Sunday Poster Session
Category: Liver
P1726 - Seizing the Secret Shunt: A Congenital Portosystemic Shunt Disguised as Epilepsy
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- AM
Annabel Moore, MD
University of Kentucky
Lexington, KY
Presenting Author(s)
Annabel Moore, MD, Colton J. Hartig, MD, Jordan Woodard, MD, Nimish Thakral, MD, Ahmed Sobieh, MD
University of Kentucky, Lexington, KY
Introduction: Intrahepatic congenital portosystemic shunts (CPSS) are atypical vascular connections that allow blood to bypass the liver. Frequently, symptoms such as confusion and fatigue develop in childhood. Less often, patients remain asymptomatic as children but become symptomatic in adulthood. Currently, there are no evidence-based management guidelines in adults with these shunts. Experts recommend endovascular shunt closure in all adults, especially if symptoms are present.
Case Description/
Methods: A 61-year-old female with a medical history of constipation and obstructive sleep apnea presented with persistent left lower quadrant abdominal pain. A congenital intrahepatic portosystemic shunt was incidentally found on abdominal Doppler ultrasound. Computed tomography of the abdomen with intravenous contrast was obtained to better characterize anatomy and size of the shunt (figure 1). Liver function testing was within normal limits. The patient attested to episodic confusion and fatigue lasting minutes to hours during which she was not oriented to place or time. She developed these symptoms at 18 years old and was prescribed antiepileptic medications without improvement. Given the size of the shunt and her symptoms, closure of the shunt was conducted by interventional radiology with endovascular plug deployment. After the initial embolization, the patient’s symptoms improved but persisted. Imaging revealed persistent shunt and a second vascular plug procedure was performed with significant improvement in the patient’s symptoms (figure 2).
Discussion: Here we present a rare case of intrahepatic CPSS previously misdiagnosed as refractory epilepsy. Given that the episodic confusion failed to improve on anti-epileptic medication, the etiology was attributed to hepatic encephalopathy secondary to the shunt. In accordance with expert consensus, the patient’s shunt was closed via vascular plug deployment. Interestingly, a two-stage approach was required to fully close the shunt and resolve her symptoms.
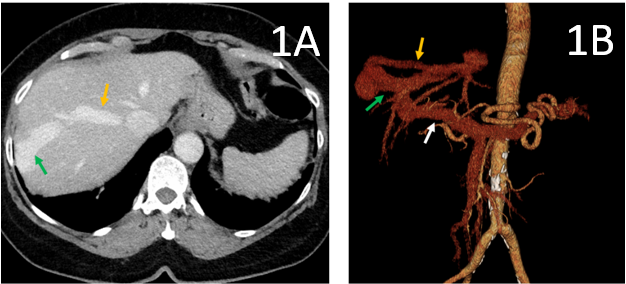
Figure: Figure 1. Transverse view of the original computed tomography scan of the liver with intravenous contrast (1A) and its corresponding three-dimensional reconstructed image (1B). A large vascular shunt (green arrow) is demonstrated connecting an enlarged right posterior portal vein branch (white arrow) and an enlarged segment 8 hepatic vein (orange arrow).
