Sunday Poster Session
Category: Liver
P1731 - Pembrolizumab-Induced Mixed Hepatocellular and Cholestatic Liver Injury: A Case Report
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Lan Nguyen, DO
University at Buffalo
Buffalo, NY
Presenting Author(s)
Lan Nguyen, DO1, Xavier Zonna, DO1, Edward Tamale, MD2, Ali Aijaz, DO2, Dzenita Manning, MD1
1University at Buffalo, Buffalo, NY; 2University of Buffalo Jacobs School of Medicine, Buffalo, NY
Introduction: Immune checkpoint inhibitors (ICIs) have revolutionized cancer therapy but are associated with immune-related adverse events, including hepatotoxicity. While most ICI-injuries liver injuries are either hepatocellular or cholestatic, mixed patterns are increasingly recognized and can complicate diagnosis and management. We present a case of pembrolizumab-induced mixed liver injury in a patient with metastatic lung cancer.
Case Description/
Methods: An 80-year-old woman with lung cancer metastatic to the brain and adrenal glands presented with jaundice, dark urine, and pale stools one month after initiating pembrolizumab. The patient was hemodynamically stable with physical exam notable for scleral icterus, jaundice, and non-tender non-distended abdomen. Laboratory studies showed elevated ALP 1118, AST 1146, ALT 1526, GGT 1200, total bilirubin 11.4. The calculated R factor was 4.09, indicating a mixed hepatocellular-cholestatic pattern. CT abdomen/pelvis revealed gallbladder wall thickening and mural hyperemia of the common bile duct without gallstones. ERCP demonstrated mild bile duct dilation of 8 mm without obstruction; stents were placed in the common bile and pancreatic ducts to exclude extrahepatic processes. Infectious, autoimmune, and metabolic workups were unremarkable. A mixed, cholestatic-predominant pattern of liver injury was therefore suspected. High-dose corticosteroids were initiated, followed by mycophenolate mofetil and ursodeoxycholic acid due to limited initial response. Liver function gradually improved with immunosuppressive therapy.
Discussion: ICI-induced mixed liver injury is underrecognized with overlapping features of hepatitis and cholangitis. While hepatitis often presents with fatigue or right upper quadrant discomfort and elevations in ALT/AST, cholangitis is associated with jaundice, increased ALP/GGT, and imaging evidence of biliary inflammation. Imaging should include abdominal ultrasound or CT to assess obstruction, with MRCP or ERCP offering detailed biliary evaluation. Biopsy may support diagnosis, although histological features are often nonspecific. Treatment is guided by the Common Terminology Criteria for Adverse Events, which stratifies hepatotoxicity by severity. Corticosteroids remain first-line therapy; in cholestatic or steroid-refractory cases, mycophenolate and adjunctive ursodiol are often necessary. As ICI use continues to grow, recognition of liver injury patterns is critical to optimize outcomes and maintain continuity of cancer therapy.
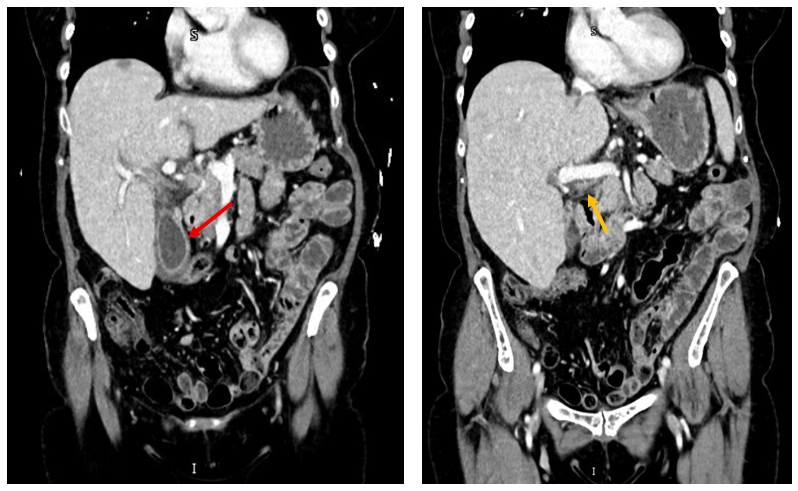
Figure: Figure 1. CT Abdomen and Pelvis: Coronal view showed gallbladder wall thickening (red arrow) with no cholelithiasis and mural hyperemia of common bile duct (orange arrow), suggesting cholangitis
Disclosures:
Lan Nguyen indicated no relevant financial relationships.
Xavier Zonna indicated no relevant financial relationships.
Edward Tamale indicated no relevant financial relationships.
Ali Aijaz indicated no relevant financial relationships.
Dzenita Manning indicated no relevant financial relationships.
