Sunday Poster Session
Category: Liver
P1699 - The Double Burden: Unraveling the Complexity of Hepatic Sarcoidosis and MASLD in a Hispanic Patient
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Archit Garg, MD (he/him/his)
Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School
New Brunswick, NJ
Presenting Author(s)
Archit Garg, MD, Rajesh Desai, MD, Louisa Recinos-Arenas, MD
Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ
Introduction: Hepatic sarcoidosis occurs in 50–70% of sarcoidosis patients, often with asymptomatic or liver enzyme abnormalities. Metabolic dysfunction-associated steatotic liver disease (MASLD) is increasingly prevalent, particularly in Hispanic populations, yet coexisting hepatic sarcoidosis and MASLD remain unreported in this demographic. Hispanics exhibit higher MASLD prevalence and severity at lower BMIs, linked to PNPLA3 gene variants. Sarcoidosis-related inflammation may accelerate metabolic liver injury, complicating diagnosis and management.
Case Description/
Methods: A 30-year-old Hispanic female (BMI 23.4 kg/m²) with T2DM and hyperlipidemia presented with abdominal pain. CT revealed hepatomegaly with hepatic steatosis and an incidental lung nodule. Elevated liver enzymes (ALT 175 U/L, ALP 110 U/L) and ALP progression (peak 171 U/L) prompted further workup. Thoracic CT done for lung nodule showed mediastinal lymphadenopathy and bilateral nodules. Mediastinal lymph node biopsy confirmed sarcoidosis. Liver biopsy done due to persistent elevated ALP demonstrated both MASLD and hepatic sarcoidosis. Ursodiol was initiated, normalizing ALP within 3 months.
Discussion: This case represents the first documented coexistence of MASLD and hepatic sarcoidosis in a U.S. Hispanic patient, highlighting diagnostic and management complexities. The initial presentation with elevated liver enzymes and steatosis on imaging suggested MASLD, yet the elevated liver enzymes and concurrent pulmonary sarcoidosis prompted biopsy that revealed dual pathology: non-caseating granulomas alongside macrovesicular steatosis. Hispanics face unique risks, including 50% higher MASLD susceptibility (often at lower BMIs, potentially linked to PNPLA3 gene variants) and extrapulmonary sarcoidosis manifestations. The atypical ALP elevation signaled sarcoidosis-driven cholestasis, effectively managed with ursodiol, while MASLD required metabolic control. There can be a synergistic interaction with MASLD-related inflammation unmasking subclinical sarcoidosis, accelerating presentation, while sarcoidosis could exacerbate metabolic dysfunction (e.g., insulin dependence via potential pancreatic involvement). This dual etiology underscores the need for biopsy in Hispanic patients with metabolic risk factors and unexplained cholestasis, multidisciplinary monitoring to mitigate rapid progression risks, and awareness of genetic/environmental influences on disease phenotyping.
