Sunday Poster Session
Category: Liver
P1739 - Rapidly Progressing Biliary Cystadenoma in a Young Patient: A Case Report
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- AK
Abdelrahman Khater, MD
UCSF Fresno
Fresno, CA
Presenting Author(s)
Abdelrahman Khater, MD1, Sindhu Chadalawada, MD1, Amir Fathi, MD1, Marina Roytman, MD2
1UCSF Fresno, Fresno, CA; 2Hepatology Fellowship, UCSF Fresno, Fresno, CA
Introduction: Biliary cystadenomas make up < 5% of all hepatic cysts. These pre-malignant lesions have a 10-30% lifetime risk of transformation to cystadenocarcinoma. They are typically incidental findings and present with nonspecific symptoms such as abdominal pain, fullness, or jaundice.
Case Description/
Methods: A 23-year-old woman with history of complex hepatic cyst noted in June 2024 presented with stabbing, subacute on chronic right upper quadrant (RUQ) abdominal pain and unintentional 20 lbs. weight loss in December 2024. She had associated post prandial non-bilious, non-bloody emesis. Social history noted travel to Mexico earlier in the year with accommodations in a jungle resort. Physical exam revealed tenderness to palpation in RUQ and epigastrium. Single phase contrast tomography (CT) revealed an enlarging 10.5 cm x 12 cm x 15.8 cm complex cystic lesion with multiple septations in the inferior hepatic margin and hepatic hilum. Subsequent multiphase magnetic resonance imaging (MRI) re-demonstrated a partially exophytic 11.6 cm x 16.8 cm multiloculated cystic mass in hepatic segments IV, V, and VIII with internal septation, blood products, and perilesional perfusion alteration. Enzyme immunoassay for echinococcus antibodies was negative. Laparoscopic partial cyst resection was performed, and pathology confirmed biliary cystadenoma with a single layer of bland mucinous columnar lining epithelium without proliferation or significant cellular atypia. The cyst wall was comprised of cellular ovarian-type stroma, confirmed by stromal cell nuclear positivity for estrogen and progesterone receptors.
Discussion: Due to the risk of malignant transformation of biliary cystadenomas, resection and surveillance are the mainstay of treatment. Enucleation is an option for centrally located cysts or those risking significant parenchymal loss. In this case, the cyst occupied most of the central and left liver, making complete resection of the cyst challenging. The presence of ovarian-type stroma is considered a good prognostic factor. Following multidisciplinary discussion, a decision was made to pursue reoperation to resect the majority of cyst and ablate the remaining epithelial lining that resides on critical central liver structures such as portal vein and biliary bifurcation. This case highlights the importance of timely evaluation of biliary cystadenomas, which are frequently identified incidentally. Particular attention is warranted in young age, rapid growth, given its potential for malignant transformation.
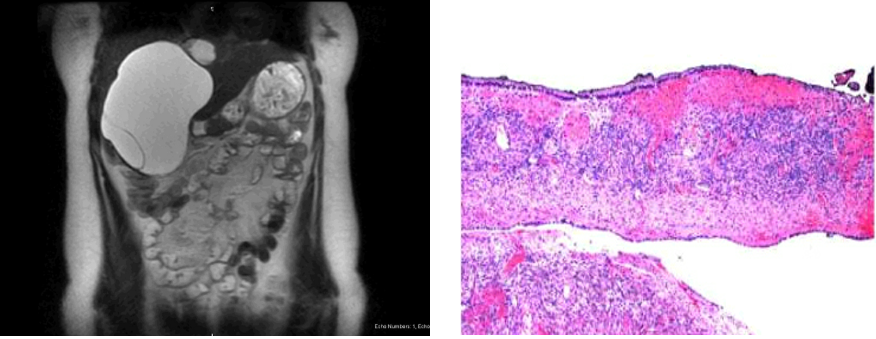
Figure: Figure 1A. Coronal MRI section of cystadenoma prior to resection.
Figure 1B. Biliary cystadenoma with ovarian-type stroma in cyst wall.
Disclosures:
Abdelrahman Khater indicated no relevant financial relationships.
Sindhu Chadalawada indicated no relevant financial relationships.
Amir Fathi indicated no relevant financial relationships.
Marina Roytman: Gilead – Speakers Bureau. Ipsen – Advisory Committee/Board Member. Madrigal – Speakers Bureau. Salix – Speakers Bureau.
