Sunday Poster Session
Category: Liver
P1673 - Factors Associated With Recompensation in Cirrhosis Based on Baveno VII Criteria and Its Clinical Impact
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Kanachai Boonpiraks, MD (he/him/his)
University of Kansas Medical Center
Kansas City, KS
Presenting Author(s)
Kanachai Boonpiraks, MD1, Gunn Unchitti, MD2, Sith Siramolpiwat, MD2
1University of Kansas Medical Center, Kansas City, KS; 2Thammasat University, Khlong Luang, Pathum Thani, Thailand
Introduction: Cirrhosis is a major global health burden, responsible for approximately 1.47 million deaths annually. Recently, the Baveno VII consensus introduced the concept of recompensation, which represents a potentially reversible state in patients with decompensated cirrhosis. However, supporting evidence remains limited. In this study, we aimed to identify clinical and laboratory factors associated with recompensation in patients with decompensated cirrhosis.
Methods: This retrospective cohort study, conducted at a tertiary referral hospital, included patients with decompensated cirrhosis treated between January 1, 2018, and December 31, 2023. Decompensated cirrhosis was defined by the presence of one or more of the followings: (a) hepatic encephalopathy, (b) ascites, or (c) variceal bleeding. Demographics, clinical features, and laboratory results were collected. Patients were classified into three groups based on the Baveno VII consensus: recompensated, non-recompensated with stable disease, and non-recompensated with further decompensation. Patients were followed until death or the last follow-up date.
Results: Of the 196 patients included (mean age 61 years, 62% Child-Pugh class B, mean MELD score 12 ± 5.9), 53 (27%) achieved recompensation, 76 (38.7%) experienced further decompensation, and 73 (37.2%) remained stable without further decompensation. Compared to the non-recompensated group, patients with recompensation had significantly higher white blood cell counts (8.76x103 vs. 7.06x103/uL, p = 0.033), albumin levels (2.83 vs. 2.64 g/dL, p = 0.04) and alanine transaminase (51.08 vs. 30.29 U/L, p = 0.018). At the first decompensated event, the recompensated group had lower Child-Pugh score (7.70 + 1.64 vs. 8.41 + 1.5, p = 0.004), lower rates of ascites (57% vs. 83%, p < 0.001), less diuretic use (55% vs. 80%, p = 0.001), and higher beta-blocker use (60% vs. 38%, p = 0.009). Additionally, patients without ascites had significantly higher cumulative probabilities of recompensation over time (10.0% vs. 9.6% at 1 year and 66.5% vs. 35.1% at 3 years, p < 0.001).
Discussion: Our findings suggest that recompensation may be predicted by specific clinical and laboratory markers such as the Child-Pugh score and albumin levels. The association between beta-blocker use and recompensation highlights a potential implication for future therapeutic strategies. Validating these factors in future studies could improve prognostic accuracy and offer more individualized patient care.