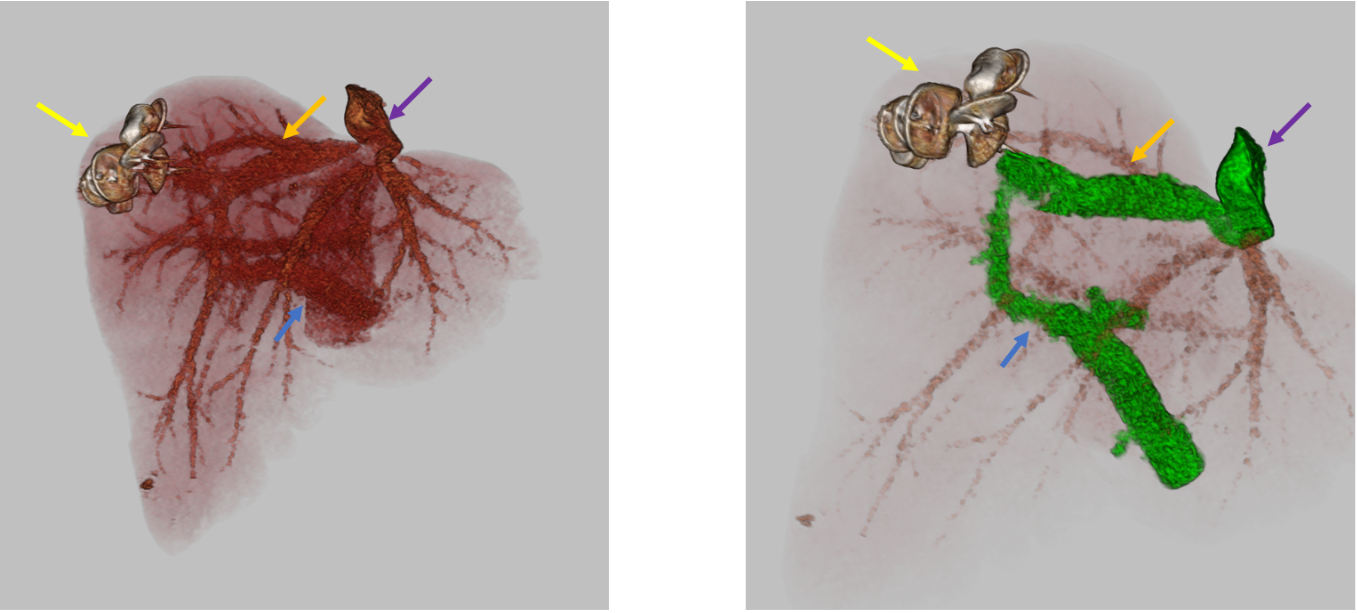
Figure: Figure 2. Three-dimensional reconstructions of the hepatic vasculature after final vascular plug deployment. Vascular plugs (yellow arrow) are demonstrated, in addition to the portal vein (blue arrow), right hepatic vein (orange arrow), and inferior vena cava (purple arrow).
Disclosures:
Annabel Moore indicated no relevant financial relationships.
Colton Hartig indicated no relevant financial relationships.
Jordan Woodard indicated no relevant financial relationships.
Nimish Thakral indicated no relevant financial relationships.
Ahmed Sobieh indicated no relevant financial relationships.
Annabel Moore, MD, Colton J. Hartig, MD, Jordan Woodard, MD, Nimish Thakral, MD, Ahmed Sobieh, MD. P1726 - Seizing the Secret Shunt: A Congenital Portosystemic Shunt Disguised as Epilepsy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Kentucky, Lexington, KY
Introduction: Intrahepatic congenital portosystemic shunts (CPSS) are atypical vascular connections that allow blood to bypass the liver. Frequently, symptoms such as confusion and fatigue develop in childhood. Less often, patients remain asymptomatic as children but become symptomatic in adulthood. Currently, there are no evidence-based management guidelines in adults with these shunts. Experts recommend endovascular shunt closure in all adults, especially if symptoms are present.
Case Description/
Methods: A 61-year-old female with a medical history of constipation and obstructive sleep apnea presented with persistent left lower quadrant abdominal pain. A congenital intrahepatic portosystemic shunt was incidentally found on abdominal Doppler ultrasound. Computed tomography of the abdomen with intravenous contrast was obtained to better characterize anatomy and size of the shunt (figure 1). Liver function testing was within normal limits. The patient attested to episodic confusion and fatigue lasting minutes to hours during which she was not oriented to place or time. She developed these symptoms at 18 years old and was prescribed antiepileptic medications without improvement. Given the size of the shunt and her symptoms, closure of the shunt was conducted by interventional radiology with endovascular plug deployment. After the initial embolization, the patient’s symptoms improved but persisted. Imaging revealed persistent shunt and a second vascular plug procedure was performed with significant improvement in the patient’s symptoms (figure 2).
Discussion: Here we present a rare case of intrahepatic CPSS previously misdiagnosed as refractory epilepsy. Given that the episodic confusion failed to improve on anti-epileptic medication, the etiology was attributed to hepatic encephalopathy secondary to the shunt. In accordance with expert consensus, the patient’s shunt was closed via vascular plug deployment. Interestingly, a two-stage approach was required to fully close the shunt and resolve her symptoms.
