Sunday Poster Session
Category: Liver
P1667 - The Hidden Cost of Inequity: Education, Language, and Insurance Status Shape Cirrhosis Outcomes
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Dilman Natt, MD
Nassau University Medical Center
East Meadow, New York
Presenting Author(s)
Dilman Natt, MD, Rajmohan Rammohan, MD, Sai Reshma Magam, MD, Leeza E. Pannikodu, MD, Sindhuja Giridharan, MD, Achal Patel, MD, Amilcar Guaschino, MD, Amina Zafar, MD, Venkata Panchagnula, MD, Sri Harsha Boppana, MD, Wing Hang Lau, DO, Cesar Orlando Ortiz Bernard, MD, Paul Mustacchia, MD
Nassau University Medical Center, East Meadow, NY
Introduction: Cirrhosis, characterized by high mortality and frequent hospitalizations, necessitates complex medication regimens to manage liver disease and associated complications. Non-adherence to these treatments, often due to side effects or changes in routine, leads to preventable readmissions. This study utilizes the Healthcare Cost and Utilization Project (HCUP) National Database to examine the factors influencing hospital readmissions. We aim to identify key predictors of readmission and evaluate the impact of socio-economic factors on patient outcomes.
Methods: In our study, we conducted a retrospective analysis using the HCUP National Database, covering 2019 to 2024. We identified the cirrhotic patient population using specific ICD codes. Data collected included information on comorbidities, insurance status, educational level, and hospital admissions. we utilized area under the receiver operating characteristic curve (AUROC) and relationship mapping techniques to investigate the risk and predictive accuracy of interacting variables within the logistic regression model.
Results: Using HCUP data from 2019 to 2024 (n=2,858,576), we identified 78,546 cirrhotic patients and found that low education (p=0.012), inadequate insurance (p=0.023), and English as a second language (p=0.011) significantly increased 30-day readmission rates. Language barriers (HR=0.346, p=0.043) and low educational status (HR=0.756, p=0.025) were also associated with delayed recovery. AUROC values for education (0.645, p< 0.01) and insurance (0.554, p< 0.01) supported their predictive value. These findings highlight the need for targeted interventions addressing socio-economic and linguistic barriers in cirrhotic patient care.
Discussion: The findings from this comprehensive analysis of the HCUP National Database highlight significant socio-economic factors, such as low education level, inadequate insurance, and language barriers, that contribute to higher readmission rates among cirrhotic patients. The statistical significance of these factors suggests that tailored interventions focusing on education and language support could mitigate these risks. This study underscores the necessity for healthcare systems to integrate socio-economic considerations into the management plans for patients with cirrhosis to reduce preventable hospitalizations and improve overall patient outcomes.
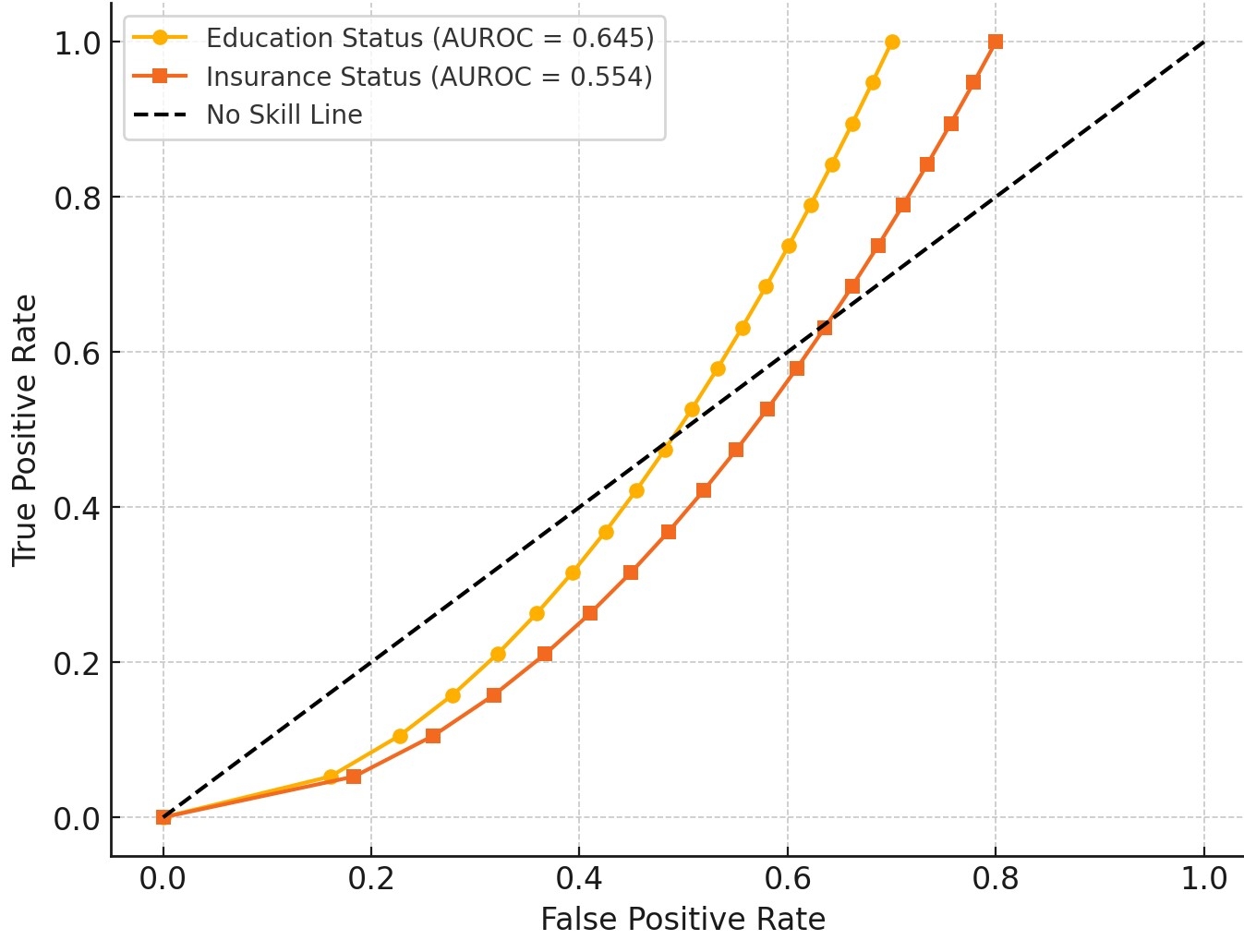
Figure: Social determinants
Disclosures:
Dilman Natt indicated no relevant financial relationships.
Rajmohan Rammohan indicated no relevant financial relationships.
Sai Reshma Magam indicated no relevant financial relationships.
Leeza Pannikodu indicated no relevant financial relationships.
Sindhuja Giridharan indicated no relevant financial relationships.