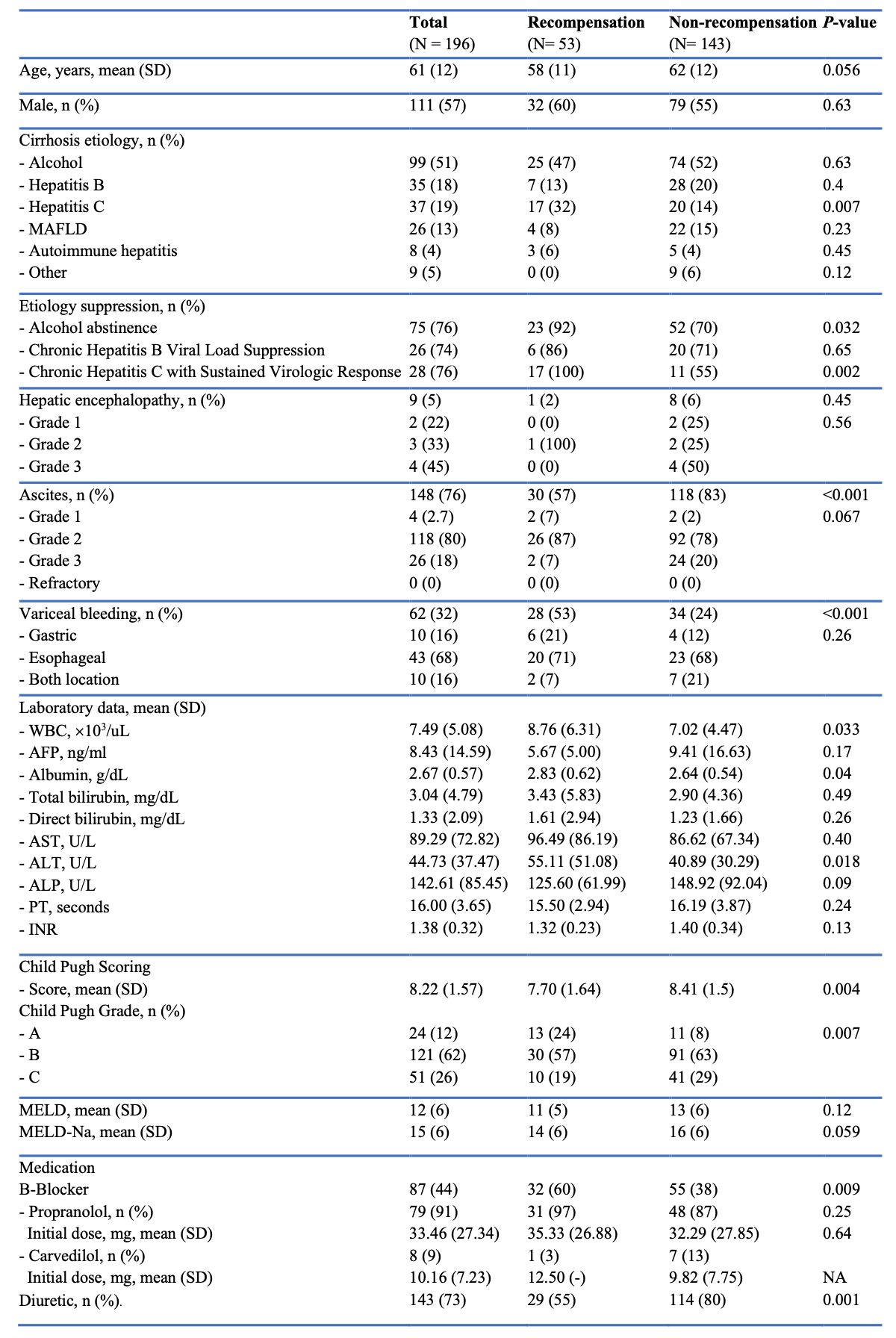
Figure: Comparison of Clinical and Laboratory Features Between Recompensated and Non-Recompensated Patients
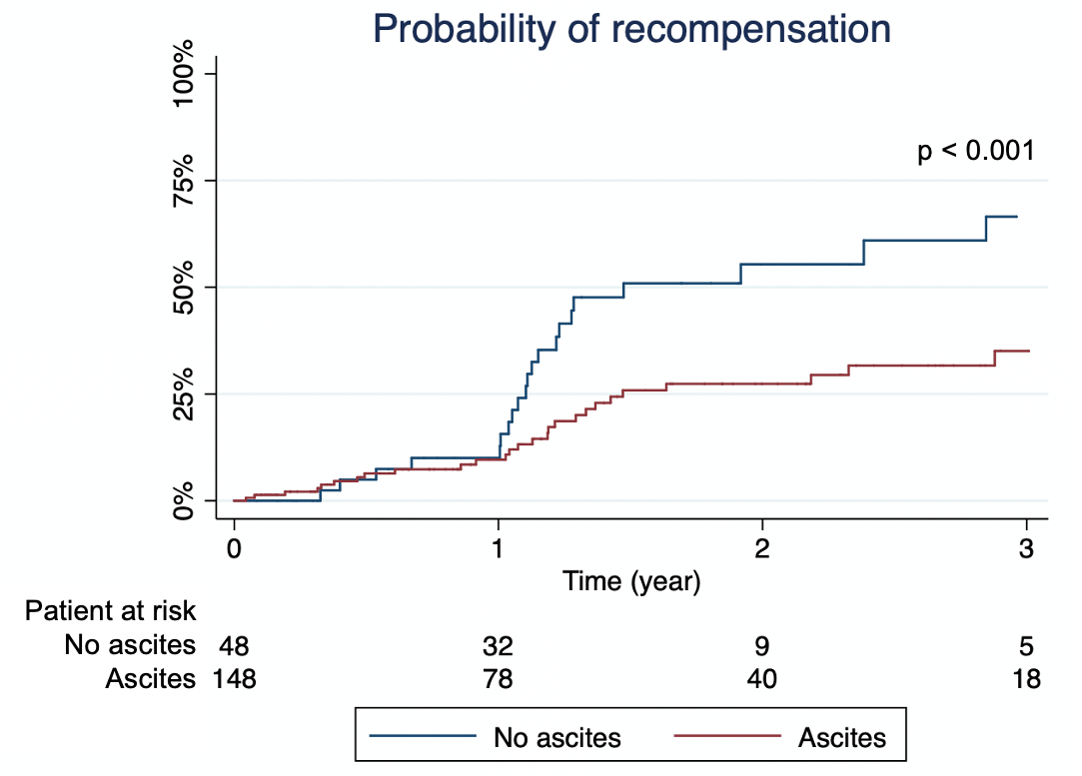
Figure: The Kaplan–Meier curves showing the cumulative probability of recompensation aaccording to ascites status
Disclosures:
Kanachai Boonpiraks indicated no relevant financial relationships.
Gunn Unchitti indicated no relevant financial relationships.
Sith Siramolpiwat indicated no relevant financial relationships.
Kanachai Boonpiraks, MD1, Gunn Unchitti, MD2, Sith Siramolpiwat, MD2. P1673 - Factors Associated With Recompensation in Cirrhosis Based on Baveno VII Criteria and Its Clinical Impact, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Kansas Medical Center, Kansas City, KS; 2Thammasat University, Khlong Luang, Pathum Thani, Thailand
Introduction: Cirrhosis is a major global health burden, responsible for approximately 1.47 million deaths annually. Recently, the Baveno VII consensus introduced the concept of recompensation, which represents a potentially reversible state in patients with decompensated cirrhosis. However, supporting evidence remains limited. In this study, we aimed to identify clinical and laboratory factors associated with recompensation in patients with decompensated cirrhosis.
