Sunday Poster Session
Category: Liver
P1660 - Impact of Nosocomial Infections in Post-Liver Transplantation Patients: A National Inpatient Sample Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Vera Hapshy, DO
Hackensack Meridian JSUMC
Neptune City, NJ
Presenting Author(s)
Vera Hapshy, DO1, Idan Grossman, MD2, Karolina Kaczmarczyk, MD, MPH3, Harshavardhan Sanekommu, MD4, Mohammad Hossain, MD4, Avik Sarkar, MD2, Haroon Shahid, MD2, Lee Peng, MD, PhD4
1Hackensack Meridian JSUMC, Neptune City, NJ; 2Jersey Shore University Medical Center, Neptune, NJ; 3Hackensack Meridian Jersey Shore University Medical Center, Neptune City, NJ; 4Hackensack Meridian Health, Neptune, NJ
Introduction: Despite advancements in liver transplantation, infections remain a leading cause of mortality and graft loss. This impact can be mitigated through preventive strategies, early diagnosis, and appropriate treatment. This study aims to investigate nosocomial infections (NI) in post-liver transplantation patients.
Methods: A retrospective analysis was conducted utilizing data from the National Inpatient Sample (NIS) database spanning the years 2016 to 2019. Liver transplant recipients were identified using the ICD-10 procedure codes (0FY00Z0 and 0FY00Z1), and the analysis was restricted to patients who had a length of stay greater than three days. NI was defined as the presence of at least one of the following conditions: catheter-associated urinary tract infections, central line-associated bloodstream infections, ventilator-associated pneumonia, Clostridioides difficile infection, and surgical site infections. The primary outcome of interest was in-hospital mortality, and secondary outcomes included LOS and total hospitalization charges.
Results: A total of 21,465 patients underwent liver transplantation, of whom 440 (2.0%) developed NI. Patients with NI exhibited higher rates of congestive heart failure, cardiac arrhythmias, uncomplicated hypertension, and fluid and electrolyte disorders. The presence of NI was associated with significantly higher in-hospital mortality (15% vs. 2.9%, Adjusted OR 3.28, CI: 1.39–7.74), longer LOS (43.6 vs. 15.3 days), and greater hospital costs ($303,478.4 vs. $129,137.3). Among infection types, VAP had the highest mortality rate at 60% (30 of 50 patients, AOR 29.6, CI: 5.24–169). CDI and SSI were associated with mortality rates of 8.6% and 25%, respectively, but these were not statistically significant. Risk factors for developing NI included congestive heart failure (OR 2.08, CI: 1.03–4.23) and fluid and electrolyte disorders (OR 2.4, CI: 1.24–4.62).
Discussion: NI significantly increases in-hospital mortality, prolongs hospital stays, and escalates healthcare costs in post-liver transplantation patients. Infections such as VAP carry especially high mortality risks. These findings emphasize the urgent need for effective prevention, early detection, and targeted intervention strategies.
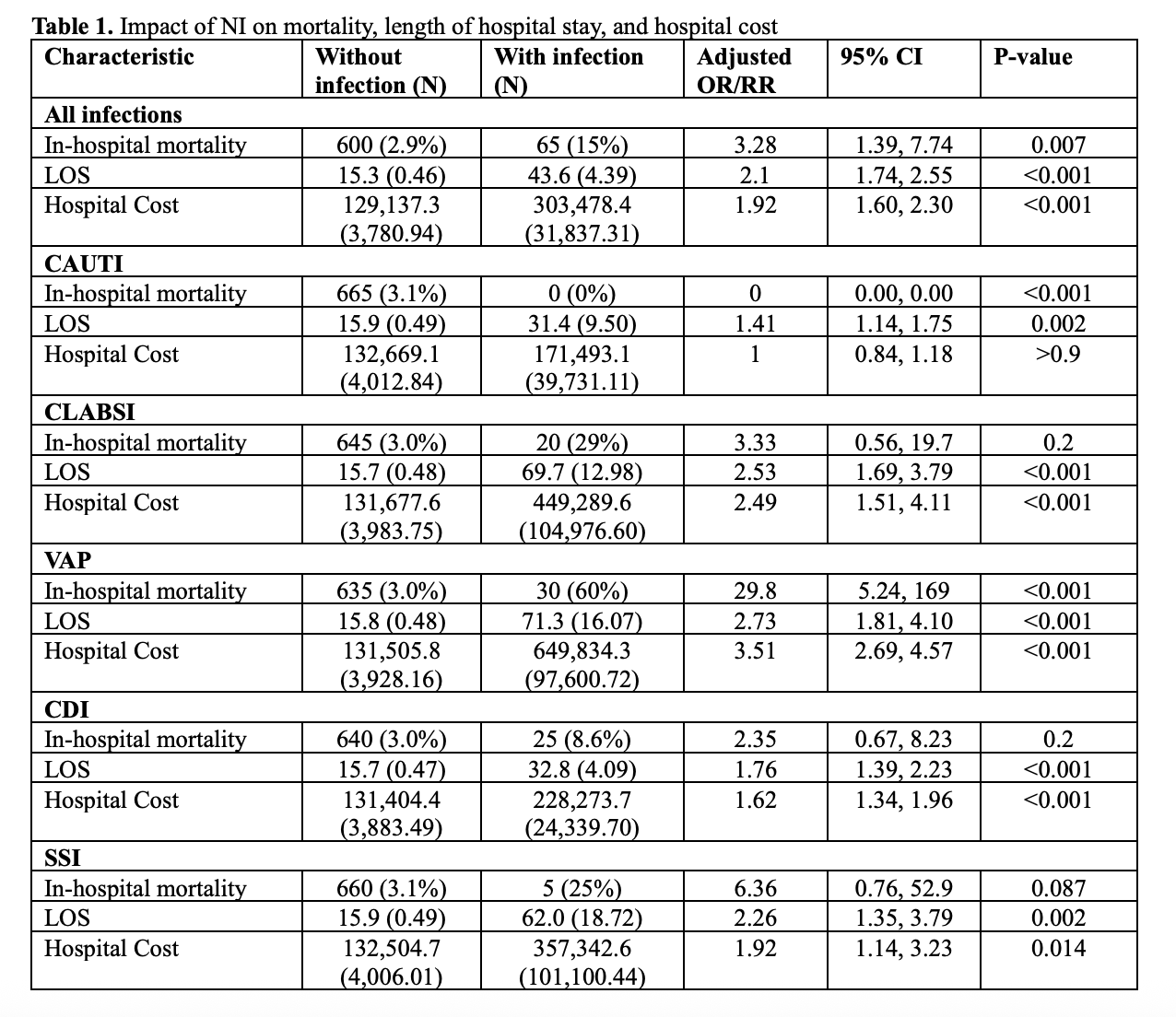
Figure: Table 1. Impact of NI on mortality, length of hospital stay, and hospital cost
Disclosures:
Vera Hapshy indicated no relevant financial relationships.
Idan Grossman indicated no relevant financial relationships.
