Sunday Poster Session
Category: Liver
P1679 - Improving Accuracy of Intake and Output Monitoring in Hospitalized Cirrhosis Patients: A Multidisciplinary Quality Improvement Initiative
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- JC
John Cooper, MD
University of Alabama at Birmingham Heersink School of Medicine
Birmingham, AL
Presenting Author(s)
John Cooper, MD1, Malcolm B. Chapman, MD, MBA1, Crystal Knox, MSN, RN2, Hollyn Davis, MSN, RN2, Laura Braddock, BSN, RN2, Katie Shields, BSN, RN2, Sujan Ravi, MD, MPH3
1University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 2University of Alabama at Birmingham Hospital, Birmingham, AL; 3Basil I. Hirschowitz Endoscopic Center of Excellence, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL
Introduction: Accurate intake and output (I&O) monitoring is essential in managing hospitalized patients, particularly those with cirrhosis-related complications such as volume overload and acute kidney injury. Despite its clinical importance, I&O charting is often unreliable due to system inefficiencies and personnel-related barriers. To address this, our inpatient hepatology Accountable Care Team (ACT) launched a multidisciplinary quality improvement initiative to identify obstacles and implement sustainable, protocol-driven interventions.
Methods: I&O data were extracted from electronic health records for all patients on the hepatology service in a designated inpatient unit with active strict I&O orders. Intake was considered accurate if documentation reflected recorded intake in the absence of an NPO order. Output was accurate if quantitative values were documented and no urine or diaper counts were missed.
The intervention followed three iterative Plan-Do-Study-Act (PDSA) cycles. In Cycle 1, house staff were educated on appropriate use of strict I&O orders, and nursing staff received training on the clinical relevance of accurate monitoring. Cycle 2 integrated I&O concerns into transition of care (ToC) rounds and introduced an escalation pathway for nursing challenges related to I&O charting. In Cycle 3, we implemented a standardized ToC script to prompt nursing input, launched real-time audits by nursing leadership, and introduced auto-generated I&O monitoring forms to support ongoing review.
Results: A total of 5,642 patient-days were analyzed from January 2024 to May 2025. Baseline I&O accuracy from January to April 2024 was 52.1%. Accuracy improved to 55.1% and 54.9% during PDSA Cycles 1 and 2, respectively. In Cycle 3, accuracy rose to 59.0%, representing a 13.3% relative improvement from baseline.
Discussion: A structured, multidisciplinary approach using iterative PDSA cycles led to measurable improvements in I&O documentation accuracy. The greatest gains occurred following implementation of standardized communication tools, leadership-driven audits, and automated support for nursing workflow. These results emphasize the value of combining education, protocols, and system-level enhancements to achieve sustainable quality improvement.
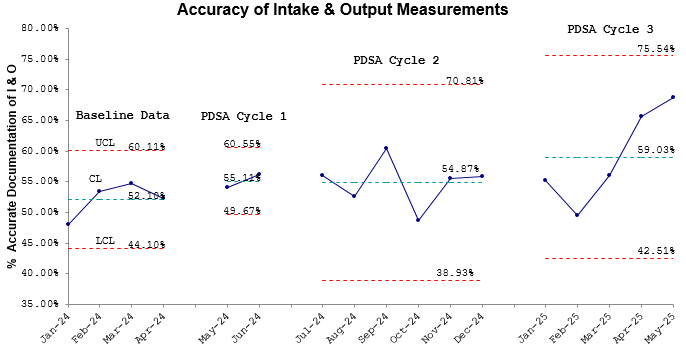
Figure: Figure 1
Disclosures:
John Cooper indicated no relevant financial relationships.
Malcolm Chapman indicated no relevant financial relationships.
Crystal Knox indicated no relevant financial relationships.
Hollyn Davis indicated no relevant financial relationships.
Laura Braddock indicated no relevant financial relationships.
Katie Shields indicated no relevant financial relationships.
Sujan Ravi indicated no relevant financial relationships.