Methods: This retrospective cohort study, conducted at a tertiary referral hospital, included patients with decompensated cirrhosis treated between January 1, 2018, and December 31, 2023. Decompensated cirrhosis was defined by the presence of one or more of the followings: (a) hepatic encephalopathy, (b) ascites, or (c) variceal bleeding. Demographics, clinical features, and laboratory results were collected. Patients were classified into three groups based on the Baveno VII consensus: recompensated, non-recompensated with stable disease, and non-recompensated with further decompensation. Patients were followed until death or the last follow-up date.
Results: Of the 196 patients included (mean age 61 years, 62% Child-Pugh class B, mean MELD score 12 ± 5.9), 53 (27%) achieved recompensation, 76 (38.7%) experienced further decompensation, and 73 (37.2%) remained stable without further decompensation. Compared to the non-recompensated group, patients with recompensation had significantly higher white blood cell counts (8.76x103 vs. 7.06x103/uL, p = 0.033), albumin levels (2.83 vs. 2.64 g/dL, p = 0.04) and alanine transaminase (51.08 vs. 30.29 U/L, p = 0.018). At the first decompensated event, the recompensated group had lower Child-Pugh score (7.70 + 1.64 vs. 8.41 + 1.5, p = 0.004), lower rates of ascites (57% vs. 83%, p < 0.001), less diuretic use (55% vs. 80%, p = 0.001), and higher beta-blocker use (60% vs. 38%, p = 0.009). Additionally, patients without ascites had significantly higher cumulative probabilities of recompensation over time (10.0% vs. 9.6% at 1 year and 66.5% vs. 35.1% at 3 years, p < 0.001).
