Sunday Poster Session
Category: Liver
P1742 - Hepatic Infarction Due to Preeclampsia With Severe Features
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Sarah Huang, MD
Brown University / Women and Infants Hospital
Providence, RI
Presenting Author(s)
Sarah Huang, MD1, Victoria Angenent-Mari, 2, Nnenna Okpara, MD1, Mariam Fayek, MD1
1Brown University / Women and Infants Hospital, Providence, RI; 2Brown University / Warren Alpert Medical School, Providence, RI
Introduction: Hepatic infarction is a rare complication of preeclampsia with an estimated incidence at 1 in 67,000 births or occurring in 1 in 2,000 individuals with preeclampsia. More recent literature reports unclear true incidence of hepatic infarction due to HELLP due to the limited number of published cases. We present a case of hepatic infarction in the setting of preeclampsia with severe features by hepatic dysfunction.
Case Description/
Methods: A 37 year old G2P0111 female presented to the hospital at 33 weeks gestation with new onset hypertension, blurry vision, and lightheadedness. Induction of labor was begun given presentation concerning for preeclampsia. She presented with normal labs, but she acutely developed right upper quadrant pain and acute transaminases; therefore she underwent an emergent C-section for concern for preeclampsia with severe features by hepatic dysfunction. Labs were as follows: ALT 477 IU/L, AST 526 IU/L, ALP 192 IU/L, normal bilirubin, INR, and albumin. Acute hepatitis panels were non reactive. LDH was elevated to 807 IU/L. Haptoglobin was low at 21 mg/dL. Platelets lowest was at 105,000 per microliter. She did not have anemia.
Contrast enhanced CT abdomen and pelvis (Figure 1) revealed multiple peripheral regions of wedge-shaped hypoattenuation in the right hepatic lobe, concerning for hepatic infarction. No biliary dilatation or gallstones were seen. Following delivery, her blood pressure and liver enzymes steadily improved. Her care was managed in a multidisciplinary fashion between Maternal Fetal Medicine and Gastroenterology. She was educated to be aware of the risk of pyogenic superinfection and hepatic rupture. Supportive care and close followup was provided with near resolution in the hepatic infarction on interval CT scan with three phase liver protocol a month later.
Discussion: Early recognition and diagnosis of hepatic infarction is essential to prevent fulminant liver failure and death, which can occur in 16% of cases. The extent of hepatic infarction may be massive, necessitate ICU level of care, and life saving surgical interventions such as hepatic resection or liver transplantation. Treatment involves addressing the underlying cause of the disruption in blood flow. Therapeutic anticoagulation may be considered to prevent further thrombus formation. Patients with hepatic infarction should also be monitored for symptoms concerning pyogenic superinfection. Patients who are asymptomatic may be managed supportively with serial cross sectional imaging.
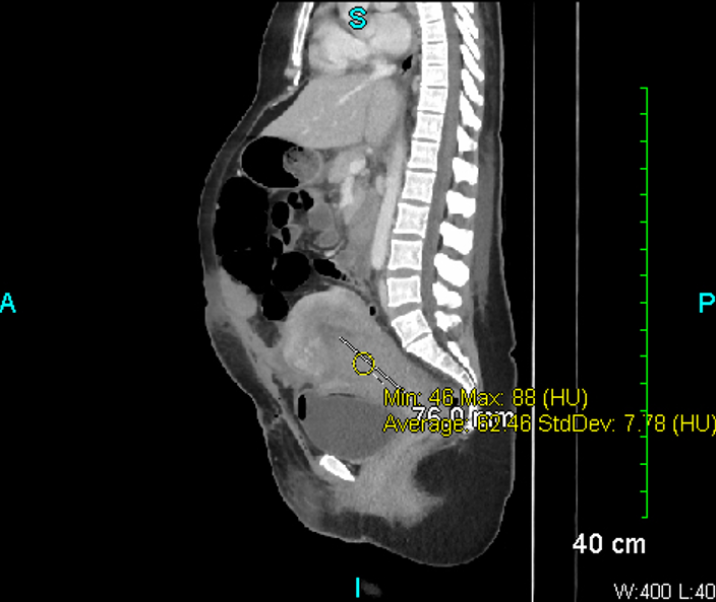
Figure: Computed tomography scan demonstrating multiple peripheral regions of wedge-shaped hypoattenuation in the right hepatic lobe, concerning for hepatic infarcts.
Disclosures:
Sarah Huang indicated no relevant financial relationships.
Victoria Angenent-Mari indicated no relevant financial relationships.
Nnenna Okpara indicated no relevant financial relationships.
Mariam Fayek indicated no relevant financial relationships.
