case Description/
Methods: A 54-year-old man with severe mitral regurgitation presented to the cardiovascular surgery clinic for mitral valve repair evaluation. A preoperative abdominal CT incidentally revealed a shrunken, irregular liver with ascites (Figure 1), raising concerns for cirrhosis and prompting a hepatology referral. However, a subsequent liver ultrasound revealed a complex perihepatic fluid collection, warranting further investigation.
The patient, who was asymptomatic with normal liver function tests, underwent MRI, which revealed liver scalloping and a heterogeneous, septated peritoneal fluid collection suggestive of PMP (Figure 2). Paracentesis confirmed the presence of intra-abdominal gelatinous fluid, and elevated tumor markers (CEA of 31 ng/mL, CA19-9 of 1,318 U/mL) supported the diagnosis of malignancy. Biopsy of a newly detected abdominal wall mass confirmed a well-differentiated mucinous adenocarcinoma, leading to a diagnosis of Stage IV PMP.
Due to the severity of the patient’s mitral regurgitation, the care team proceeded with mitral valve repair before pursuing oncologic intervention. Only after successful cardiac surgery and rehabilitation did the patient undergo PMP treatment with cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) nine months post-diagnosis. Follow-up imaging at six months and one year showed stable disease.
Discussion: Overall, PMP is rare and requires a high degree of suspicion in patients presenting with complex ascites. In this case, pseudocirrhosis due to peritoneal disease mimicked true cirrhosis, but liver scalloping and preserved liver function were key distinguishing features. Furthermore, while CRS/HIPEC is typically performed within three months of PMP diagnosis, this patient’s treatment was delayed for cardiac surgery, demonstrating that, in select cases, deferring CRS/HIPEC can be a viable strategy to optimize patient outcomes while managing coexisting medical conditions.
Disclosure: AI software was used to assist with grammar and spelling during the preparation of this abstract.
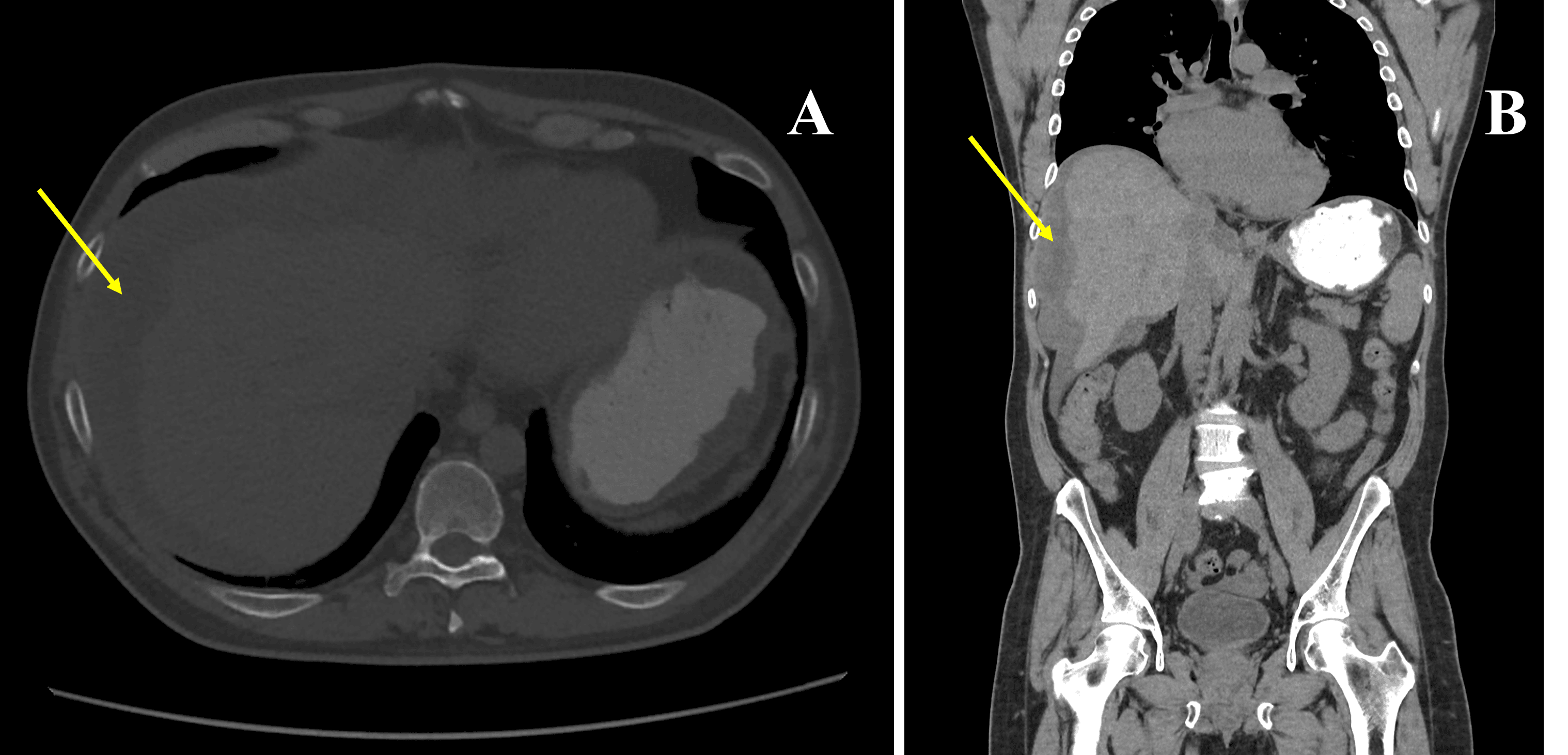
Figure: CT Abdomen and Pelvis without contrast. Initial axial (A) and coronal (B) views with incidental findings of a small, shrunken and irregular liver with surrounding fluid (denoted by yellow arrows) misattributed to liver cirrhosis and simple ascites.