Discussion: Our findings suggest that recompensation may be predicted by specific clinical and laboratory markers such as the Child-Pugh score and albumin levels. The association between beta-blocker use and recompensation highlights a potential implication for future therapeutic strategies. Validating these factors in future studies could improve prognostic accuracy and offer more individualized patient care.
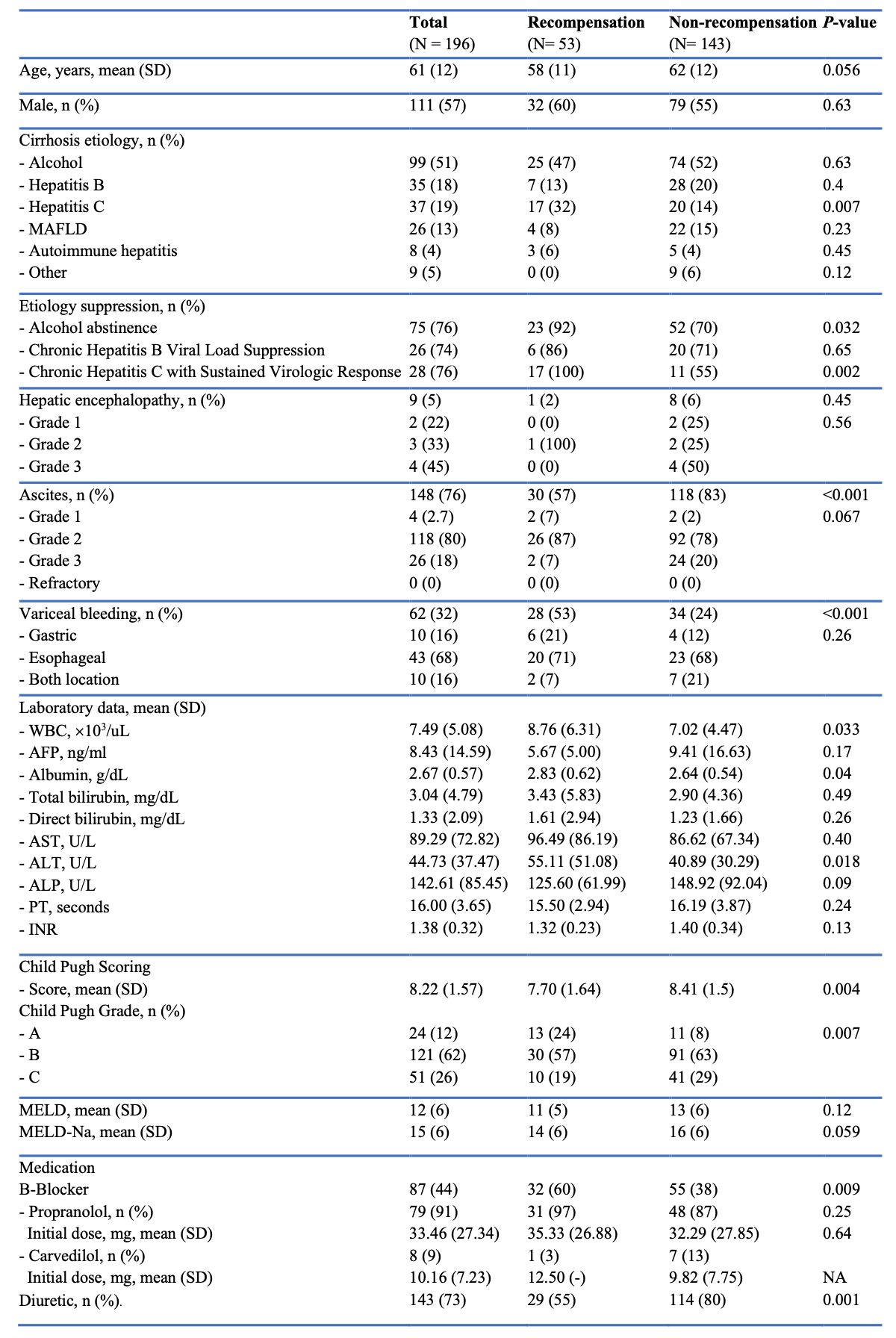
Figure: Comparison of Clinical and Laboratory Features Between Recompensated and Non-Recompensated Patients