Lan Nguyen, DO1, Xavier Zonna, DO1, Edward Tamale, MD2, Ali Aijaz, DO2, Dzenita Manning, MD1. P1731 - Pembrolizumab-Induced Mixed Hepatocellular and Cholestatic Liver Injury: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University at Buffalo, Buffalo, NY; 2University of Buffalo Jacobs School of Medicine, Buffalo, NY
Introduction: Immune checkpoint inhibitors (ICIs) have revolutionized cancer therapy but are associated with immune-related adverse events, including hepatotoxicity. While most ICI-injuries liver injuries are either hepatocellular or cholestatic, mixed patterns are increasingly recognized and can complicate diagnosis and management. We present a case of pembrolizumab-induced mixed liver injury in a patient with metastatic lung cancer.
Case Description/
Methods: An 80-year-old woman with lung cancer metastatic to the brain and adrenal glands presented with jaundice, dark urine, and pale stools one month after initiating pembrolizumab. The patient was hemodynamically stable with physical exam notable for scleral icterus, jaundice, and non-tender non-distended abdomen. Laboratory studies showed elevated ALP 1118, AST 1146, ALT 1526, GGT 1200, total bilirubin 11.4. The calculated R factor was 4.09, indicating a mixed hepatocellular-cholestatic pattern. CT abdomen/pelvis revealed gallbladder wall thickening and mural hyperemia of the common bile duct without gallstones. ERCP demonstrated mild bile duct dilation of 8 mm without obstruction; stents were placed in the common bile and pancreatic ducts to exclude extrahepatic processes. Infectious, autoimmune, and metabolic workups were unremarkable. A mixed, cholestatic-predominant pattern of liver injury was therefore suspected. High-dose corticosteroids were initiated, followed by mycophenolate mofetil and ursodeoxycholic acid due to limited initial response. Liver function gradually improved with immunosuppressive therapy.
Discussion: ICI-induced mixed liver injury is underrecognized with overlapping features of hepatitis and cholangitis. While hepatitis often presents with fatigue or right upper quadrant discomfort and elevations in ALT/AST, cholangitis is associated with jaundice, increased ALP/GGT, and imaging evidence of biliary inflammation. Imaging should include abdominal ultrasound or CT to assess obstruction, with MRCP or ERCP offering detailed biliary evaluation. Biopsy may support diagnosis, although histological features are often nonspecific. Treatment is guided by the Common Terminology Criteria for Adverse Events, which stratifies hepatotoxicity by severity. Corticosteroids remain first-line therapy; in cholestatic or steroid-refractory cases, mycophenolate and adjunctive ursodiol are often necessary. As ICI use continues to grow, recognition of liver injury patterns is critical to optimize outcomes and maintain continuity of cancer therapy.
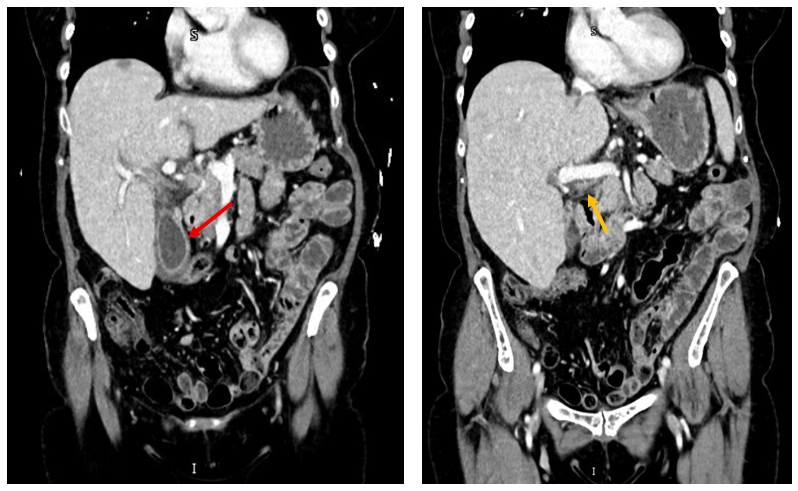
Figure: Figure 1. CT Abdomen and Pelvis: Coronal view showed gallbladder wall thickening (red arrow) with no cholelithiasis and mural hyperemia of common bile duct (orange arrow), suggesting cholangitis
Disclosures:
Lan Nguyen indicated no relevant financial relationships.
Xavier Zonna indicated no relevant financial relationships.
Edward Tamale indicated no relevant financial relationships.
Ali Aijaz indicated no relevant financial relationships.
Dzenita Manning indicated no relevant financial relationships.
Lan Nguyen, DO1, Xavier Zonna, DO1, Edward Tamale, MD2, Ali Aijaz, DO2, Dzenita Manning, MD1. P1731 - Pembrolizumab-Induced Mixed Hepatocellular and Cholestatic Liver Injury: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