Achal Patel indicated no relevant financial relationships.
Amilcar Guaschino indicated no relevant financial relationships.
Amina Zafar indicated no relevant financial relationships.
Venkata Panchagnula indicated no relevant financial relationships.
Sri Harsha Boppana indicated no relevant financial relationships.
Wing Hang Lau indicated no relevant financial relationships.
Cesar Orlando Ortiz Bernard indicated no relevant financial relationships.
Paul Mustacchia indicated no relevant financial relationships.
Dilman Natt, MD, Rajmohan Rammohan, MD, Sai Reshma Magam, MD, Leeza E. Pannikodu, MD, Sindhuja Giridharan, MD, Achal Patel, MD, Amilcar Guaschino, MD, Amina Zafar, MD, Venkata Panchagnula, MD, Sri Harsha Boppana, MD, Wing Hang Lau, DO, Cesar Orlando Ortiz Bernard, MD, Paul Mustacchia, MD. P1667 - The Hidden Cost of Inequity: Education, Language, and Insurance Status Shape Cirrhosis Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Nassau University Medical Center, East Meadow, NY
Introduction: Cirrhosis, characterized by high mortality and frequent hospitalizations, necessitates complex medication regimens to manage liver disease and associated complications. Non-adherence to these treatments, often due to side effects or changes in routine, leads to preventable readmissions. This study utilizes the Healthcare Cost and Utilization Project (HCUP) National Database to examine the factors influencing hospital readmissions. We aim to identify key predictors of readmission and evaluate the impact of socio-economic factors on patient outcomes.
Methods: In our study, we conducted a retrospective analysis using the HCUP National Database, covering 2019 to 2024. We identified the cirrhotic patient population using specific ICD codes. Data collected included information on comorbidities, insurance status, educational level, and hospital admissions. we utilized area under the receiver operating characteristic curve (AUROC) and relationship mapping techniques to investigate the risk and predictive accuracy of interacting variables within the logistic regression model.
Results: Using HCUP data from 2019 to 2024 (n=2,858,576), we identified 78,546 cirrhotic patients and found that low education (p=0.012), inadequate insurance (p=0.023), and English as a second language (p=0.011) significantly increased 30-day readmission rates. Language barriers (HR=0.346, p=0.043) and low educational status (HR=0.756, p=0.025) were also associated with delayed recovery. AUROC values for education (0.645, p< 0.01) and insurance (0.554, p< 0.01) supported their predictive value. These findings highlight the need for targeted interventions addressing socio-economic and linguistic barriers in cirrhotic patient care.
Discussion: The findings from this comprehensive analysis of the HCUP National Database highlight significant socio-economic factors, such as low education level, inadequate insurance, and language barriers, that contribute to higher readmission rates among cirrhotic patients. The statistical significance of these factors suggests that tailored interventions focusing on education and language support could mitigate these risks. This study underscores the necessity for healthcare systems to integrate socio-economic considerations into the management plans for patients with cirrhosis to reduce preventable hospitalizations and improve overall patient outcomes.