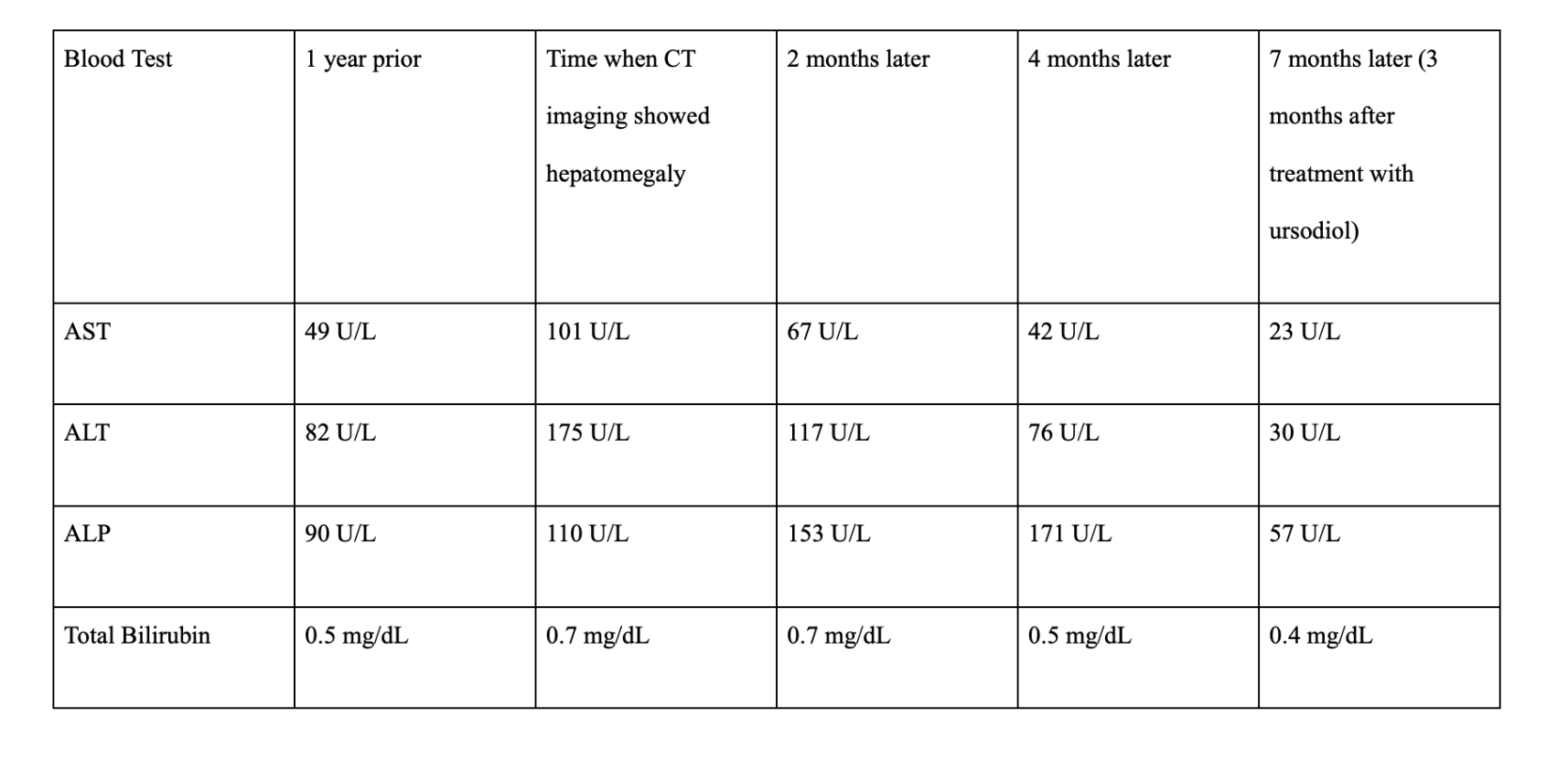
Figure: Table 1. Liver enzyme trends in the patient
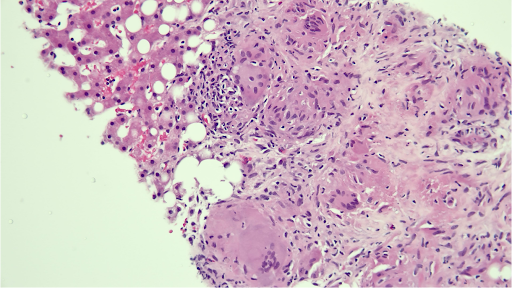
Figure: Figure 1: Liver core biopsy showed mild macrovesicular steatosis without ballooning degeneration of hepatocytes and a few portal tracts contain multiple coalescing epithelioid granulomas with fibrosis
Disclosures:
Archit Garg indicated no relevant financial relationships.
Rajesh Desai indicated no relevant financial relationships.
Louisa Recinos-Arenas indicated no relevant financial relationships.
