Sunday Poster Session
Category: Liver
P1672 - Evaluating FIB-4-Guided MASLD Care in a VA Spinal Cord Unit
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Ethan Shamsian, DO
Rutgers New Jersey Medical School
Newark, NJ
Presenting Author(s)
Ethan Shamsian, DO1, Joshua E. Pagán-Busigó, MD2, Dean Magat, MD1, Kranthi Mandava, MD1, Mahinaz Mohsen, MD1, Rohan Karkra, MBBS1, Muhammad Hassaan Arif Maan, MBBS1, Tomicka Mc Million, NP3, Jazmin Torres, RN3, Carol Gibson-Gill, MD3, Sima Vossough-Teehan, MD4
1Rutgers New Jersey Medical School, Newark, NJ; 2Rutgers New Jersey Medical School, Kearny, NJ; 3Rutgers New Jersey Medical School, East Orange, NJ; 4East Orange VA Hospital, East Orange, NJ
Introduction: MASLD is now the leading cause of cirrhosis in the United States. In recent years, tools such as the FIB-4 score and non-invasive tests have helped assess risk and identify patients with fibrosis, allowing for appropriate follow-up. Patients with spinal cord injuries or disorders (SCI/D) may be more vulnerable to steatotic liver disease due to a higher prevalence of metabolic dysfunction, underscoring the need for proper screening. The medical literature has yet to examine the patterns and adequacy of steatotic liver screening in this population. This study evaluates liver fibrosis risk assessment practices in patients with SCI/D at a single Veterans Affairs Medical Center (VA).
Methods: This single-center, retrospective chart review involved veterans with paraplegia and tetraplegia due to SCI or multiple sclerosis (MS) at the VA. A total of 100 patients (37% MS and 63% SCI) with an abdominal ultrasound-confirmed diagnosis of steatotic liver disease, randomly selected from 2020 to 2024, had their EMR reviewed. We analyzed patient demographics, clinical profiles, FIB-4 score documentation, and whether appropriate follow-up with non-invasive tests were completed based on FIB-4 risk stratification.
Results: Out of the 100 patients included in this study, the majority were males (94%) with a median age of 71.5 years (Table 1). Only 23% had a FIB-4 score documented in the electronic health record. Despite this, 39% of patients were found to fall into the intermediate (n = 37) or high-risk (n = 2) FIB-4 categories based on calculated scores. Transient elastography was completed in only 10% of the total cohort. Among the 39 intermediate/high-risk patients, just 4 underwent elastography.
Discussion: This quality analysis highlights a significant gap in MASLD risk stratification among veterans with SCI/D. Although 39% of patients had intermediate or high-risk FIB-4 scores, only 26% had the score documented, and just 10% underwent elastography, suggesting under-recognition of liver fibrosis risk. Given that several medications for SCI/D complications are processed through the liver, ensuring liver health is especially important in this population. In the presence of unrecognized fibrosis, these medications could accelerate liver injury or complicate management. As patients with SCI/D are living longer due to medical advances, future efforts should focus on raising awareness of MASLD in this population and developing tailored clinical pathways to ensure timely risk stratification and management.
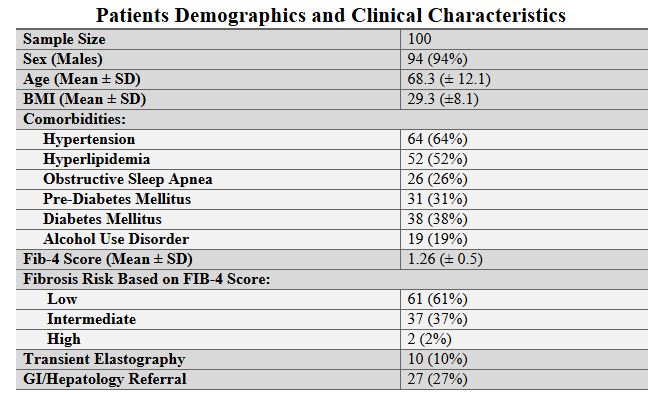
Figure: Patient Demographics and Clinical Characteristics
Disclosures:
Ethan Shamsian indicated no relevant financial relationships.
Joshua Pagán-Busigó indicated no relevant financial relationships.
Dean Magat indicated no relevant financial relationships.
Kranthi Mandava indicated no relevant financial relationships.
Mahinaz Mohsen indicated no relevant financial relationships.
Rohan Karkra indicated no relevant financial relationships.
Muhammad Hassaan Arif Maan indicated no relevant financial relationships.
Tomicka Mc Million indicated no relevant financial relationships.
Jazmin Torres indicated no relevant financial relationships.
Carol Gibson-Gill indicated no relevant financial relationships.
Sima Vossough-Teehan indicated no relevant financial relationships.