Sarah Huang, MD1, Victoria Angenent-Mari, 2, Nnenna Okpara, MD1, Mariam Fayek, MD1. P1742 - Hepatic Infarction Due to Preeclampsia With Severe Features, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Brown University / Women and Infants Hospital, Providence, RI; 2Brown University / Warren Alpert Medical School, Providence, RI
Introduction: Hepatic infarction is a rare complication of preeclampsia with an estimated incidence at 1 in 67,000 births or occurring in 1 in 2,000 individuals with preeclampsia. More recent literature reports unclear true incidence of hepatic infarction due to HELLP due to the limited number of published cases. We present a case of hepatic infarction in the setting of preeclampsia with severe features by hepatic dysfunction.
Case Description/
Methods: A 37 year old G2P0111 female presented to the hospital at 33 weeks gestation with new onset hypertension, blurry vision, and lightheadedness. Induction of labor was begun given presentation concerning for preeclampsia. She presented with normal labs, but she acutely developed right upper quadrant pain and acute transaminases; therefore she underwent an emergent C-section for concern for preeclampsia with severe features by hepatic dysfunction. Labs were as follows: ALT 477 IU/L, AST 526 IU/L, ALP 192 IU/L, normal bilirubin, INR, and albumin. Acute hepatitis panels were non reactive. LDH was elevated to 807 IU/L. Haptoglobin was low at 21 mg/dL. Platelets lowest was at 105,000 per microliter. She did not have anemia.
Contrast enhanced CT abdomen and pelvis (Figure 1) revealed multiple peripheral regions of wedge-shaped hypoattenuation in the right hepatic lobe, concerning for hepatic infarction. No biliary dilatation or gallstones were seen. Following delivery, her blood pressure and liver enzymes steadily improved. Her care was managed in a multidisciplinary fashion between Maternal Fetal Medicine and Gastroenterology. She was educated to be aware of the risk of pyogenic superinfection and hepatic rupture. Supportive care and close followup was provided with near resolution in the hepatic infarction on interval CT scan with three phase liver protocol a month later.
Discussion: Early recognition and diagnosis of hepatic infarction is essential to prevent fulminant liver failure and death, which can occur in 16% of cases. The extent of hepatic infarction may be massive, necessitate ICU level of care, and life saving surgical interventions such as hepatic resection or liver transplantation. Treatment involves addressing the underlying cause of the disruption in blood flow. Therapeutic anticoagulation may be considered to prevent further thrombus formation. Patients with hepatic infarction should also be monitored for symptoms concerning pyogenic superinfection. Patients who are asymptomatic may be managed supportively with serial cross sectional imaging.
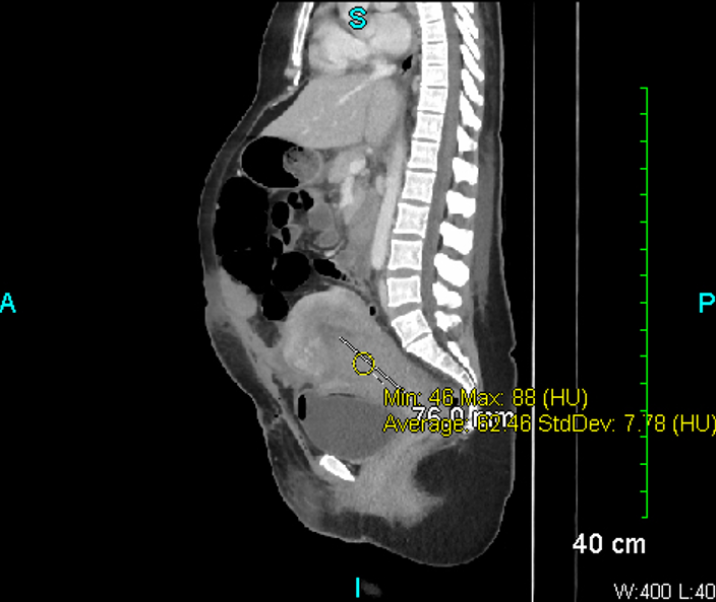
Figure: Computed tomography scan demonstrating multiple peripheral regions of wedge-shaped hypoattenuation in the right hepatic lobe, concerning for hepatic infarcts.
Disclosures:
Sarah Huang indicated no relevant financial relationships.
Victoria Angenent-Mari indicated no relevant financial relationships.
Nnenna Okpara indicated no relevant financial relationships.
Mariam Fayek indicated no relevant financial relationships.
Sarah Huang, MD1, Victoria Angenent-Mari, 2, Nnenna Okpara, MD1, Mariam Fayek, MD1. P1742 - Hepatic Infarction Due to Preeclampsia With Severe Features, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