Abdelrahman Khater, MD1, Sindhu Chadalawada, MD1, Amir Fathi, MD1, Marina Roytman, MD2. P1739 - Rapidly Progressing Biliary Cystadenoma in a Young Patient: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1UCSF Fresno, Fresno, CA; 2Hepatology Fellowship, UCSF Fresno, Fresno, CA
Introduction: Biliary cystadenomas make up < 5% of all hepatic cysts. These pre-malignant lesions have a 10-30% lifetime risk of transformation to cystadenocarcinoma. They are typically incidental findings and present with nonspecific symptoms such as abdominal pain, fullness, or jaundice.
Case Description/
Methods: A 23-year-old woman with history of complex hepatic cyst noted in June 2024 presented with stabbing, subacute on chronic right upper quadrant (RUQ) abdominal pain and unintentional 20 lbs. weight loss in December 2024. She had associated post prandial non-bilious, non-bloody emesis. Social history noted travel to Mexico earlier in the year with accommodations in a jungle resort. Physical exam revealed tenderness to palpation in RUQ and epigastrium. Single phase contrast tomography (CT) revealed an enlarging 10.5 cm x 12 cm x 15.8 cm complex cystic lesion with multiple septations in the inferior hepatic margin and hepatic hilum. Subsequent multiphase magnetic resonance imaging (MRI) re-demonstrated a partially exophytic 11.6 cm x 16.8 cm multiloculated cystic mass in hepatic segments IV, V, and VIII with internal septation, blood products, and perilesional perfusion alteration. Enzyme immunoassay for echinococcus antibodies was negative. Laparoscopic partial cyst resection was performed, and pathology confirmed biliary cystadenoma with a single layer of bland mucinous columnar lining epithelium without proliferation or significant cellular atypia. The cyst wall was comprised of cellular ovarian-type stroma, confirmed by stromal cell nuclear positivity for estrogen and progesterone receptors.
Discussion: Due to the risk of malignant transformation of biliary cystadenomas, resection and surveillance are the mainstay of treatment. Enucleation is an option for centrally located cysts or those risking significant parenchymal loss. In this case, the cyst occupied most of the central and left liver, making complete resection of the cyst challenging. The presence of ovarian-type stroma is considered a good prognostic factor. Following multidisciplinary discussion, a decision was made to pursue reoperation to resect the majority of cyst and ablate the remaining epithelial lining that resides on critical central liver structures such as portal vein and biliary bifurcation. This case highlights the importance of timely evaluation of biliary cystadenomas, which are frequently identified incidentally. Particular attention is warranted in young age, rapid growth, given its potential for malignant transformation.
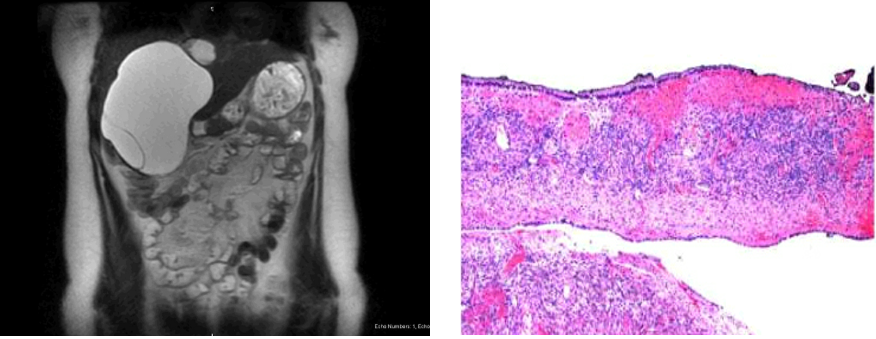
Figure: Figure 1A. Coronal MRI section of cystadenoma prior to resection.
Figure 1B. Biliary cystadenoma with ovarian-type stroma in cyst wall.
Disclosures:
Abdelrahman Khater indicated no relevant financial relationships.
Sindhu Chadalawada indicated no relevant financial relationships.
Amir Fathi indicated no relevant financial relationships.
Marina Roytman: Gilead – Speakers Bureau. Ipsen – Advisory Committee/Board Member. Madrigal – Speakers Bureau. Salix – Speakers Bureau.
Abdelrahman Khater, MD1, Sindhu Chadalawada, MD1, Amir Fathi, MD1, Marina Roytman, MD2. P1739 - Rapidly Progressing Biliary Cystadenoma in a Young Patient: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