Ethan Shamsian, DO1, Joshua E. Pagán-Busigó, MD2, Dean Magat, MD1, Kranthi Mandava, MD1, Mahinaz Mohsen, MD1, Rohan Karkra, MBBS1, Muhammad Hassaan Arif Maan, MBBS1, Tomicka Mc Million, NP3, Jazmin Torres, RN3, Carol Gibson-Gill, MD3, Sima Vossough-Teehan, MD4. P1672 - Evaluating FIB-4-Guided MASLD Care in a VA Spinal Cord Unit, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rutgers New Jersey Medical School, Newark, NJ; 2Rutgers New Jersey Medical School, Kearny, NJ; 3Rutgers New Jersey Medical School, East Orange, NJ; 4East Orange VA Hospital, East Orange, NJ
Introduction: MASLD is now the leading cause of cirrhosis in the United States. In recent years, tools such as the FIB-4 score and non-invasive tests have helped assess risk and identify patients with fibrosis, allowing for appropriate follow-up. Patients with spinal cord injuries or disorders (SCI/D) may be more vulnerable to steatotic liver disease due to a higher prevalence of metabolic dysfunction, underscoring the need for proper screening. The medical literature has yet to examine the patterns and adequacy of steatotic liver screening in this population. This study evaluates liver fibrosis risk assessment practices in patients with SCI/D at a single Veterans Affairs Medical Center (VA).
Methods: This single-center, retrospective chart review involved veterans with paraplegia and tetraplegia due to SCI or multiple sclerosis (MS) at the VA. A total of 100 patients (37% MS and 63% SCI) with an abdominal ultrasound-confirmed diagnosis of steatotic liver disease, randomly selected from 2020 to 2024, had their EMR reviewed. We analyzed patient demographics, clinical profiles, FIB-4 score documentation, and whether appropriate follow-up with non-invasive tests were completed based on FIB-4 risk stratification.
Results: Out of the 100 patients included in this study, the majority were males (94%) with a median age of 71.5 years (Table 1). Only 23% had a FIB-4 score documented in the electronic health record. Despite this, 39% of patients were found to fall into the intermediate (n = 37) or high-risk (n = 2) FIB-4 categories based on calculated scores. Transient elastography was completed in only 10% of the total cohort. Among the 39 intermediate/high-risk patients, just 4 underwent elastography.
Discussion: This quality analysis highlights a significant gap in MASLD risk stratification among veterans with SCI/D. Although 39% of patients had intermediate or high-risk FIB-4 scores, only 26% had the score documented, and just 10% underwent elastography, suggesting under-recognition of liver fibrosis risk. Given that several medications for SCI/D complications are processed through the liver, ensuring liver health is especially important in this population. In the presence of unrecognized fibrosis, these medications could accelerate liver injury or complicate management. As patients with SCI/D are living longer due to medical advances, future efforts should focus on raising awareness of MASLD in this population and developing tailored clinical pathways to ensure timely risk stratification and management.
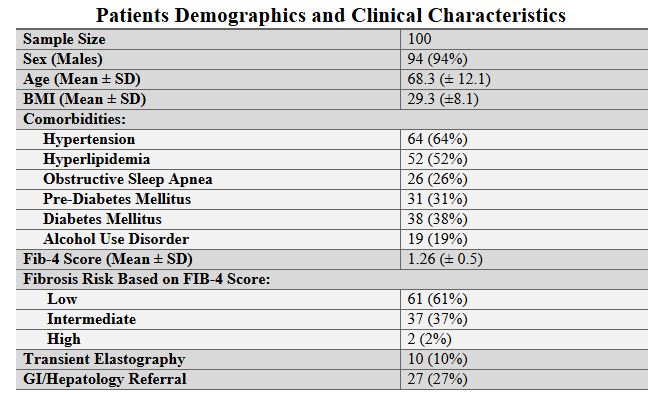
Figure: Patient Demographics and Clinical Characteristics
Disclosures:
Ethan Shamsian indicated no relevant financial relationships.
Joshua Pagán-Busigó indicated no relevant financial relationships.
Dean Magat indicated no relevant financial relationships.
Kranthi Mandava indicated no relevant financial relationships.
Mahinaz Mohsen indicated no relevant financial relationships.
Rohan Karkra indicated no relevant financial relationships.
Muhammad Hassaan Arif Maan indicated no relevant financial relationships.
Tomicka Mc Million indicated no relevant financial relationships.
Jazmin Torres indicated no relevant financial relationships.
Carol Gibson-Gill indicated no relevant financial relationships.
Sima Vossough-Teehan indicated no relevant financial relationships.
Ethan Shamsian, DO1, Joshua E. Pagán-Busigó, MD2, Dean Magat, MD1, Kranthi Mandava, MD1, Mahinaz Mohsen, MD1, Rohan Karkra, MBBS1, Muhammad Hassaan Arif Maan, MBBS1, Tomicka Mc Million, NP3, Jazmin Torres, RN3, Carol Gibson-Gill, MD3, Sima Vossough-Teehan, MD4. P1672 - Evaluating FIB-4-Guided MASLD Care in a VA Spinal Cord Unit, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