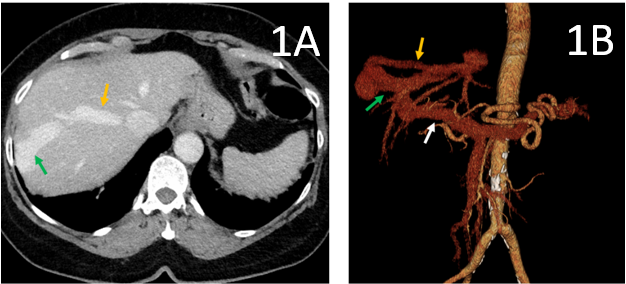
Figure: Figure 1. Transverse view of the original computed tomography scan of the liver with intravenous contrast (1A) and its corresponding three-dimensional reconstructed image (1B). A large vascular shunt (green arrow) is demonstrated connecting an enlarged right posterior portal vein branch (white arrow) and an enlarged segment 8 hepatic vein (orange arrow).
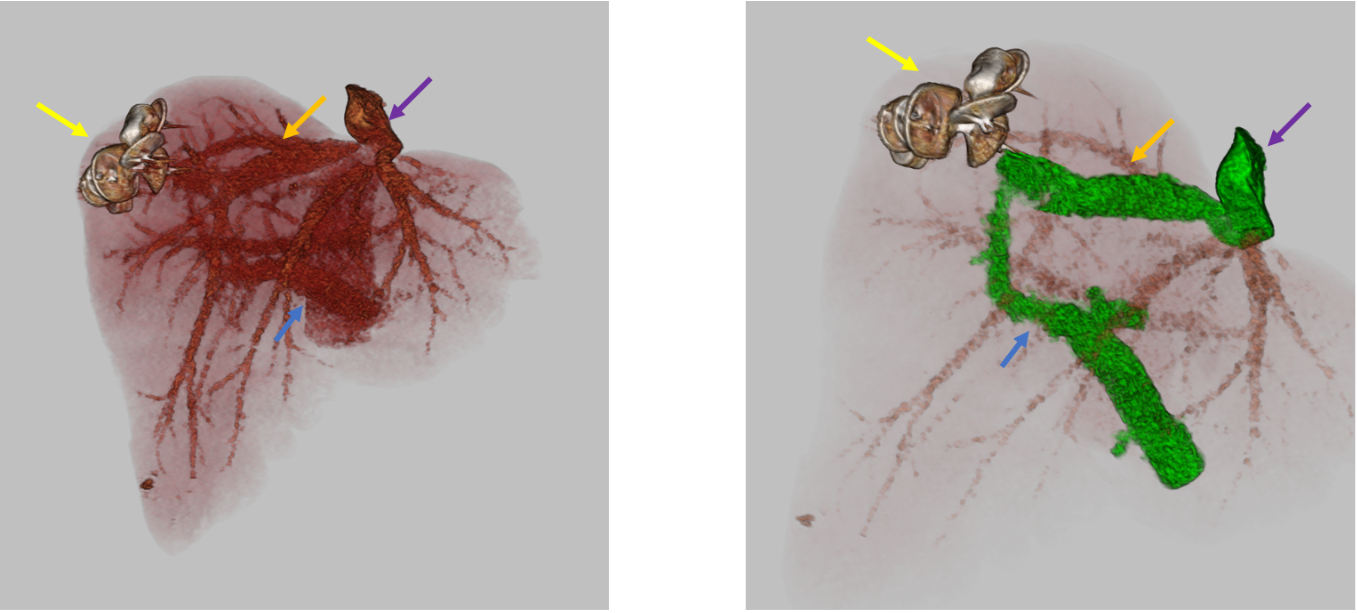
Figure: Figure 2. Three-dimensional reconstructions of the hepatic vasculature after final vascular plug deployment. Vascular plugs (yellow arrow) are demonstrated, in addition to the portal vein (blue arrow), right hepatic vein (orange arrow), and inferior vena cava (purple arrow).
Disclosures:
Annabel Moore indicated no relevant financial relationships.
Colton Hartig indicated no relevant financial relationships.
Jordan Woodard indicated no relevant financial relationships.
Nimish Thakral indicated no relevant financial relationships.
Ahmed Sobieh indicated no relevant financial relationships.
Annabel Moore, MD, Colton J. Hartig, MD, Jordan Woodard, MD, Nimish Thakral, MD, Ahmed Sobieh, MD. P1726 - Seizing the Secret Shunt: A Congenital Portosystemic Shunt Disguised as Epilepsy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