Karolina Kaczmarczyk indicated no relevant financial relationships.
Harshavardhan Sanekommu indicated no relevant financial relationships.
Mohammad Hossain indicated no relevant financial relationships.
Avik Sarkar indicated no relevant financial relationships.
Haroon Shahid indicated no relevant financial relationships.
Lee Peng indicated no relevant financial relationships.
Vera Hapshy, DO1, Idan Grossman, MD2, Karolina Kaczmarczyk, MD, MPH3, Harshavardhan Sanekommu, MD4, Mohammad Hossain, MD4, Avik Sarkar, MD2, Haroon Shahid, MD2, Lee Peng, MD, PhD4. P1660 - Impact of Nosocomial Infections in Post-Liver Transplantation Patients: A National Inpatient Sample Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Hackensack Meridian JSUMC, Neptune City, NJ; 2Jersey Shore University Medical Center, Neptune, NJ; 3Hackensack Meridian Jersey Shore University Medical Center, Neptune City, NJ; 4Hackensack Meridian Health, Neptune, NJ
Introduction: Despite advancements in liver transplantation, infections remain a leading cause of mortality and graft loss. This impact can be mitigated through preventive strategies, early diagnosis, and appropriate treatment. This study aims to investigate nosocomial infections (NI) in post-liver transplantation patients.
Methods: A retrospective analysis was conducted utilizing data from the National Inpatient Sample (NIS) database spanning the years 2016 to 2019. Liver transplant recipients were identified using the ICD-10 procedure codes (0FY00Z0 and 0FY00Z1), and the analysis was restricted to patients who had a length of stay greater than three days. NI was defined as the presence of at least one of the following conditions: catheter-associated urinary tract infections, central line-associated bloodstream infections, ventilator-associated pneumonia, Clostridioides difficile infection, and surgical site infections. The primary outcome of interest was in-hospital mortality, and secondary outcomes included LOS and total hospitalization charges.
Results: A total of 21,465 patients underwent liver transplantation, of whom 440 (2.0%) developed NI. Patients with NI exhibited higher rates of congestive heart failure, cardiac arrhythmias, uncomplicated hypertension, and fluid and electrolyte disorders. The presence of NI was associated with significantly higher in-hospital mortality (15% vs. 2.9%, Adjusted OR 3.28, CI: 1.39–7.74), longer LOS (43.6 vs. 15.3 days), and greater hospital costs ($303,478.4 vs. $129,137.3). Among infection types, VAP had the highest mortality rate at 60% (30 of 50 patients, AOR 29.6, CI: 5.24–169). CDI and SSI were associated with mortality rates of 8.6% and 25%, respectively, but these were not statistically significant. Risk factors for developing NI included congestive heart failure (OR 2.08, CI: 1.03–4.23) and fluid and electrolyte disorders (OR 2.4, CI: 1.24–4.62).
Discussion: NI significantly increases in-hospital mortality, prolongs hospital stays, and escalates healthcare costs in post-liver transplantation patients. Infections such as VAP carry especially high mortality risks. These findings emphasize the urgent need for effective prevention, early detection, and targeted intervention strategies.