Archit Garg, MD, Rajesh Desai, MD, Louisa Recinos-Arenas, MD. P1699 - The Double Burden: Unraveling the Complexity of Hepatic Sarcoidosis and MASLD in a Hispanic Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ
Introduction: Hepatic sarcoidosis occurs in 50–70% of sarcoidosis patients, often with asymptomatic or liver enzyme abnormalities. Metabolic dysfunction-associated steatotic liver disease (MASLD) is increasingly prevalent, particularly in Hispanic populations, yet coexisting hepatic sarcoidosis and MASLD remain unreported in this demographic. Hispanics exhibit higher MASLD prevalence and severity at lower BMIs, linked to PNPLA3 gene variants. Sarcoidosis-related inflammation may accelerate metabolic liver injury, complicating diagnosis and management.
Case Description/
Methods: A 30-year-old Hispanic female (BMI 23.4 kg/m²) with T2DM and hyperlipidemia presented with abdominal pain. CT revealed hepatomegaly with hepatic steatosis and an incidental lung nodule. Elevated liver enzymes (ALT 175 U/L, ALP 110 U/L) and ALP progression (peak 171 U/L) prompted further workup. Thoracic CT done for lung nodule showed mediastinal lymphadenopathy and bilateral nodules. Mediastinal lymph node biopsy confirmed sarcoidosis. Liver biopsy done due to persistent elevated ALP demonstrated both MASLD and hepatic sarcoidosis. Ursodiol was initiated, normalizing ALP within 3 months.
Discussion: This case represents the first documented coexistence of MASLD and hepatic sarcoidosis in a U.S. Hispanic patient, highlighting diagnostic and management complexities. The initial presentation with elevated liver enzymes and steatosis on imaging suggested MASLD, yet the elevated liver enzymes and concurrent pulmonary