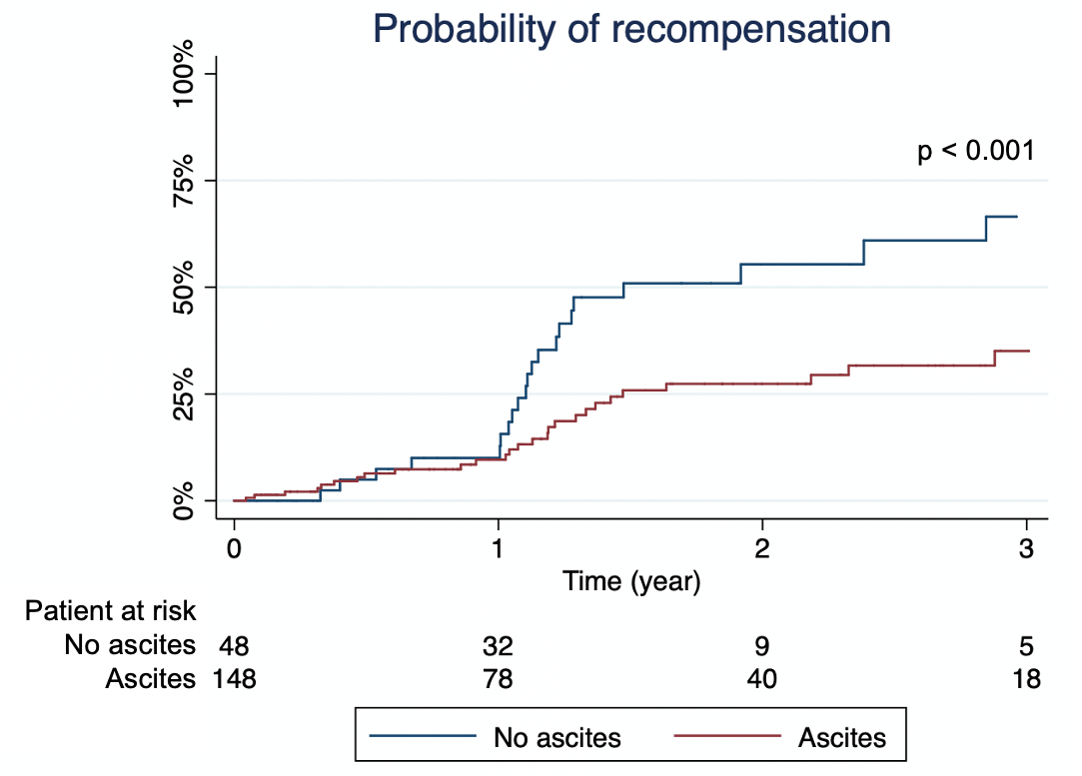
Figure: The Kaplan–Meier curves showing the cumulative probability of recompensation aaccording to ascites status
Disclosures:
Kanachai Boonpiraks indicated no relevant financial relationships.
Gunn Unchitti indicated no relevant financial relationships.
Sith Siramolpiwat indicated no relevant financial relationships.
Kanachai Boonpiraks, MD1, Gunn Unchitti, MD2, Sith Siramolpiwat, MD2. P1673 - Factors Associated With Recompensation in Cirrhosis Based on Baveno VII Criteria and Its Clinical Impact, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