John Cooper, MD1, Malcolm B. Chapman, MD, MBA1, Crystal Knox, MSN, RN2, Hollyn Davis, MSN, RN2, Laura Braddock, BSN, RN2, Katie Shields, BSN, RN2, Sujan Ravi, MD, MPH3. P1679 - Improving Accuracy of Intake and Output Monitoring in Hospitalized Cirrhosis Patients: A Multidisciplinary Quality Improvement Initiative, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 2University of Alabama at Birmingham Hospital, Birmingham, AL; 3Basil I. Hirschowitz Endoscopic Center of Excellence, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL
Introduction: Accurate intake and output (I&O) monitoring is essential in managing hospitalized patients, particularly those with cirrhosis-related complications such as volume overload and acute kidney injury. Despite its clinical importance, I&O charting is often unreliable due to system inefficiencies and personnel-related barriers. To address this, our inpatient hepatology Accountable Care Team (ACT) launched a multidisciplinary quality improvement initiative to identify obstacles and implement sustainable, protocol-driven interventions.
Methods: I&O data were extracted from electronic health records for all patients on the hepatology service in a designated inpatient unit with active strict I&O orders. Intake was considered accurate if documentation reflected recorded intake in the absence of an NPO order. Output was accurate if quantitative values were documented and no urine or diaper counts were missed.
The intervention followed three iterative Plan-Do-Study-Act (PDSA) cycles. In Cycle 1, house staff were educated on appropriate use of strict I&O orders, and nursing staff received training on the clinical relevance of accurate monitoring. Cycle 2 integrated I&O concerns into transition of care (ToC) rounds and introduced an escalation pathway for nursing challenges related to I&O charting. In Cycle 3, we implemented a standardized ToC script to prompt nursing input, launched real-time audits by nursing leadership, and introduced auto-generated I&O monitoring forms to support ongoing review.
Results: A total of 5,642 patient-days were analyzed from January 2024 to May 2025. Baseline I&O accuracy from January to April 2024 was 52.1%. Accuracy improved to 55.1% and 54.9% during PDSA Cycles 1 and 2, respectively. In Cycle 3, accuracy rose to 59.0%, representing a 13.3% relative improvement from baseline.
Discussion: A structured, multidisciplinary approach using iterative PDSA cycles led to measurable improvements in I&O documentation accuracy. The greatest gains occurred following implementation of standardized communication tools, leadership-driven audits, and automated support for nursing workflow. These results emphasize the value of combining education, protocols, and system-level enhancements to achieve sustainable quality improvement.
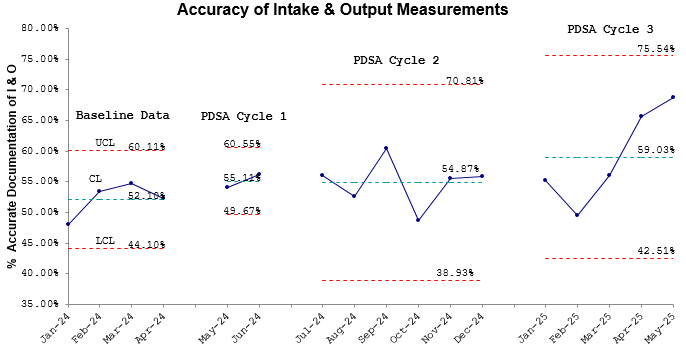
Figure: Figure 1
Disclosures:
John Cooper indicated no relevant financial relationships.
Malcolm Chapman indicated no relevant financial relationships.
Crystal Knox indicated no relevant financial relationships.
Hollyn Davis indicated no relevant financial relationships.
Laura Braddock indicated no relevant financial relationships.
Katie Shields indicated no relevant financial relationships.
Sujan Ravi indicated no relevant financial relationships.
John Cooper, MD1, Malcolm B. Chapman, MD, MBA1, Crystal Knox, MSN, RN2, Hollyn Davis, MSN, RN2, Laura Braddock, BSN, RN2, Katie Shields, BSN, RN2, Sujan Ravi, MD, MPH3. P1679 - Improving Accuracy of Intake and Output Monitoring in Hospitalized Cirrhosis Patients: A Multidisciplinary Quality Improvement Initiative, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