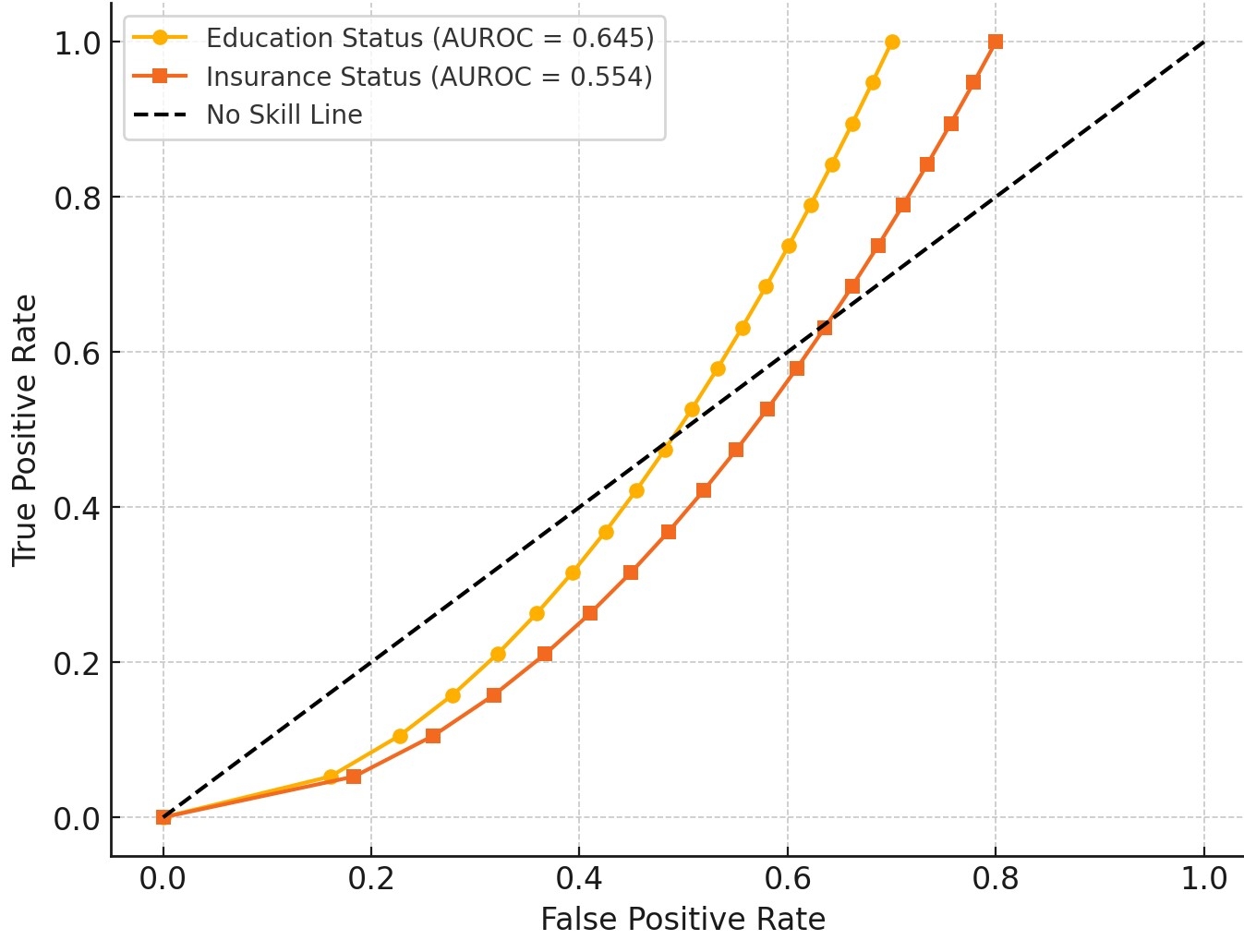
Figure: Social determinants
Disclosures:
Dilman Natt indicated no relevant financial relationships.
Rajmohan Rammohan indicated no relevant financial relationships.
Sai Reshma Magam indicated no relevant financial relationships.
Leeza Pannikodu indicated no relevant financial relationships.
Sindhuja Giridharan indicated no relevant financial relationships.
Achal Patel indicated no relevant financial relationships.
Amilcar Guaschino indicated no relevant financial relationships.
Amina Zafar indicated no relevant financial relationships.
Venkata Panchagnula indicated no relevant financial relationships.
Sri Harsha Boppana indicated no relevant financial relationships.
Wing Hang Lau indicated no relevant financial relationships.
Cesar Orlando Ortiz Bernard indicated no relevant financial relationships.
Paul Mustacchia indicated no relevant financial relationships.
Dilman Natt, MD, Rajmohan Rammohan, MD, Sai Reshma Magam, MD, Leeza E. Pannikodu, MD, Sindhuja Giridharan, MD, Achal Patel, MD, Amilcar Guaschino, MD, Amina Zafar, MD, Venkata Panchagnula, MD, Sri Harsha Boppana, MD, Wing Hang Lau, DO, Cesar Orlando Ortiz Bernard, MD, Paul Mustacchia, MD. P1667 - The Hidden Cost of Inequity: Education, Language, and Insurance Status Shape Cirrhosis Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
