Sunday Poster Session
Category: Liver
P1685 - Hepatopulmonary Syndrome Ought to Be Considered in Patients With Chronic Liver Disease and Persistent Hypoxia
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Amit Rajkarnikar, MD (he/him/his)
Ochsner University Hospital & Clinics
Lafayette, LA
Presenting Author(s)
Amit Rajkarnikar, MD1, Jonathan Vignes, MD2
1Ochsner University Hospital & Clinics, Lafayette, LA; 2Ochsner Medical Center, Lafayette, LA
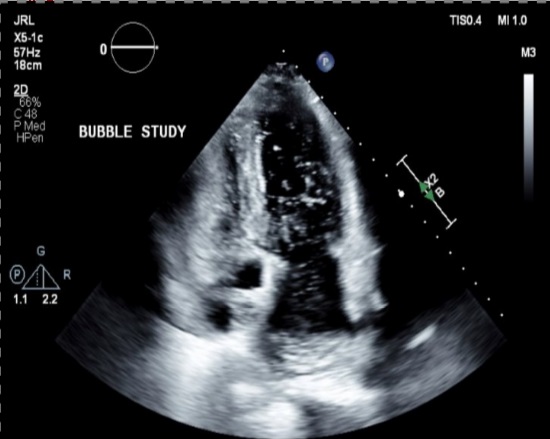
Introduction: Hepatopulmonary syndrome (HPS) is characterized by the triad of abnormal arterial oxygenation caused by intrapulmonary vascular dilatations (IPVDs) in the setting of liver disease or portal hypertension. Transthoracic contrast echocardiogram (TTCE) with agitated saline bubble study should be considered for patients with persistent hypoxia and chronic liver disease.
Case Description/
Methods:69-year-old female with NASH related cirrhosis, splenic and esophageal varices, chronic pancytopenia, T2DM, HLD, remote history of DVT presented with dyspnea on exertion and lightheadedness. Of note, the patient had two prior hospitalizations for atypical chest pain accompanied by shortness of breath in the span of 6 months.
1Ochsner University Hospital & Clinics, Lafayette, LA; 2Ochsner Medical Center, Lafayette, LA
Introduction: Hepatopulmonary syndrome (HPS) is characterized by the triad of abnormal arterial oxygenation caused by intrapulmonary vascular dilatations (IPVDs) in the setting of liver disease or portal hypertension. Transthoracic contrast echocardiogram (TTCE) with agitated saline bubble study should be considered for patients with persistent hypoxia and chronic liver disease.
Case Description/
Methods: