Sunday Poster Session
Category: Liver
P1737 - A Storm of Clots: Unmasking Catastrophic Antiphospholipid Syndrome in a Case of Rapid Multi-Vessel Thrombosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Mohamed Abdelfattah, MD (he/him/his)
Howard University Hospital, Department of Medicine
Washington, DC
Presenting Author(s)
Mohamed Abdelfattah, MD1, Ahmed Attia, MD2, Rediet Atalay, MD1, Ahmed Ali, MD3
1Howard University Hospital, Department of Medicine, Washington, DC; 2Transplant Institute, Department of Surgery, George Washington University School of Medicine and Health Science, Washington, DC; 3Howard University Hospital, Department of Hematology/Oncology, Washington, DC
Introduction: Catastrophic Antiphospholipid Syndrome (CAPS) is a fatal variant of antiphospholipid syndrome occurring in 1% of APLS patients, characterized by the rapid onset of multiple thrombotic events leading to acute organ dysfunction. Patients with CAPS typically present with significant thrombosis across various vascular territories within a short time, often precipitated by factors such as surgery or infection. The presence of antiphospholipid antibodies, such as anticardiolipin antibodies, plays a crucial role in pathogenesis.
Case Description/
Methods: A 49-year-old male with a history of unprovoked left leg DVT presented with abdominal pain 7 days after stopping Eliquis. He had bilateral upper extremity swelling and black discoloration of the middle three toes of the left foot. Ultrasound showed extensive thrombosis: bilateral internal jugular and axillary veins, right basilic vein, nonocclusive left cephalic and femoral veins, and main portal vein thrombosis. He was admitted to the SICU and started on heparin. Lactate peaked at 14. Two exploratory laparotomies revealed necrotic small bowel requiring resection. Platelet count dropped to 6, raising concern for heparin-induced thrombocytopenia (HIT) so Argatroban drip was started. Although initial HIT antibodies were positive, thrombocytopenia was present before heparin, and serotonin release assays were negative which rose concern for CAPS so quadruple therapy with steroids, plasma exchange, aspirin, and Argatroban was initiated. Platelets rebounded to >300 over days. Repeat ultrasounds confirmed resolution of most thromboses except persistent portal vein thrombosis. Antiphospholipid panel revealed positive lupus anticoagulant in high titer. Surgical pathology confirmed microvascular thrombosis. Given the macrovascular and microvascular thrombosis, multi-organ involvement, and serologic evidence, the patient met all four criteria for CAPS. The patient was transitioned to weight-based enoxaparin with stable platelet counts.
Discussion: This case highlights the urgency and complexity of CAPS. The rapid development of multiple clots underscores the need for prompt diagnosis and treatment. Plasmapheresis played a key therapeutic role but initially caused false-negative antiphospholipid antibody results. However, testing 10 days after the final session helps confirm the CAPS diagnosis.
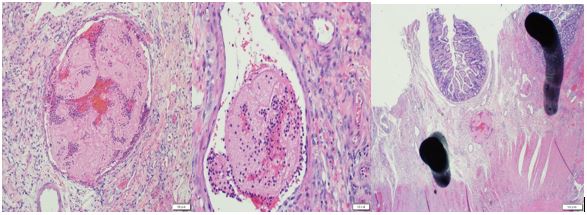
Figure: Surgical specimen pathologic findings show evidence of microvascular thrombosis.
Disclosures:
Mohamed Abdelfattah indicated no relevant financial relationships.
Ahmed Attia indicated no relevant financial relationships.
Rediet Atalay indicated no relevant financial relationships.
Ahmed Ali indicated no relevant financial relationships.
Mohamed Abdelfattah, MD1, Ahmed Attia, MD2, Rediet Atalay, MD1, Ahmed Ali, MD3. P1737 - A Storm of Clots: Unmasking Catastrophic Antiphospholipid Syndrome in a Case of Rapid Multi-Vessel Thrombosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Howard University Hospital, Department of Medicine, Washington, DC; 2Transplant Institute, Department of Surgery, George Washington University School of Medicine and Health Science, Washington, DC; 3Howard University Hospital, Department of Hematology/Oncology, Washington, DC
Introduction: Catastrophic Antiphospholipid Syndrome (CAPS) is a fatal variant of antiphospholipid syndrome occurring in 1% of APLS patients, characterized by the rapid onset of multiple thrombotic events leading to acute organ dysfunction. Patients with CAPS typically present with significant thrombosis across various vascular territories within a short time, often precipitated by factors such as surgery or infection. The presence of antiphospholipid antibodies, such as anticardiolipin antibodies, plays a crucial role in pathogenesis.
Case Description/
Methods: A 49-year-old male with a history of unprovoked left leg DVT presented with abdominal pain 7 days after stopping Eliquis. He had bilateral upper extremity swelling and black discoloration of the middle three toes of the left foot. Ultrasound showed extensive thrombosis: bilateral internal jugular and axillary veins, right basilic vein, nonocclusive left cephalic and femoral veins, and main portal vein thrombosis. He was admitted to the SICU and started on heparin. Lactate peaked at 14. Two exploratory laparotomies revealed necrotic small bowel requiring resection. Platelet count dropped to 6, raising concern for heparin-induced thrombocytopenia (HIT) so Argatroban drip was started. Although initial HIT antibodies were positive, thrombocytopenia was present before heparin, and serotonin release assays were negative which rose concern for CAPS so quadruple therapy with steroids, plasma exchange, aspirin, and Argatroban was initiated. Platelets rebounded to >300 over days. Repeat ultrasounds confirmed resolution of most thromboses except persistent portal vein thrombosis. Antiphospholipid panel revealed positive lupus anticoagulant in high titer. Surgical pathology confirmed microvascular thrombosis. Given the macrovascular and microvascular thrombosis, multi-organ involvement, and serologic evidence, the patient met all four criteria for CAPS. The patient was transitioned to weight-based enoxaparin with stable platelet counts.
Discussion: This case highlights the urgency and complexity of CAPS. The rapid development of multiple clots underscores the need for prompt diagnosis and treatment. Plasmapheresis played a key therapeutic role but initially caused false-negative antiphospholipid antibody results. However, testing 10 days after the final session helps confirm the CAPS diagnosis.
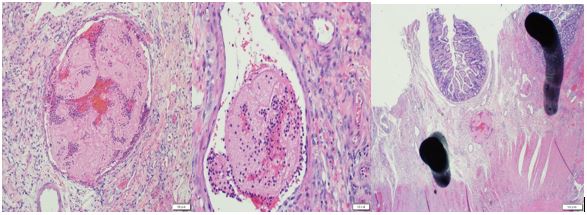
Figure: Surgical specimen pathologic findings show evidence of microvascular thrombosis.
Disclosures:
Mohamed Abdelfattah indicated no relevant financial relationships.
Ahmed Attia indicated no relevant financial relationships.
Rediet Atalay indicated no relevant financial relationships.
Ahmed Ali indicated no relevant financial relationships.
Mohamed Abdelfattah, MD1, Ahmed Attia, MD2, Rediet Atalay, MD1, Ahmed Ali, MD3. P1737 - A Storm of Clots: Unmasking Catastrophic Antiphospholipid Syndrome in a Case of Rapid Multi-Vessel Thrombosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