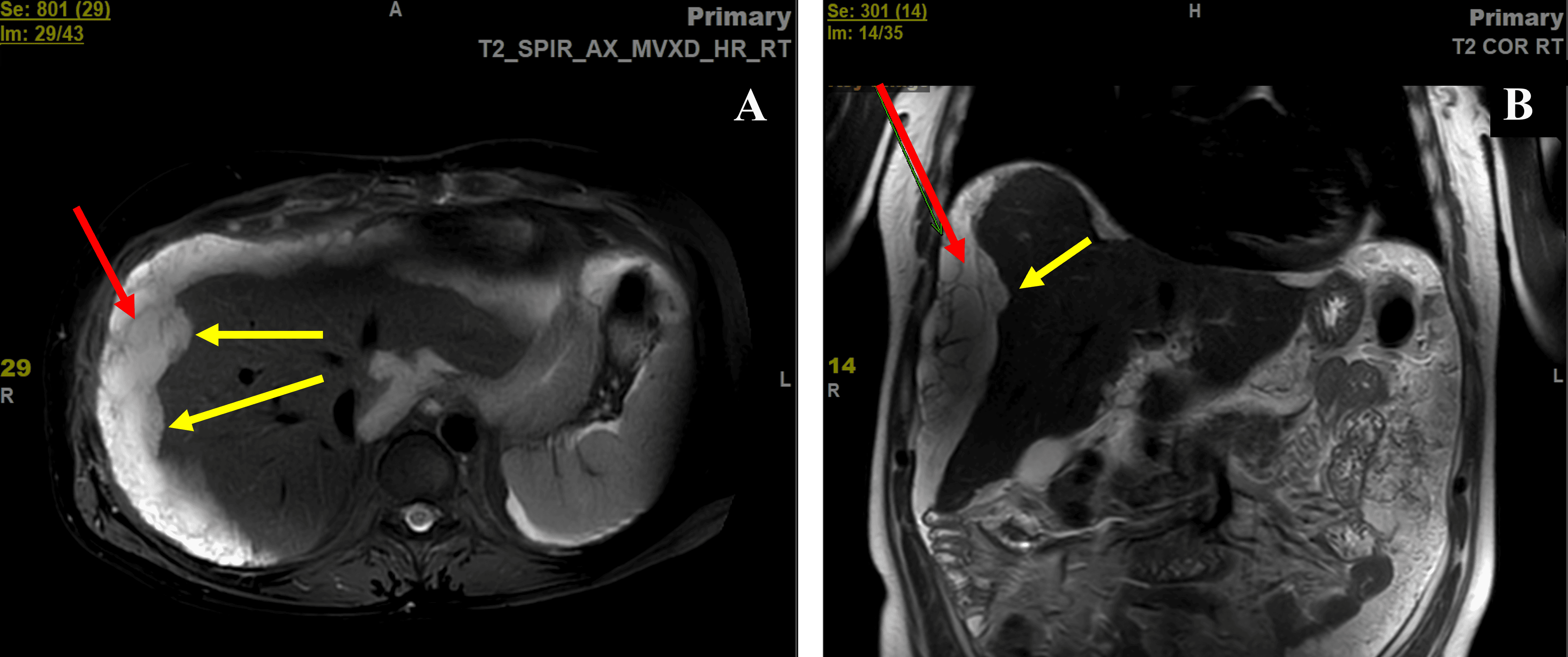
Figure: MRI of the abdomen with contrast. Axial (A) and coronal (B) views of the liver revealing scalloping of the liver (denoted by yellow arrows) and a complex septated perihepatic fluid collection causing a pseudocirrhotic liver morphology (denoted by red arrows).
Disclosures:
Sean Ngo indicated no relevant financial relationships.
Priscila Olague indicated no relevant financial relationships.
Clay Smithhart indicated no relevant financial relationships.
Tugrul Purnak indicated no relevant financial relationships.
Sean Ngo, BS1, Priscila Olague, MD2, Clay Smithhart, MD3, Tugrul Purnak, MD4. P1743 - A Diagnosis in Disguise: Asymptomatic Pseudomyxoma Peritonei Mimicking Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