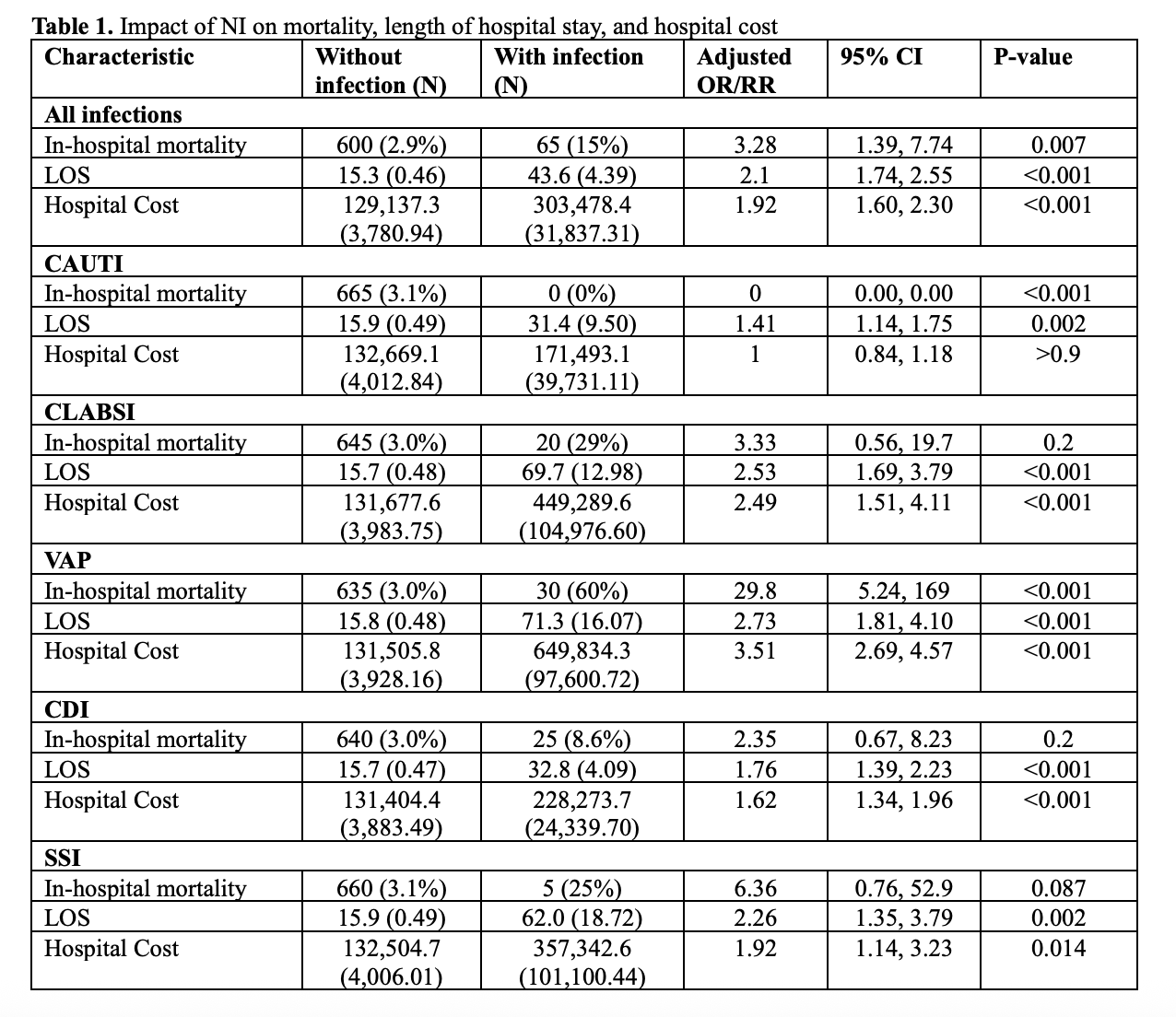
Figure: Table 1. Impact of NI on mortality, length of hospital stay, and hospital cost
Disclosures:
Vera Hapshy indicated no relevant financial relationships.
Idan Grossman indicated no relevant financial relationships.
Karolina Kaczmarczyk indicated no relevant financial relationships.
Harshavardhan Sanekommu indicated no relevant financial relationships.
Mohammad Hossain indicated no relevant financial relationships.
Avik Sarkar indicated no relevant financial relationships.
Haroon Shahid indicated no relevant financial relationships.
Lee Peng indicated no relevant financial relationships.
Vera Hapshy, DO1, Idan Grossman, MD2, Karolina Kaczmarczyk, MD, MPH3, Harshavardhan Sanekommu, MD4, Mohammad Hossain, MD4, Avik Sarkar, MD2, Haroon Shahid, MD2, Lee Peng, MD, PhD4. P1660 - Impact of Nosocomial Infections in Post-Liver Transplantation Patients: A National Inpatient Sample Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