sarcoidosis prompted biopsy that revealed dual pathology: non-caseating granulomas alongside macrovesicular steatosis. Hispanics face unique risks, including 50% higher MASLD susceptibility (often at lower BMIs, potentially linked to PNPLA3 gene variants) and extrapulmonary sarcoidosis manifestations. The atypical ALP elevation signaled sarcoidosis-driven cholestasis, effectively managed with ursodiol, while MASLD required metabolic control. There can be a synergistic interaction with MASLD-related inflammation unmasking subclinical sarcoidosis, accelerating presentation, while sarcoidosis could exacerbate metabolic dysfunction (e.g., insulin dependence via potential pancreatic involvement). This dual etiology underscores the need for biopsy in Hispanic patients with metabolic risk factors and unexplained cholestasis, multidisciplinary monitoring to mitigate rapid progression risks, and awareness of genetic/environmental influences on disease phenotyping.
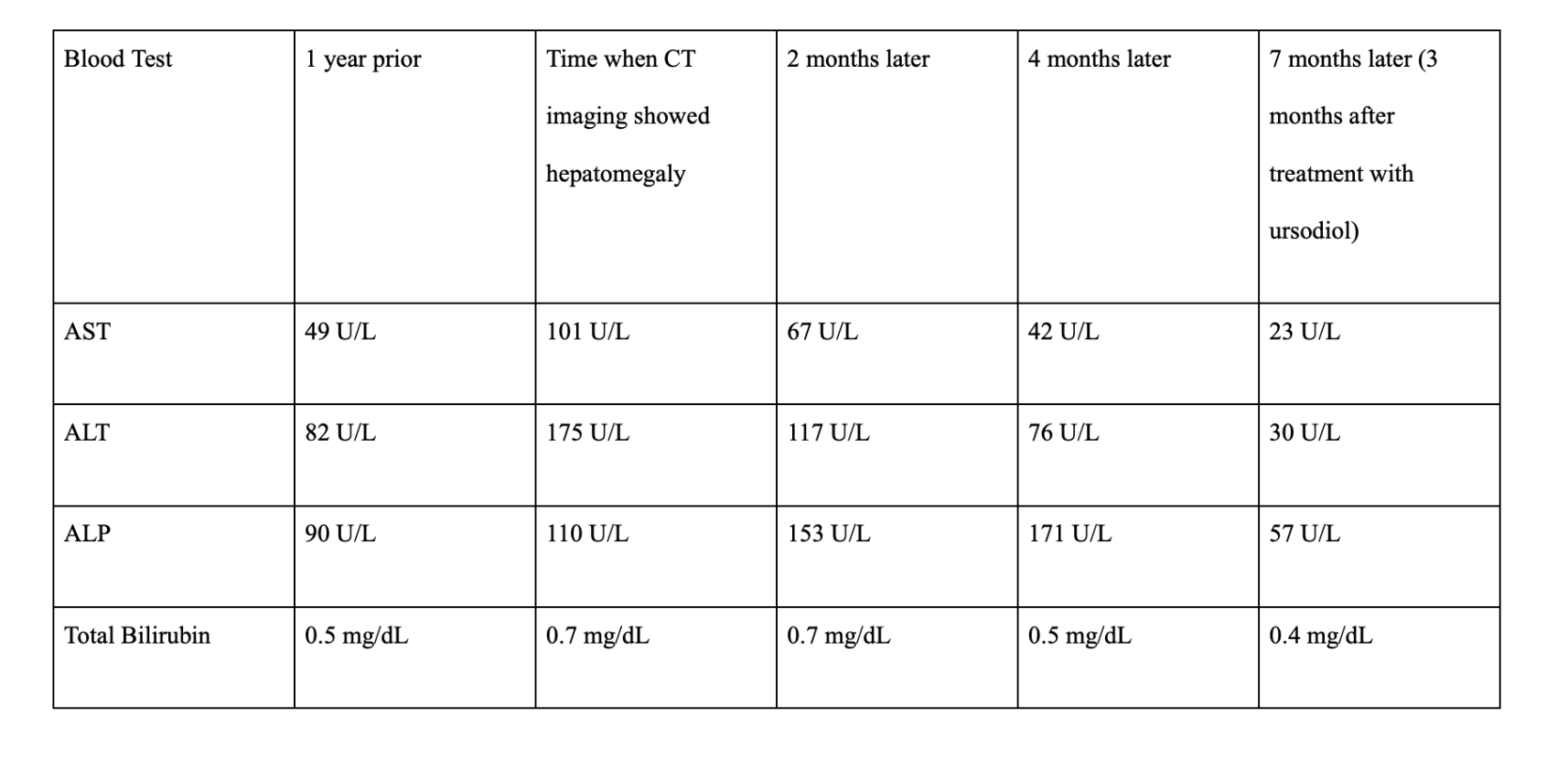
Figure: Table 1. Liver enzyme trends in the patient
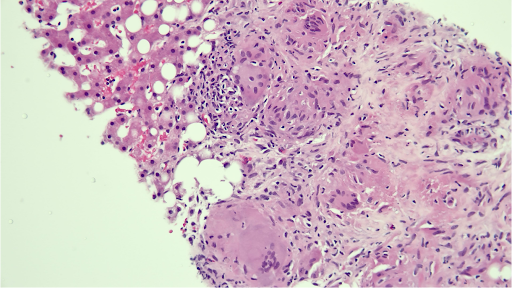
Figure: Figure 1: Liver core biopsy showed mild macrovesicular steatosis without ballooning degeneration of hepatocytes and a few portal tracts contain multiple coalescing epithelioid granulomas with fibrosis
Disclosures:
Archit Garg indicated no relevant financial relationships.
Rajesh Desai indicated no relevant financial relationships.
Louisa Recinos-Arenas indicated no relevant financial relationships.
Archit Garg, MD, Rajesh Desai, MD, Louisa Recinos-Arenas, MD. P1699 - The Double Burden: Unraveling the Complexity of Hepatic Sarcoidosis and MASLD in a Hispanic Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
